Extraarticular synovial osteochondromatosis is a very rare benign disease whose aetiology may be primary or secondary to pre-existing pathology or after trauma. The diagnosis can be made with plain radiography and CT, and MRI is necessary to evaluate the non-mineralized soft tissue component and assess extension. It must be confirmed with a pathological study by biopsy or resection. There is up to a 5% chance of malignant transformation. The treatment of choice for the extensive extra-articular form is surgery by open resection.
The case presented illustrates an atypical form of secondary extraarticular OCS with multiple involvement of the leg, ankle and foot.
La osteocondromatosis sinovial (OCS) extraarticular es una enfermedad benigna muy infrecuente cuya etiología puede ser primaria o secundaria a una patología preexistente o tras traumatismos. El diagnóstico puede realizarse con radiografía simple y TC, siendo necesaria la RM para evaluar el componente de partes blandas no mineralizado y valorar la extensión. Debe confirmarse con estudio anatomopatológico mediante biopsia o resección. Tiene hasta un 5% de posibilidades de experimentar transformación maligna. El tratamiento de elección de la forma extraarticular extensa es quirúrgico mediante resección abierta.
El caso presentado ilustra una forma de aparición atípica de la OCS extraarticular secundaria con afectación múltiple de la pierna, tobillo y pie.
Synovial Osteochondromatosis (SOC) is a rare, benign disease of the synovial membrane which may affect joints, bursas and tendon sheaths.1,2 Intra-articular involvement of large joints like the knee is most common. Extra-articular SOC is rare and predominates in tendon sheaths or bursas, mostly of the hands and ankles, rarely involving the foot.1,3
Few cases of extra-articular SOC have been described in the literature, as far as we know and no cases with such an extensive extra-articular involvement have been described. We present the exceptional case of a patient with extra-articular synovial osteochondromatosis with the involvement of the leg, ankle and foot.
Clinical observationWe present the case of a 51-year-old man with no medical history of interest. He was referred to our hospital due to a lump of 3year onset and the slow growth in the external malleous and lateral side of the right foot, which was hard and not moveable. He stated it had been painful for a year and he suffered functional limitations. He only referred to a twisting and trauma of the ankle and foot 10 years previously. Laboratory tests were normal.
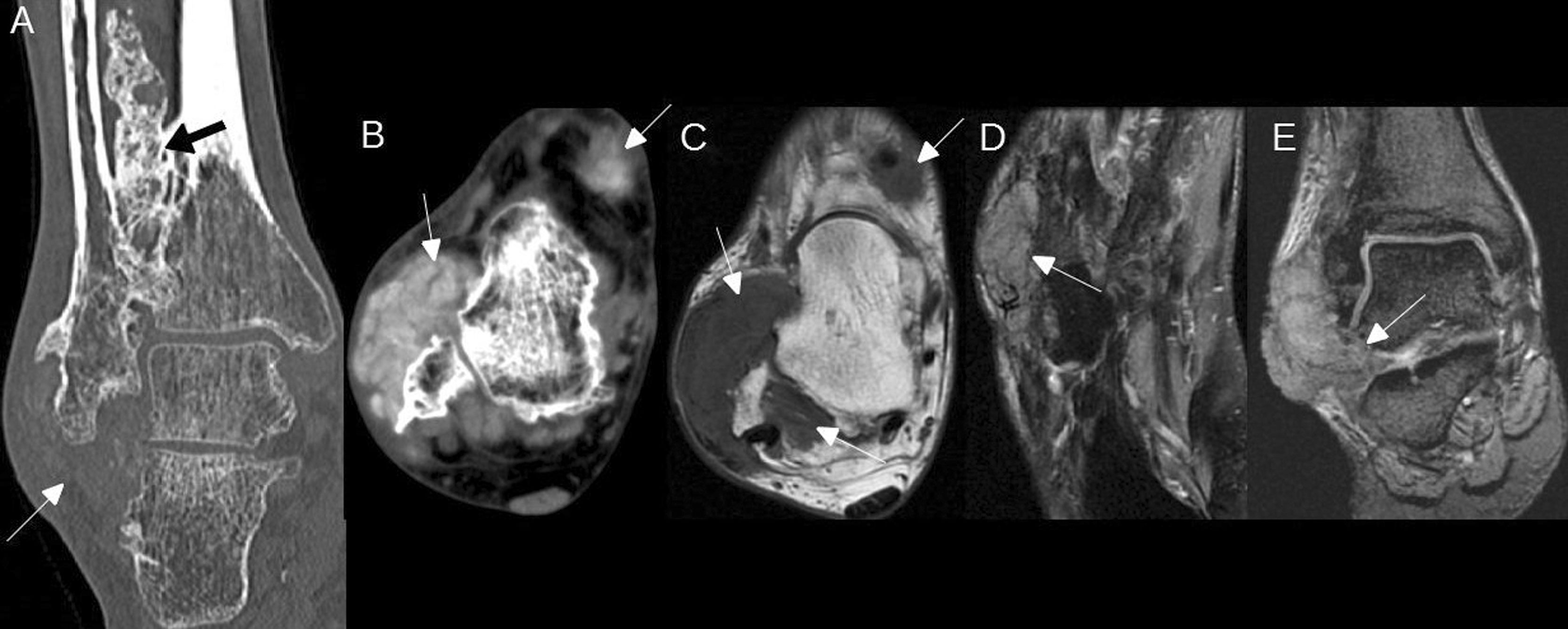
Plain radiography, computerised tomography (CT) and magnetic resonance (MR) were performed (Fig.1), which showed extensive irregular calcification of the interosseous membrane of the leg and several lobulated masses of soft tissues with different levels of mineralisation in ankle and foot. SOC, multiple osteochondromas, chondrosarcoma and disease from microcrystal deposits were included in the differential diagnosis. A biopsy of the soft tissue mass of the lateral face of the ankle was performed and the anatomopathological report was: extra-articular post-traumatic SOC.
Extensive extra-articular SOC. A) CT with no contrast agent in coronal plane which shows extensive irregular calcification of the interosseous membrane (black arrow) and mass of soft tissues in the lateral side of the ankle with scarce mineralisation (White arrow). B) CT with no contrast agent in axial plane which shows masses of soft tissues in the dorsal and lateral side of the ankle, with incipient diffuse mineralisation (arrows). C) MR with axial sequence T1 with no contrast agent, which shows the same masses as in B (arrows), isointense with respect to the muscle. D) MR with axial DP Fat Sat pulse sequence, which shows a mass of adjacent soft tissues to the base of the fifth metatarsal, of intermediate signal intensity due to incipient diffuse mineralisation (arrow). E) MR with coronal 2 GRE sequence which shows the mass of soft tissues on the lateral side of the ankle extending towards the sinus tarsi (arrow).
SOC is a rare, benign entity which is characterised by metaplasia and the formation of multiple cartilaginous nodules in the synovial membrane of joints, bursas and tendon sheaths.4 It is more frequent in its intra-articular form, with the extra-articular form being a rarity.1
Proliferous cartilaginous nodules may become detached from the synovial joint, forming loose intra-articular bodies. On rare occasions these cartilaginous nodules may cross the articular capsule and proliferate as extra-articular,1 which we believe happened in our case, since the patient’s involvement was extensively intra and extra-articular.
SOC may be classified into 2 forms: primary and secondary. The primary form is due to benign reactive metaplasia of the synovial membrane. The secondary form is associated with pre-existing articular disease such as trauma, osteonecrosis, infection, rheumatoid arthritis, synovitis, osteoarthritis, osteochondritis dissecans and neuropathic arthropathy.4,5 The 2 forms have typical histopathological characteristics which differentiate them. In our case, the background of trauma supported the diagnosis of secondary SOC.
Extra-articular SOC is difficult to detect during initial stages.4 Clinically speaking it may start with pain, deformity, functional limitation, palpable mass and paresthesias due to neurovascular compression.6,7
Radiological appearance depends on the stage of the disease and the degree of mineralisation of the cartilaginous nodules.1,4,6 If the extra-articular fragments are calcified they may be detected by plain radiography and CT, but for the diagnosis of non calcified masses, a study with MR is necessary, with this technique being highly useful in the early stage of the disease, for diagnosis and for assessing extension.1 Definitive diagnosis is established using anatomopathological study.7
There is a 5% probability of malignancy, essentially towards low-grade chondrosarcoma. A form of aggressive presentation, the rapid growth with destruction of neighbouring structures and multiple relapses after surgical treatment must lead to suspicion of a possible malignant transformation.7
The treatment of choice for the intra-articular form is the arthroscopic extraction of loose bodies and synovectomy,1 but in the cases of extensive and extra-articular SOC, as in our case, open resection is indicated.6
ConclusionThe case presented illustrates an atypical form of secondary extra-articular SOC presentation with multiple involvements of leg, ankle and foot. Although this is rare, it should be included within the differential diagnosis of peri-articular soft tissues of long duration with different degrees of mineralisation.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García Espinosa J, Moya Sánchez E, Martínez Martínez A. Osteocondromatosis sinovial extraarticular secundaria con afectación de pierna, tobillo y pie. Un caso excepcional. Reumatol Clin. 2021;17:482–484.