Behçet's disease (BD) is a chronic relapsing occlusive vasculitis of unknown etiology, characterized by the presence of oral and genital ulcers and intraocular inflammation, with less common cutaneous, joint, vascular, digestive and neurological involvement.1
The presence of neurological symptoms in the context of BD constitutes what is called neuroBehçet's, characterized in most cases by the presence of aseptic meningitis, cerebellar signs, intracranial hypertension, and pyramidal alterations.2 We report the case of a 34 year old male with a history of BD, who presented an altered consciousness and meningeal signs, diagnosed with neuroBehçet and showing a favorable clinical response to treatment with triple immunomodulatory therapy.
The patient is a Spanish man of 34 years with BD, in whom the diagnosis was established by the presence of oral and genital ulcers and repeated episodes of anterior uveitis three years prior, treated with prednisone at a dose of 5mg/day and cyclosporin A. He came to the emergency department 24h before due to a self-limited episode of loss of consciousness and subsequent headache and vomiting. The general physical examination and vital signs were normal except for the presence of nuchal rigidity upon neurological examination. There were no signs of disease activity at the time of the initial evaluation.
He was put in reverse isolation for suspected intracranial meningeal syndrome secondary to infection due to immunosuppression. During observation in the emergency department a blood count was performed which showed 4130 WBC E9/l and no left shift, hemoglobin 11.5mg/dl, hematocrit 36%, ESR 12mm/h, lactate dehydrogenase 97U/L, total protein 6.2g/l albumin 3g/l, and a computed tomography that revealed no significant structural alterations.
In accordance with the headache and meningeal signs a lumbar puncture was performed, resulting inconclusive due to a traumatic technique, and no second sample was obtained. However, the patient was admitted to the neurology department with empirical intravenous antibiotic therapy based on ceftriaxone and vancomycin as well as acyclovir for antiherpetic coverage.
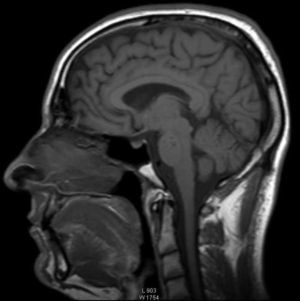
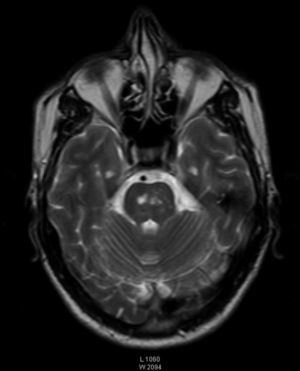
During admission, he underwent a second lumbar puncture with glucose 56mg/dl, protein 68mg/dl and WBC 600/μl (90% polymorphonuclear cells, 10% lymphocytes). Due to the polymorphonuclear pleiocitosis we performed a magnetic resonance imaging (MRI) scan (Fig. 1), which showed an extrusion affection with extension to the left cerebral peduncle which appeared isointense on T1, hyperintense on T2 (Fig. 2), and flair, and hypointense on T1 IR.
Microbiological studies with Gram and Ziehl–Neelsen stains of the cerebrospinal fluid cultures (including Lowenstein), polymerase chain reaction for herpes virus, Brucella and Borrelia serologies were negative. We also excluded other possible differential diagnoses considering the history of immunosuppression: varicella zoster virus, herpes virus, pox, cytomegalovirus, Candida and meningeal lymphomatosis.
He was assessed by neurology who considered neuroBehçet given the persistence of symptoms despite antibiotic treatment and the medical history of the patient and who initiated infliximab therapy associated with tuberculosis prophylaxis with isoniazid, prior suspension of antibiotic treatment and cyclosporin A, the latter due to the relationship described in the literature with worsening neurologic manifestations.3,4
Regarding the imaging differential diagnosis it should be noted that, because of its topography and signal intensity, similar images can be seen in early forms of multiple sclerosis and postinfectious encephalopathy. Viral rhomboencephalitis would be a differential diagnosis also, but it is a rare condition in which the injury is unique, extensive and of pontine dominance. Given the history, the clinical and laboratory tests, we oriented the diagnosis toward neuroBehçet.
The patient showed significant clinical improvement and resolution of the headache and nuchal rigidity. A third lumbar puncture was performed 72h after treatment initiation, with glucose 52mg/dl, protein 48mg/dl and 100/μl with predominantly mononuclear leukocytes.
Considering the rapid radiographic and clinical improvement after receiving anti-TNF therapy,5 we conclude that the patient had BD related aseptic meningitis; the patient was discharged with prednisone 1mg/kg/day, isoniazide-pyridoxine, infliximab and azathioprine. Control brain MRI showed no lesions described in the previous study and presently the patient had no recurrence of neurological affectation.
The central and/or peripheral nervous system affection occurs in about 5%–25% of patients with BD. It is more common in males and usually presents between 3 and 6 years following the onset of illness. Presentation as the first manifestation of the disease is rare.6,7
Involvement of the central nervous system (CNS) is the most prevalent and there are two clinical forms: parenchymal and non-parenchymal affection.8 This clinical, pathological, radiological differentiation is important and influences prognosis since parenchymal injury is more prevalent (80% of cases) and has a worse prognosis.9 The clinical presentation is nonspecific and varied, including loss of consciousness, seizures, confusion, lethargy, psychiatric disorders, personality changes and dementia.10,11 Unlike immunosuppressed patients without BD, meningitis can be present as oligosymptomatic, subacute, or associated to cranial nerve disorders.
In the context of an BD our patient presented neurological manifestations and we established the diagnosis of neuroBehçet supported in patient study and prior exclusion of other causes. The presence of signs of meningeal inflammation is common in the CNS parenchymal form; however, the presentation as isolated meningitis is quite rare. This case highlights, therefore, the importance of ruling out an infectious etiology, particularly in patients undergoing immunomodulator treatment.
MRI findings in relation to the progression of the disease and the initial phase T2 hyperintensity areas in the brainstem, basal ganglia and brain hemispheres, followed by an intermediate stage of edema with a mass effect and microhemorrhages and a third stage with brainstem atrophy have been described.12,13 In our case, there was no clinical but rather imaging evidence of thromboencephalic involvement, with findings corresponding in our patient with his initial changes.
In accordance with the above, it is advisable to perform MRI controls for tracking injuries once the treatment is started although these lesions can take months or years to disappear14; in our case, we verified resolution after 5 weeks of triple therapy with immunomodulatory therapy.
Please, cite this article as: Andrade-Rodado FM, et al. Meningitis aguda en la enfermedad de Behçet. Reumatol Clin. 2014;10:59–61.