Osteoarthritis (OA) and soft tissue pathology (STP) are the most frequent causes of osteoarticular disease. According to the EPISER1 study, the prevalence of OA in Spain stands at 29.35%. Inflammation plays an important role in these diseases, as the release of cytokines in the synovial fluid triggers a vicious circle of inflammation-destruction, causing pain, rigidity and patient disability.2,3
Current therapies include conservative treatments which aim to control pain, although these treatments often fail and invasive surgical procedures are required that are not free of risks.4 Due to this the use of low-dose radiotherapy (RT) has emerged once again in recent years to control pain in these diseases.
The aim of this study was to evaluate the efficacy of RT in improving pain measured on the analogue visual scale (VAS-pain). The patients were classified in the OA group if they had at least one of the following characteristics as shown by simple X-ray imaging: the presence of osteophytes, subchondral sclerosis, asymmetrical reduction of the space in a joint or subchondral cysts. In the enthesitis, synovitis or tenosynovitis group they were included if they fulfilled the corresponding ultrasound scan definitions according to the 2005 Outcome Measures in Rheumatology (OMERACT) guides.5 All of the patients were diagnosed OA or STP. No patient had autoimmune disease or associated inflammatory rheumatic disease.
A longitudinal study was undertaken of 114 patients (96 women and 18 men; average age 64.4±11.1 years and average VAS-basal pain 8.26±1.56) included from 2015 to 2017. Diseases were grouped into 5 categories: enthesitis (N=29) including trochanteritis, fasciitis plantar, lateral epicondylitis, peripheral OA (N=67) including shoulder OA, hip OA, foot OA, knee OA, hand OA and axial lumbar OA (N=8), proximal interfalangeal synovitis of the hands (N=5) and tendinitis (N=5) including hand flexor tenosynovitis and posterior tibial tenosynovitis.
The main outcome of the study was the improvement of the VAS-pain ≥50%. All of the patients received initial RT treatment at a dose of 6Gy/6 sessions/during 2 weeks. After a period of 6–8 weeks the patients were evaluated again, and those who had not responded received another cycle of RT identical to the previous one. Fifty three patients attained a therapeutic response in the first cycle and 40 received a second cycle of treatment and 27 of them responded. The total percentage of patients who responded in both treatments amounted to 70.1%. The average reduction in the VAS after the first treatment respecting the basal level was 2.89 points (IC 95%: 2.29–3.31; P<.001), while the reduction after both treatments was 3.67 points (IC 95%: 2.82–4.62; P<.0001). Respecting the type of disease, the cases of enthesitis responded better than axial OA (P=.046) and peripheral OA (P=.019). According to location, those which responded to the treatment in a statistically significant way were hand OA, shoulder OA, knee OA, trochanteritis, posterior tibial tendinitis and fasciitis plantar. The other diseases could not be evaluated due to the small size of the sample. No patient suffered adverse effects.
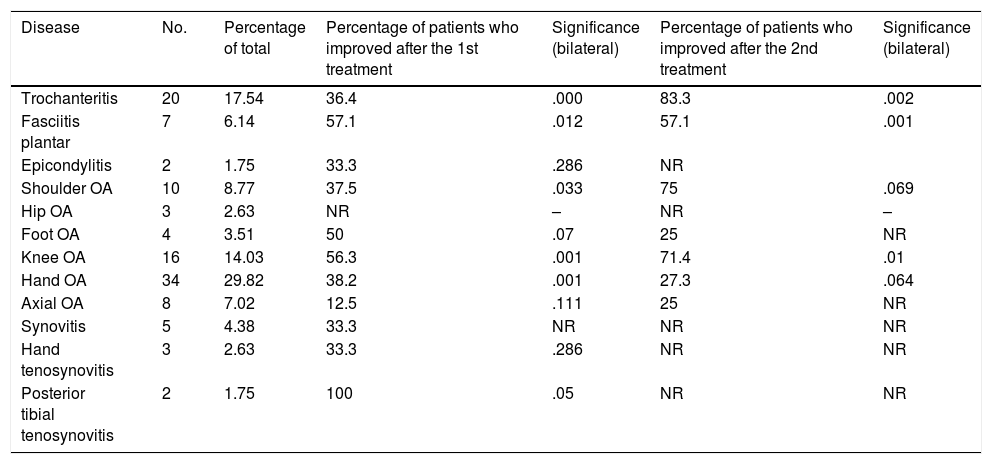
Table 1 shows the size of the sample and percentage respecting the total of each disease, as well as statistical significance using the paired samples test after the first and second treatment in comparison with the basal situation.
Percentage of the total of each disease and percentage of patients who experienced a response to the first and second treatment.
| Disease | No. | Percentage of total | Percentage of patients who improved after the 1st treatment | Significance (bilateral) | Percentage of patients who improved after the 2nd treatment | Significance (bilateral) |
|---|---|---|---|---|---|---|
| Trochanteritis | 20 | 17.54 | 36.4 | .000 | 83.3 | .002 |
| Fasciitis plantar | 7 | 6.14 | 57.1 | .012 | 57.1 | .001 |
| Epicondylitis | 2 | 1.75 | 33.3 | .286 | NR | |
| Shoulder OA | 10 | 8.77 | 37.5 | .033 | 75 | .069 |
| Hip OA | 3 | 2.63 | NR | – | NR | – |
| Foot OA | 4 | 3.51 | 50 | .07 | 25 | NR |
| Knee OA | 16 | 14.03 | 56.3 | .001 | 71.4 | .01 |
| Hand OA | 34 | 29.82 | 38.2 | .001 | 27.3 | .064 |
| Axial OA | 8 | 7.02 | 12.5 | .111 | 25 | NR |
| Synovitis | 5 | 4.38 | 33.3 | NR | NR | NR |
| Hand tenosynovitis | 3 | 2.63 | 33.3 | .286 | NR | NR |
| Posterior tibial tenosynovitis | 2 | 1.75 | 100 | .05 | NR | NR |
NR: not realizable; OA: osteoarthritis.
These results agree with those of other studies6–9 and show the efficacy of the treatment of pain in more than two thirds of the patients. Although the administration of a second RT cycle has been studied less,10 given its good tolerability it may be an interesting option in patients who do not achieve a response with the first treatment.
The evolution of techniques (smaller fields of radiation and lower doses) has helped to improve the safety profile of this procedure, so that the risk of radio-induced cancer in low dose RT treatments for benign disease is very low.11 These data therefore contribute to offering clinicians a description of RT as a safe and effective therapeutic alternative in OA and STP that are refractory to conventional treatment.
Please cite this article as: Aramburu F, Montero A, Cabrera Alarcón JL, García de la Peña-Lefevre P. Tratamiento con radioterapia en enfermedad osteoarticular benigna. Reumatol Clin. 2021;17:624–625.