Recurrent aphthous stomatitis consists on recurring oral ulcers of unknown etiology. Oral ulcers may be different in number and size depending on the clinical presentation, which also determines the time needed for healing. Moreover, there are factors associated to outbreaks but not implicated in its etiopathogenesis. When oral aphthosis has a known etiology, it is not considered as recurrent aphthous stomatitis. The severity and the clinical presentation helps in the differential diagnosis. Treatment is symptomatic in recurrent aphthous stomatitis while, if there is an underlying systemic disease, the treatment of such disease is need in addition to topical treatment.
La aftosis oral recurrente consiste en la aparición de episodios repetidos de úlceras sin que exista una causa conocida. Son úlceras orales en número y tamaño variable según la forma de presentación, la cual también condiciona el tiempo necesario para la curación. Existen factores que favorecen su aparición, pero no son causales. En determinados casos, los brotes de aftosis tienen una causa conocida y entonces no se considera una aftosis oral recurrente. La forma de presentación de las úlceras y su gravedad son claves en el diagnóstico diferencial. El tratamiento es sintomático en la aftosis oral recurrente, mientras que si existe una causa sistémica de base el tratamiento será el indicado en este caso además del tópico.
Aphtae (Greek aphtai, burn) are ulcerated lesions that sit on the mucosal surface where, unlike erosion, loss of continuity involves the whole epithelial lining and may affect the underlying connective tissue.
Aphthosis presents with ulcerated oral lesions (aphtae), which are often painful and self-limiting. The causes of oral ulcers are diverse: infectious skin diseases, cancer, hematological diseases, gastrointestinal diseases, rheumatic diseases, drugs, and radiotherapy (Table 1).1–4 They appear almost always in non-keratinized areas of the mouth found on the mucosal lining (inside of the cheeks, inner lips, soft palate, ventral tongue, and floor of the mouth), but are not exceptional in the keratinized surface that constitutes the masticatory mucosa (gingiva and hard palate), or even the specialized mucosa, which is located in the epithelium of the dorsal tongue. They are considered acute if lasting less than six weeks or chronic if they last longer. When in the form of recurrent oral outbreaks in the absence of a systemic cause, they are referred to as recurrent oral aphthosis (ROA) or recurrent aphthous stomatitis.
Main Causes of Oral Ulcers.
| Infectious diseaseHerpetic stomatitisChicken poxHerpes zosterCoxsackie Virus (hand-foot disease, herpangina)Infectious MononucleosisHIV infectionaAcute necrotizing gingivitisMycobacterium tuberculosisTreponema pallidumFungal infectionsProtozoal infections (leishmania) |
| Malignant tumors |
| Blood diseasesAnemiaLeukemiaNeutropeniaWhite cell dyscrasia |
| Gartrointestinal diseasesCeliac diseaseCrohn's diseaseUlcerous colitis |
| Skin diseasesLichen planusPemphigusPenphigoidErithema multiformisHerpetiform dermatitisLineal IgA diseaseAmpule EpidermolysisChronic ulcerous stomatitisOther dermatosis |
| Rheumatic diseasesLupus erithematosusBehçet's syndromeMAGICb syndromeSweet syndromeReactive arthritisWegener¿s granulomatosisPFAPAc syndrome |
| Drugs (Table 4) |
| Radiotherapy |
ROA is one of the most common oral disorders with a prevalence that varies across the studied populations,5 but that approximately 20% of the general population suffers at some point in their lives. There is a familial aggregation and is more common in women. It usually starts in childhood, adolescence, or young adults under 30, tending to decrease over time, both in severity and frequency.6
PathogenesisThe etiology and pathogenesis of ROA are unknown so far. It is likely that in genetically predisposed individuals, immune dysfunction linked to various triggers facilitates the development of aphtosis. Local immunological dysfunction could be related to increased T-lymphocyte subpopulations (CD4 and CD8), and plays an important role in altered immune responses in which the initial stimulus is not known. Changes in serum levels of immunoglobulins have also been described, which may play a role in the pathogenesis of ulcers and alterations in cell adhesion molecules that are essential to maintain a stable structure of the oralepithelium have been reported.7–11
Possible local and general factors have been implicated and may favor the development or worsening of ulcers12:
- 1.
Genetic. There is a familial aggregation, and some studies have correlated ROA to HLA13–15 antigens. The chance of developing aphthous lesions is 90% in people with two parents who present them, reduced to 20% in those in which parents have never presented them.16
- 2.
Immune imbalance in relation to likely immune events triggered by transitory immunodeficiency.17
- 3.
Infections probably mean little. There is evidence of possible cross-reactivity between bacterial antigens and the oral mucosa. Potential associations with infection by Helicobacter pylori18 as well as human herpes virus-619 have been seen.
- 4.
Mechanical trauma20 (bites, dentures, toothbrushes, etc.), thermal or chemical lesions. ROA has been related to the local irritant action of sodium lauryl sulfate, a surfactant used in many types of toothpaste, which can influence people with ROA.21
- 5.
Smoking cessation. In non-smokers there is decreased keratinization of the mucosa which is more sensitive, though, when lesions are present; when smoking, there is no effect on their severity.22
- 6.
Deficiency of vitamins and minerals like iron, folic acid and vitamin B12 in patients with frequent ROA, without significant differences while studying each element separately.23 In other studies there is a significant association with vitamin A and B1224 and B125 vitamin deficiency.
- 7.
Hypersensitivity to foods (chocolate, cheese, citrus, tomatoes, seafood, etc.).26,27 Often allergy or food intolerance is associated with atopy, and in patients with a family history of ROA, a significant association with a history of atopy28 has been seen.
- 8.
Hormonal changes. ROA has often been associated with the menstrual cycle, but this relationship has not been established clearly.29
- 9.
Stress. It may play a role as a triggering or modifying factor rather than causing ROA.30,31
The lesions are initiated by an inflammatory foci in the form of painful erythematous macules. Within hours, keratolysis mediated by cytokines leads to a shallow, rounded or oval, well-defined ulcer, with a raised inflammatory halo in which microscopically one can observe a large numbers of neutrophils, lymphocytes, and monocytes. The center is necrotic and covered by a yellowish–gray pseudomembrane (Fig. 1). They present centrifugal growth and healing is achieved by re-epithelialization from the edges.
Their presence may hinder speech, eating, and swallowing. Pain is similar to that resulting from a burn, and increases with contact with hot foods and spices.
There are three different forms of presentation of ulcers in ROA: minor, major, and herpetiform.32
- •
Minor aphthosis is the most common. It usually affects non-keratinized mucosa, especially the lips, cheeks, and sides of the tongue. It is characterized by single or few ulcers (less than 5) with a size of less than 1cm. They are usually concentrated in the front of the mouth, and often occur 2–4 times a year. They present spontaneous healing without scarring in 1–2 weeks.
- •
Major aphthosis is less common. It typically affects the keratinized and non-keratinized mucosa, especially the soft palate. It occurs in the form of single or few ulcers (less than 5) of a size equal to or greater than 1cm. They usually have a predilection for the back of the mouth. They are deeper and more painful than minor aphthae. It takes 2–12 weeks to heal and leave a scar.
- •
Aphthosis herpetiformis is the least common. It usually affects non-keratinized mucosa, especially the floor of the mouth and ventral surface of the tongue. It usually has a later onset than the two previous forms, occurring in the second or third decade of life. It manifests with a variable number of ulcers (10–100) with a size of 1–3mm appearing simultaneously and can coalesce. It takes 1–4 weeks to heal and may leave scars, especially in the coalescing ulcers.
The presentation of oral aphtae helps in the differential diagnosis. According to it, diagnosis can be guided according to whether it is a solitary ulcer, recurrent episodes of one or more ulcers that heal spontaneously, a single episode preceded by blisters, ulcers affecting multiple oral locations, or persistent oral aphthosis affecting different sites (Table 2).32 With the emergence of recurrent episodes of one or more ulcers that heal spontaneously, the differential diagnosis must be made between recurrent aphthous stomatitis, Behçet's disease, aphthous-like-ulcers due to systemic diseases or drugs and recurrent erythema multiforme.
Main Causes of Oral Ulcers According to Their Presentation.
| Single ulcerTraumaSquamous carcinomaInfections (syphilis, tuberculosis) |
| Spontaneous episodes of one or more ulcers that heal spontaneouslyRecurrent aphtous stomatitisBehçet's disease“Aphthous-like-ulcers” due to systemic disease or drugsRecurrent erithema multiformis |
| Single episode of vesicle preceded ulcers which affect multiple oral localizationsViral infections (herpangina, primary herpetic stomatitis)Erithema multiformis |
| Persistent oral ulcers affecting different localizationsSkin and mucosa (oral lichen planus)Autoimmune ampules (oral pemphigus)Gastrointestinal (Crohn's disease)Hematological (leukemia)Drugs |
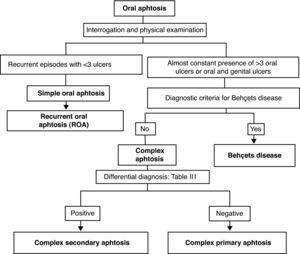
In addition to the presentation of oral aphtae, the severity of clinical manifestations of oral aphthosis also helps to make the differential diagnosis. With this criterion they are classified as simple aphthosis and aphthosis complex (Fig. 2).33–36 Simple aphthosis presentation is more frequent.1 It presents with recurrent oral lesions in any of the three ways (minor, major or herpetiformis), usually with 3–6 episodes per year that are of short duration and resolve spontaneously, allowing the diagnosis of ROA. Aphthosis complex manifests prolonged outbreaks that are often continuous, with three or more oral lesions and may be associated with genital or perianal ulcers.
Faced with a complex oral aphthosis, the first step should be to rule out Behçet's disease. Once the diagnosis has been excluded, oral aphthosis complex can be classified as primary or secondary.
To establish the diagnosis of primary complex aphthosis, one must discard all the processes that can produce and that would classify it as secondary (Table 3),35 but even so, it should be noted that the diagnosis of Behçet's disease can be difficult in the early stages and may be delayed up to several years, which justifies a careful follow-up of all patients diagnosed with complex primary aphthosis.37
Clinical Classification of Ulcers.
| Simple aphtosis: recurrent attacks of minor, major or herpetiform ulcers, with disease free periods, mostly in young persons (ROA) |
| Complex aphtosis: almost constant presence of ≥3 oral ulcers or recurrent oral and genital ulcers. Excluding Behçet's disease, it may be:Primary or idiopathic complex aphtosisComplex secondary aphtosis:Intestinal inflammatory diseaseHIV infection (human immunodeficiency virus)Cyclic neutropeniaPFAPA syndrome (“Periodic Fever, Aphthous stomatitis, Pharyngitis, cervical Adenitis”)Iron, zinc, folate or vitamin B1, B2, B6, B12 deficiencyGluten enteropathy |
| Behçet's disease |
| MAGIC syndrome (“Mouth And Genital ulcers with Inflamed Cartilages”) |
Secondary complex oral aphthosis may be a sign of many systemic processes that may present with episodes similar to recurrent oral aphthosis. The most common is inflammatory bowel disease, of which it may be its first manifestation.
In clinical rheumatology practice it is not uncommon to find ulcers secondary to certain drugs and some diseases with joint manifestations.
As for drugs, there have been many cases of oral ulceration in relation to them, and among them, several are commonly used in rheumatology, even to treat systemic diseases, which in turn can cause oral aphthosis (Table 4).38–42
Drugs That Produce Oral Ulcers.
| Alendronate | Diclofenac | Interpheron | Penicillamine | |
| Alprazolam | Dideoxycytidine | Interleukin-2 | Penicillin | |
| Allopurinol | Dilthiazem | Imipramine | Potassium | |
| Aspirin | Disopiramide | Isoprenaline | Proguanile | Chloride |
| Atorvastatin | Docetaxel | Ketorolac | Promethazine | |
| Aurothiomalate | Doxorrhubicine | Lamotrigin | Propanolol | |
| Azathioprine | Emepronius-Bromide | Leflunomide | Propilthyouracil | |
| Aztreonam | Enalapril | Levamizole | Quinidine | |
| Barbiturates | Erythromicine | Lythium | Ritonavir | |
| Bleomi¡ycin | Everolimus | Losartan | Sachinavir | |
| Captopril | Phenilbutazone | Melphan | SertralineStreptomycin | |
| Carbamazepine | Phenindione | Metamizole | Sulphonamides | |
| Cyclosporine | Phenitoin | Methotrexate | Sulindac | |
| Cisplatin | Fluconazole | Metronidazole | Terbutaline | |
| Citarabine | Flunisolide | Mitomycin | Tetracyclines | |
| Claritromicina | Fluoxetin | Molgramostim | Vancomycin | |
| Clonazepam | Gancyclovir | Naproxen | Vincristin | |
| Chloranphenicole | Hydralazine | Nicorandil | Venlaphaxine | |
| Chloroquine | Hydroxiurea | Niphedipine | Warfarin | |
| Chloropromacine | Ibuprofen | Olanzapine | Zidovudin | |
| Codeine | Indomethacin | Pancreatine |
With regard to the systemic diseases that may have joint involvement (arthritis or joint pain), some include the presence of ulcers among their diagnostic criteria:
- 1.
Lupus erythematosus: oral or nasopharyngeal ulcers, usually painless, observed by a physcian.43
- 2.
Behçet's disease: recurrent oral ulcers (major, minor or herpetiform aphthosis) seen by a physician or patient and having occurred at least three times in a period of 12 months.44
- 3.
Wegener's granulomatosis: oral or nasal inflammation to the development of painful or painless oral ulcers or purulent or bloody nasal discharge.45
- 4.
Crohn's disease: multiple small aphthous ulcerations in the upper and lower digestive tract, not necessarily with longitudinal organization, for at least three months, plus caseous granulomas.46
- 5.
PFAPA syndrome (“Periodic Fever, aphthous stomatitis, pharyngitis, cervical adenitis”): oral ulcers.47
Other systemic diseases that have or may have joint involvement, and sometimes present with oral ulcers, but their presence is not included among diagnostic criteria:
- 1.
Reactive arthritis may be present and typically are not painful.48
- 2.
Sjögren's syndrome: a dry oral mucosa often present ulcers.49
- 3.
Sweet syndrome or acute neutrophilic febrile dermatosis.50,51
- 4.
Ulcerative colitis: ulcers are more prevalent than those found in a control group of patients with functional disorders of intestinal motility,52 but are more persistent and tend to be larger.53
Another syndrome that may be considered in the differential diagnosis of rheumatic diseases capable of producing an oral aphthosis complex is the MAGIC (“mouth and genital ulcers with inflamed cartilage”) syndrome, which has no established diagnostic criteria, but is manifested by an overlap between Behçet's syndrome in which recurrent ulcers are a diagnostic criterion and relapsing polychondritis.54
TreatmentLack of knowledge regarding the cause of ROA makes it impossible to cure the disease. Existing symptomatic treatments are directed at reducing pain, shortening the healing of ulcers, and increasing the length of asymptomatic periods between attacks. When ulcers are small, with few symptoms and infrequent, topical treatment along with dietary measures such as avoiding foods that can worsen ulcers is sufficient, including those that due to their hard texture could erode the oral mucosa. If identified precipitating factors can be corrected, and act on them. If there is a basic process that explains the appearance of aphthosis, treatment of it leads to improvement.
A systematic review of the outcome of various topical treatments used in ROA reached the following conclusions as to their ability to decrease the incidence of ulcers and their analgesic power55:
- 1.
Chlorhexidine
- a.
Incidence of ulcer. Compared with placebo mouthwash may be more effective in reducing the severity, incidence and duration of the ulcer (very low quality evidence).
- b.
Analgesia. Compared with placebo gel may be more effective in reducing pain (very low quality evidence).
- a.
- 2.
Hexetedine
- a.
Incidence of ulcer. Compared with placebo may not be more effective in reducing the severity, incidence and duration of the ulcer (very low quality evidence).
- b.
Analgesia. Compared with placebo may not be more effective in reducing pain (very low quality evidence).
- a.
- 3.
Carbenoxolone gel or mouthwash
- a.
Incidence of ulcer. Compared with placebo mouthwash may be more effective in reducing the number of ulcers (very low quality evidence).
- b.
Analgesia. Compared with placebo mouthwash may be more effective in reducing pain (very low quality evidence).
- a.
- 4.
Topical corticosteroids
- a.
Incidence of ulcer. Compared with placebo may be more effective in reducing the incidence of new ulcers and their duration (very low quality evidence).
- b.
Analgesia. Compared with placebo may be quicker to reduce the amount and duration of pain without causing adverse local or systemic events (very low quality evidence).
- a.
- 5.
Local anesthetic: benzidamide mouthwash
- a.
Incidence of ulcer. Compared with placebo may not be more effective in reducing the incidence of new ulcers (very low quality evidence).
- b.
Analgesia. Compared with placebo may not be more effective in reducing pain, but may be preferred for its transient topical analgesic effect (very low quality evidence).
- a.
- 6.
Tetracycline mouthwash
- a.
Analgesia. Compared with placebo may be more effective in reducing pain (very low quality evidence).
- a.
Other topical treatments such as sucralphate56 have also been proposed, which act by forming a protective film on the bottom of the oral ulcers, reducing pain and shortening healing time. Amlexanox 5% also leads to a rapid healing of ulcers when applied as oral ointment.57
Local cauterization by caustic solutions such as silver nitrate58 has been employed. Cryotherapy with liquid nitrogen has been used, but has not shown greater analgesic effect than placebo.59 Laser treatment60 has also been used, as has low intensity ultrasound.61
If ROA presents with recalcitrant recurrent episodes several systemic treatments have been recommended with varying success, including: steroids,62 pentoxiphylin,63 levamisole,64 colchicine and dapsone,65 thalidomide,66,67 biologic drug68 treatment,69 clophazimine,70 and others (methotrexate, azathioprine, cyclosporine, cyclophosphamide, etc.).71,72
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Riera Matute G, Riera Alonso E. La aftosis oral recurrente en Reumatología. Reumatol Clin. 2011. doi:10.1016/j.reuma.2011.05.003.