Septic arthritis is a condition that is caused by bacterial nesting in the synovial membrane leading to an inflammatory response that causes the acute purulent synovial fluid appearance. It is a medical emergency because of rapid anatomical and functional impairment. From the etiological viewpoint, Gram-positive bacteria such as Staphylococcus aureus (S. aureus), are implicated in over 50% of cases, followed by Streptococcus (15%–20%) and Gram-negative bacteria. In its epidemiology various risk factors such as advanced age, immunosuppression, presence of prosthetic joints, and patient comorbidities, influence the disease. Sometimes the early diagnosis of septic arthritis is difficult and this increases the risk of joint destruction.1
We present the case of a patient with two successive episodes of septic arthritis, caused by different microorganisms and microcrystalline arthritis associated with monosodium urate and calcium pyrophosphate deposits.
The patient, an 86-year-old woman, presented no allergies, no history of substance abuse and was independent for activities of daily living. She had a history of atrial fibrillation treated with warfarin and tophaceous gout. In the last month she presented an episode of septic arthritis of the right shoulder caused by Escherichia coli (E. coli), due to bacteremia secondary to a urinary tract infection. She was treated with intravenous ciprofloxacin 400mg every 12h for 2 weeks (continued with a dose of 750mg orally for 6 weeks) presenting improvement. Fifteen days after this episode, she presented with pain and swelling of her left knee which had lasted for a week without fever or other symptoms.
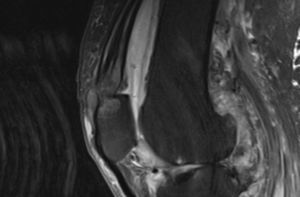
On physical examination, the patient was afebrile and stressed left knee monoarthritis with functional impotence for knee flexion. The rest of the examination found no significant alterations. Arthrocentesis was performed, yielding 4cm3 of liquid of inflammatory characteristics: 9650leukocytes/mm3 with a predominance of polymorphonuclear cells (94%) and glucose 75mg/dl. Monosodium urate crystals were observed under polarized light microscopy. Gram stain was negative. The synovial fluid culture was isolated Escherichia faecium (E. faecium) sensitive only to vancomycin. Laboratory tests showed no leukocytosis (8600/109 leukocytes, 60% neutrophils, 20% lymphocytes) but elevated acute phase reactants (ESR: 100mm in the first hour, C-reactive protein: 238mg/dl). Urine sediment was normal and blood and urine cultures negative. We completed the study with a chest X-ray and echocardiography to rule out pulmonary and/or cardiac affection. A simple X-ray of the left knee showed signs of advanced degenerative joint disease with marked tibiofemoral joint space narrowing and increased soft tissue density and joint effusion. Magnetic resonance imaging showed a tophi in the patellar insertion of the quadriceps tendon that caused a major erosion in the upper pole of the patella (Fig. 1). Antibiotic treatment was initiated with vancomycin, 1g every 48h (adjusted for renal function).
Joint lavage was performed daily with saline but was unproductive. After 10 days of antibiotic treatment and the continued signs of knee arthritis, as well as the isolation of the germ in serial cultures, a surgical arthrotomy and debridement with subtotal synovectomy was performed.
The breakdown of the articular surface and the large amount of tophaceous deposits were notable. Cultures after surgery were negative. The pathology of the synovial fluid showed urate and calcium pyrophosphate crystals. The patient remained hospitalized up to a month for intravenous treatment and rehabilitation, which was started early.
Enterococci are Gram-positive diplococci that are part of the normal flora of the human gastrointestinal tract and genital tract of women. They may also be isolated in soil, food, water, plants, birds, insects and other animals. The frequency of isolation of different species varies with the host. E. faecalis and E. faecium are the dominant species in the human gut, and between the 2 they make up 95% of the microorganisms in the gastrointestinal tract.2 Multiple Entercococcus cause nosocomial infections (urinary infections, endocarditis, diverticulitis, meningitis and bacteremia) and are resistant to multiple antibiotics. The immunosuppressed population and patients with chronic diseases such as gout are more likely to have a septic arthritis.1 Several hypotheses have been put forward regarding the mechanism of coexistence of septic arthritis and microcrystalline deposition such as local pH reduction by the influx of neutrophils and lactic acid production that would favor the precipitation of uric acid crystals, articular cartilage destruction by lysosomal enzymes and the formation of intraarticular crystals, which would enhance the inflammatory effect of urate crystals by endotoxins and local temperature increase.3 In contrast, the inflamed synovial allows easier access to circulating bacteria, allowing them to settle in the already affected joints (gout, pseudogout, osteoarthritis, prior septic arthritis).3,4 Furthermore, in our case, previous hospitalization and previous antibiotic treatment probably acted as risk factors that favored a nosocomial infection and microorganism resistance to conventional antibiotics.
The largest series of septic arthritis and gout was described by Yu et al.,5 and includes patients with both diseases seen in a period of 13 years (1987–2001). The germ that was most frequently isolated was S. aureus. In no case was Enterococcus isolated. In a literature review of PubMed ranging from 1972 to 2012 (keywords septic arthritis, gout, pseudogout) we found three cases in which the three diseases coexisted.6–8 The Spanish series of Minguez et al.,9 described 18 cases. In this series, all cases were septic arthritis associated with monosodium urate or pyrophosphate microcrystalline arthritis, i.e., a single crystal type. However, pyogenic arthritis due to E. faecium associated with the presence of monosodium urate crystals and pyrophosphate was not described. In clinical practice the role of arthrocentesis is fundamental in any arthritis as is synovial fluid culture despite the evidence of crystals: a delay in diagnosis and treatment triggers the destruction of the joint.
Please cite this article as: Tejera B, et al. Artritis séptica asociada a gota y seudogota: la importancia de la artrocentesis. Reumatol Clin. 2014;10:61–62.