Infections in patients with systemic vasculitis represent one of the main causes of mortality. Corticosteroid use, immunosuppressive therapy, age, associated organic involvement and dialysis dependence are risk factors of infection.
ObjectivesTo determine the prevalence of severe infection and associated factors in patients diagnosed with ANCA-associated vasculitis (AAV) and Polyarteritis Nodosa (PAN).
Methodsretrospective study was conduced in a single rheumatology center (2000–2018). We included patients diagnosed with AAV (Granulomatosis with Polyangiitis (GPA), Eosinophilic Granulomatosis with Polyangiitis (EGPA) and Microscopic Polyangiitis (PAM) and Polyarteritis nodosa (PAN). Serious infectious events requiring hospitalisation or prolonged antibiotic/antiviral treatment, recurrent infection of Herpes Zoster Virus or opportunistic infections were evaluated. Sites of infection, isolated microorganisms and mortality related were analyzed.
Results105 patients were analyzed, follow-up time median 18 m, 58.7% were women and median age was 52 years. Types of vasculitis: 41.9% PAM, 16.2% EPGA, 40% GPA, 1.9% PAN. Constitutional, pulmonary, renal and otorhinolaryngology manifestations were the most frequent.
Prevalence of infection34.2%, with a median of 3 months from diagnosis of vasculitis to the infectious event. Low respiratory tract (42.8%), sepsis (31.4%), and urinary tract (14.3%) were the most common sites of infections. Bacterial aetiology was the most prevalent (67.7%). Mortality at the first event was 14.3% and a 72.2% of patients were in the induction phase of treatment.
Infectious events were significantly associated with age > 65 years (p = 0.030), presence of lung (p = 0.016) and renal involvement (p = 0.001), BVASv3 > 15, mortality (p = 0.0002).
ConclusionsThe prevalence of infection was 34.2%. Lower airway infections, septicemia and urinary tract infections were the most prevalent. Infections were associated with renal and pulmonary involvement, age older than 65 years and score BVAS > 15. Severe infections were associated with mortality, especially in elderly patients.
Las infecciones en pacientes con vasculitis sistémica representan una de las principales causas de mortalidad. Son factores de riesgo conocidos la edad, el compromiso orgánico asociado, el uso de corticoides y de inmunosupresores, asi como el requerimiento de diálisis, entre otros.
ObjetivoDeterminar la prevalencia de infección severa y factores asociados en pacientes diagnosticados de Vasculitis asociada a ANCA (VAA) y Poliarteritis Nodosa (PAN).
MétodosEstudio retrospectivo realizado en un único centro de reumatología entre los años 2000 y 2018. Se incluyeron pacientes con Granulomatosis con Poliangeítis (GPA), Granulomatosis Eosinofílica con Poliangeítis (EGPA), Poliangeítis Microscópica (PAM) y PAN. Se registraron eventos infecciosos severos que requirieron hospitalización o tratamiento antibiótico/antiviral prolongado, infección recurrente por Virus Herpes Zoster o infecciones oportunistas.
ResultadosSe incluyeron 105 pacientes, la mediana del tiempo de seguimiento:18 m, 58.7% mujeres, mediana de edad 52 años, siendo 41.9% PAM, 16.2 % EGPA, 40% GPA, 1.9% PAN. El compromiso constitucional, pulmonar, renal y otorrinolaringologico fue el más frecuente.
Prevalencia de infección34,2% con una mediana de 3 meses desde el diagnóstico de vasculitis. Las infecciones de vías respiratorias bajas (42,8%), la sepsis (31,4%) y el tracto urinario (14,3%) fueron los sitios de infección más comunes. Predomino la etiología bacteriana (67.7%). La mortalidad en el primer evento fue del 14,3%. Se encontraban en fase de inducción del tratamiento el 72,2%. Las infecciones se asociaron significativamente con edad > 65 años ( p: 0,030), compromiso pulmonar ( p 0,016), renal ( p 0.001), BVAS3 > 15 y a mortalidad (p 0.0002).
ConclusionesLa prevalencia de infecciones graves fue del 34,2%. Las infecciones pulmonares, septicemia y urinarias fueron las mas frecuentes y se asociaron a compromiso renal y pulmonar, asi como a mortalidad, especialmente en pacientes de edad avanzada.
Systemic necrotising vasculitis covers a heterogeneous group of conditions characterised by inflammation of the blood vessels with varying degrees of organ involvement. They entail a morbi-mortality rate of nearly 90% within two years of diagnosis if the patient does not receive appropriate treatment.1
Given their elevated morbidity and social burden, early diagnosis and timely treatment become all the more important.
ANCA-associated small-vessel vasculitis share certain clinical, pathological, and laboratory features that make it possible to group them together, including: granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA).
In contrast, panarteritis nodosa (PAN) is a type of necrotising vasculitis that presents systemic manifestations as a result of involvement of small and medium-sized muscular arteries.2,3
The introduction of corticosteroids and immunosuppressive therapy over the last four decades has impacted mortality, turning these disorders into chronic diseases with long-term morbidity and mortality.1,4 These commonly used therapies target multiple immune system targets, including T and B lymphocytes. The risk of infection in vasculitis appears to be linked to the acquisition of immune deficits from the underlying disease and the use of immunosuppressive therapies such as cyclophosphamide, azathioprine, methotrexate, mycophenolate mofetil, and biologic drugs such as rituximab, among others.5–7
Most deaths among individuals with ANCA-associated vasculitis take place within the first three months of treatment when high-dose corticosteroids are being used and disease activity is at its highest.6
Data from four randomised, controlled trials that enrolled 524 participants reported that the infectious cause accounted for 50% of all deaths in these subjects during the first year of follow-up, compared to 14% as a consequence of vasculitis alone. The most commonly reported infectious complications were respiratory infections and septicaemia.5–7 Risk factors predictive of infection have also been identified such as corticosteroid use, intensity of immunosuppressive therapy, age, presence of lymphopenia, hypogammaglobulinaemia, associated organ involvement, and dialysis dependence in ANCA-associated vasculitis.6–14 Nevertheless, most of these studies have been conducted in cohorts of patients in European or American centres, and their prevalence in Spain is as yet unknown, although Hispanic subjects have been reported to suffer greater severity.15 Moreover, infection in individuals with vasculitis is one of the leading causes of death within the first year of diagnosis.
Objectives- a)
To determine the prevalence of infection in people diagnosed with: GPA, EPGA, PAM, and PAN, the clinical and laboratory characteristics related to and risk factors that are predictive of infection in patients receiving care at General San Martin de La Plata Acute Care Hospital.
- b)
To assess the mortality rate associated with severe infections compared to those patients without severe infection.
This was an analytical, observational, retrospective, retrospective, non-interventional, case-control study. Data were collected from the medical records of patients with a diagnosis of ANCA-associated small vessel vasculitis (GPA, EPGA, PAM) and PAN who met ACR 1990 classification criteria or according to the 2012 Chapel Hill Consensus Conference nomenclature, who were seen between 2000 and 2018.
Individuals with a diagnosis of secondary vasculitis, large vessel vasculitis, Kawasaki, variable vessel vasculitis, organ-limited vasculitis, and small vessel vasculitis due to immunocomplexes were excluded.
The following demographic information was recorded: sex, age at diagnosis of vasculitis, age at time of infection, type of vasculitis, and time of disease evolution until the infectious episode.
Clinical manifestations attributed to the underlying diseaseOrganic compromise was defined as the presence of clinical manifestations including the following kinds of involvement: cutaneous, otorhinolaryngological, pulmonary, cardiovascular, renal, neurological, systemic constitutional symptoms, ocular, and gastrointestinal on the modified Birmingham Vasculitis Activity Score (BVAS v3).
End-stage renal disease was defined as the need for dialysis or renal transplant.
- -
Disease activity was evaluated using BVAS v3.
- -
Laboratory data recorded: hemogram, presence of leukopenia (<4000/mm3), lymphopenia (<1000/mm3), serum creatinine (mg/dL), glomerular filtration rate (mL/min), proteinuria in 24-h urine (g/24 h), serum albumin (g/dL), hypogammaglobulinemia (g/L), and acute phase reactants APR (mm/h), and CRP (mg/dL).
Immunological: ANCA C or P antibodies were detected by indirect immunofluorescence or based on antigenic specificity (ANCA-PR3, ANCA-MPO) by enzyme-linked immunosorbent assay (ELISA). Indirect immunofluorescence was the technique used for screening or detection of people suspected of ANCA-associated vasculitis between the years 2000 and 2010. Starting in 2010, this technique was complemented with ELISA determinations of ANCA and, beginning in 2017 based on the ANCA 2017 testing consensus document, ELISA is performed as the primary screening method.
Treatment received at the time of the infectious episode- 1
Corticosteroid doses prior to the onset of the infectious episode were considered as follows: low doses of prednisone or equivalent ≤7.5 mg/day, medium doses between 7.5 and 30 mg/day, and high doses ≥30 mg/day.16
- 2
Immunosuppressant drugs used in the previous month, time between initiation of immunosuppression and the first infectious event, differentiating between whether the patient was in the induction or maintenance period of his or her vasculitis.
Severe infection was regarded as an infection requiring hospitalisation or intravenous or prolonged antibiotic/antiviral treatment, herpes zoster virus recurrences, or opportunistic infections. Opportunistic infection was considered to be one caused by a microorganism (bacterium, virus, fungus, or protozoan) that has weak virulence capacity, but that causes disease in an immunocompromised host. Mild infections such as rhinitis, bronchitis, or cystitis were not considered.
The infectious focus and isolated microorganisms were recorded.
Mortality related to the infectious episode was analysed.
Ethical considerationsThe study was evaluated and approved to be undertaken by the Ethics and Teaching Committee of the San Martín de La Plata Hospital and carried out in accordance with the local ethical standards and as set forth in the 2013
Statistical analysisFor continuous numerical variables, a descriptive analysis was performed using the mean and median as measures of central tendency and the standard deviation and interquartile range as measures of dispersion, according to the distribution of the variable analysed. In the case of categorical variables, absolute and relative frequencies were used as summary measures. Comparisons of inter-group means were conducted using the Mann-Whitney test and proportions of categorical variables were compared by means of the χ2 test. A logistic regression model was constructed to adjust for the influence of potential predictive variables for developing infection, such as age, markers of renal disease and involvement of other organs. Predictive variables that had statistical significance as per the Wald test (p < 0.05) or that modified the β coefficient of the indicator variable for severe infection by more than 20% (indicative of confounding) were retained in the model.
The association between infection and mortality was probed using the χ2 test and was adjusted for over the age of 65 years by means of logistic regression.
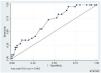
A ROC curve was created to determine a threshold on the BVAS that would be associated more frequently with infections.
ResultsA total of 105 patients were enrolled, 58.7% of whom were female. The median age at diagnosis was 52 years (IQR 40–61). Median follow-up time in months was 18 (IQR 6–39). The following conditions were recorded: PAM (41.9%; 44), GPA (40%; 42), EPGA (16.2%; 17), and non-HBV-associated PAN (1.9%; 2). Systemic involvement was present in 73.8% of the cases, with a predominance of pulmonary (63.1%), renal (58.4%), and otorhinolaryngological (43.7%) compromise. Table 1 depicts the clinical and immunological characteristics and frequency of associated clinical manifestations in each type of vasculitis.
Baseline clinical characteristics and associated organic involvement.
| Baseline clinical characteristicsType of vasculitis n (%) | GPA42 (40) | MPA44 (41.9) | EGPA17(16.2) | PAN2 (1.9) |
|---|---|---|---|---|
| Female/ male sex | ||||
| Age in years (mean, SD) | 49 ± 15.6 | 49.05 ± 15.6 | 48.8 ± 15.6 | 48.3 ± 18.7 |
| Organic involvement n, % | ||||
| Systemic constitution | 29(69) | 35(79.5) | 11 (64.7) | 150 |
| Pulmonary | 26 (61.9) | 24 (54.5) | 14 (82.3) | 0 |
| Renal | 22 (52.4) | 33 (75) | 3 (17.6) | 150 |
| Otorhinolaryngological | 30 (71.4) | 8 (18.2) | 7 (41.2) | 0 |
| Ocular | 15 (35.7) | 4 (9.1) | 2 (11.7) | 0 |
| Cutaneous | 12 (28.6) | 8 (18.2) | 4 (23.5) | 150 |
| Cardiac | 3 (7.1) | 4 (9.1) | 5 (29.4) | 0 |
| Gastrointestinal | 1 (2.4) | 3 (6.8) | 0 | 150 |
| Neurological | 11(26.2) | 16 (36.7) | 7 (41.2) | 2 (100) |
| Serology n (%) | ||||
| ANCA C by IFI | 31(73) | 13(30.9) | 3 (17) | |
| ANCA P by IFI | 6 (14.3) | 27(64.3) | 4 (23) | |
| ANCA PR3 by ELISA | 15 (35.7) | 9 (21) | 0 | |
| ANCA MPO by ELISA | 5 (11.9) | 24 (57.1) | 1 (5.8) | |
All of the participants received treatment: a 6-month induction phase with cyclophosphamide or rituximab in case of severe disease and a maintenance phase of a minimum of 24 months with azathioprine, methotrexate, or mycophenolate mofetil. In addition to the aforementioned induction therapy, plasmapheresis was performed in the event of rapidly progressive glomerulonephritis or severe alveolar haemorrhage, in line with the EULAR 2016 recommendations for the management of ANCA vasculitis.17
During induction treatment, all were given oral corticosteroids at a dose of 1 mg/kg per day not to exceed 60 mg per day or in intravenous pulses in the context of severe disease (500−1000 mg per day for 3 days).
The treatment of PAN was determined based on the presence or absence of prognostic factors for mortality according to the Five Factors Score (FFS).
Forty-six infectious episodes were recorded in 36/105 patients. Follow-up time at the time of the infectious complication was a median of 18 months (IQR 6–39). The prevalence rate of infection was 34.3% at the time of the first episode, with a median time from diagnosis of vasculitis to the first infectious episode of three months (IQR 1−15 m). The most commonly reported foci were lower respiratory infections (42.8%), sepsis for which no focus could be identified (31.4%) and urinary tract infections (14.3%). Of these patients, 27.7% presented a second infectious episode, with lower respiratory tract being the most frequent site (60%). Two patients had a third episode (soft tissue infection, septic shock). Bacterial aetiology was the most prevalent (67.6%). The most commonly isolated microorganisms were Klebsiella pneumoniae and Acinetobacter spp. in 21.4%, respectively, and polymicrobial culture in 14.3%. Table 2 lists the sites of infection and the microorganisms isolated.
Foci of infection and bacteriological isolation.
| Focus of infection | Lower respiratory tract 42.8%(n = 15) |
| Initial episode (n = 36) | Acinetobacter spp. n = 3 |
| Klebsiella pneumoniae n = 1 | |
| Pseudomonas aeruginosa n = 2 | |
| S. coagulase negative n = 1 | |
| Polymicrobial n = 2 | |
| No microbiological isolation n = 6 | |
| Sepsis with no focus 31.4% (n = 14) | |
| S. aureus n = 3 | |
| S. epidermidis n = 1 | |
| Klebsiella spp. n = 3 | |
| Candida spp. n = 2 | |
| Bulrkholderia cepacia + Enterococcus spp. n = 1 | |
| Acinetobacter spp. n = 2 | |
| Without isolation = 2 | |
| Urinary tract 14.3% (n = 4) | |
| Enterococcus spp. n = 1 | |
| Escherichia coli n = 1 | |
| Klebsiella spp. n = 1 | |
| Morganella morganii n = 1 | |
| Skin and soft tissues 8.5% (n = 3) | |
| Disseminated herpes zoster n = 3 | |
| Gastrointestinal 1.5% (n = 1) | |
| Without isolation | |
| Osteoarticular 1.5% (n = 1) | |
| Klebsiella spp. n = 1 | |
| Focus of infection | Lower respiratory tract 60% (n = 6) |
| Second episode (n = 10) | E. coli n = 1 |
| Aspergillus spp. n = 1 | |
| Scedosporium apiospermum n = 1 | |
| Polymicrobial = 2 | |
| Klebsiella spp. = 1 | |
| Skin and soft tissues 10% (n = 1) | |
| Disseminated herpes zoster (n = 1 | |
| Sepsis with no focus 20% (n = 2) | |
| Klebsiella spp. + Acinetobacter spp. n = 1 | |
| Acinetobacter n = 1 | |
| Osteoarticular (10%) n = 1 | |
| Methicillin-resistant S. aureus |
No infection by Mycobacterium tuberculosis was detected in this cohort; 60/105 (57.2%) patients had undergone a Mantoux test prior to immunosuppression, which was positive in 4 (7%) of them (>5 mm). Treatment for latent tuberculosis infection was therefore initiated.
Of the participants who developed an infectious complication, 72.2% (n = 26) were in the induction phase of treatment.
The immunosuppressant medications administered in the months leading up to the infectious episode were as follows: 52.7% (n = 19), cyclophosphamide; 11.1% (n = 4) azathioprine; 8.3% (n = 3) methotrexate; 2.2% (n = 2) rituximab; 2.7% (n = 1) mycophenolate mofetil, and 19.4% (n = 7) none. Of the subjects who were given steroids, 45.7% received high-dose steroids, 8.6% medium-dose steroids, and 28.6% low-dose steroids. The following factors associated with infection were detected in individuals with infectious episodes: leukocytopenia (22%), lymphopenia (41.9%), hypoalbuminemia (26.9%), kidney failure (58%), and haemodialysis dependence (36.3%). The bivariate analysis (Table 3) revealed that infectious episodes were significantly associated with being over the age of 65 years (p = 0.030), the presence of pulmonary involvement with pulmonary infiltrates (p = 0.016), alveolar haemorrhage (p = 0.002), presence of renal insufficiency (<0.001), the presence of RPGN (p = 0.016), and higher activity scores as measured by the BVA, median: 20 IQR 17–27 (p = 0.005). The BVAS cut-off was calculated extrapolated by calculating the area under the curve (ROC) as: score >15 (sensitivity 82.76% and specificity 41.2%; p = 0.069). In the χ2 test analysis, a BVAS score of >15 correlated significantly with a greater frequency of severe infection (p-value = 0.028; OR: 3.4; 95% CI: 1.1–10.2) compared to those patients with a BVAS score of 3 < 15.
Bivariate analysis.
| N (% of infected patients) | N (% of not infected patients) | p-value | |
|---|---|---|---|
| Sex | |||
| Male | 14 (37.80) | 23 (62.2) | NSa |
| Female | 22 (39.30) | 34 (60.7) | |
| Age > 65 years | 9 (64.3) | 5 (35.7) | 0.030a |
| Subtype of vasculitis | |||
| GPA | 11 (29.7) | 26 (70.3) | NSc |
| EGPA | 3 (18.8) | 13 (81.2) | |
| PAM | 21 (53.8) | 18 (46.2) | |
| PAN | 1 (50) | 1 (50) | |
| Subtype of ANCA | |||
| PR3-ANCA | 11 (42.3) | 15 (57.07) | NSa |
| MPO-ANCA | 14 (48.3) | 15 (57.7) | NSa |
| Associated organic involvement | |||
| Constitutional | 26 (37.1) | 44 (62.9) | NSa |
| Musculoskeletal | 14 (44.1) | 18 (55.9) | NSa |
| Cutaneous | 5 (25) | 15 (75) | NSa |
| Ophthalmological | 3 (14.3) | 18 (85.7) | 0.009 |
| Otolaryngological | 10 (24.4) | 31 (75.6) | 0.12a |
| Pulmonary | 27 (45) | 33 (55) | NSa |
| Pulmonary infiltrates | 25 (50) | 25 (50) | 0.016a |
| Nodules | 7 (36.8) | 12 (63.2) | NSa |
| Diffuse alveolar haemorrhage | 14 (66.7) | 7 (33.3) | 0.002a |
| Cardiac | 4 (40) | 6 (60) | NSa |
| Digestive | 3 (60) | 2 (40) | NSb |
| Renal | 29 (53.7) | 25 (46.3) | <0.001a |
| RPGN | 12 (60) | 8 (40) | 0.016 |
| Neurological | 12 (35.3) | 22 (64.7) | NSa |
As for steroid use, all patients in whom steroid doses >30 mg per day were used had infections, compared to 33% of those not treated with steroids (p < 0.001).
In terms of overall mortality, in 82/105 subjects 16 patients died (19.5%) during the follow-up period and, in 13 cases, death was related to an infectious episode. No data regarding mortality due to loss to follow-up could be found for 24 subjects.
There was a 14.3% mortality rate linked to the first infectious episode (n = 4); septic shock was the cause in three participants. Another individual receiving treatment with voriconazole due to isolation of Scedosporium apiospermun in the respiratory tract developed pulmonary haemorrhage in association with her underlying disease.
Thirteen/36 infected (37%) and 3/47 uninfected (6%) patients died. According to the χ2 test (p value: .001) (OR: 8.67; 95% CI: 2.03–50.89).
Similarly, there was a logical association between age >65 and mortality. A total of 8/12 over the age of 65 (67%) and 9/74 under 65 (12%) died χ2 test (p-value: .001) (OR: 14.44; 95% CI: 2.99–76.02).
The age-adjusted OR for the association between mortality and infection was 6.26 (1.49–26.39).
In the multivariate analysis of significant variables adjusted for age >65 years, the positive association between infections and the presence of diffuse alveolar haemorrhage persisted, as one of the manifestations of pulmonary involvement adjusted by logistic regression (OR: 3.47; 95% CI: 1.10–10.92; p = .0034) and the presence of renal involvement (OR: 4.55; 95% CI: 1.54–13.42; p = .006) were significantly associated with the presence of infection in this cohort of patients (Table 4).
DiscussionIn our cohort of individuals with systemic necrotising vasculitis, we found a 34.2% prevalence rate of infection. This is consistent with reports from earlier studies. In their publication, Charlier et al. reported 53 major infectious episodes in 35/113 patients diagnosed with GPA (31%), while Fauchais et al. reported 14 major infections in 35 patients diagnosed with GPA (40%).7
Most infections occurred within three months of the diagnosis of vasculitis, during the induction treatment period, with increased exposure to high doses of glucocorticoids and immunosuppressants. Infections were mainly bacterial in origin (67.6%) and the most common foci of infection were respiratory, septicaemia, and urinary tract infections. Debouverie et al., in a cohort of 82 patients, documented a bacterial aetiology in 60% of infectious episodes, with respiratory infections (bronchopneumonia) being the most frequent.5 In their cohort of 132 patients with a median follow-up period of 140 months (96–228), Garcia-Vives et al. observed a total of 300 serious infections, primarily bacterial in origin (87%), which occurred in 60% of the sample during follow-up.18
For our part, we found no difference in the frequency of serious infections between those participants with PR 3-positive AAV vs. MPO positive AAV patients. In a series of 108 patients with AAV, Caballero-Islas et al. described the characteristics and outcomes of those with severe infections classified according to clinical phenotype (non-severe AAV, severe-MPO AAV, severe PR3 AAV) and reported a greater frequency of severe infections in those with vasculitis-related pulmonary involvement and severe PR3 AAV phenotype who received boluses of methylprednisolone. On the other hand, those with severe MPO AAV and severe infections were older and required admission to intensive care units.19
We would highlight the results of the univariate analysis in which age >65 years at diagnosis correlated significantly with high rates of infection, which may be explained by the immunosenescence and higher prevalence of comorbidities in this age group.
Similarly, the association between kidney failure and the presence of infection was significant, given that kidney involvement is, in itself, known to be a risk factor for infection due to a decline in the immune response and because its presence is associated with more severe disease, requiring high doses of glucocorticoids and immunosuppressants.20
On the other hand, the presence of alveolar haemorrhage as an initial manifestation was significantly correlated with infection, possibly linked to the need for initial treatment with high doses of corticosteroids and immunosuppressants in light of the gravity of this manifestation. Juyoungyoo et al. demonstrated that pulmonary symptoms at baseline may be predictive of hospitalisation for infection in a retrospective cohort of 154 patients, due to increased rates of respiratory tract infections due to both bacteria and opportunistic germs.21
We would like to underscore the fact that there were no cases of tuberculosis despite it being an endemic infection in our country and often found in immunocompromised individuals. We regard this as a result of the preventive measures implemented in our centre in conjunction with the Infectious Diseases Department. In fact, cases of latent tuberculosis were detected and adequately treated.
In our study, a BVAS > 15 was associated with a higher incidence of severe infections, in contrast to the results published by Juyoungyoo et al. who found that a BVAS > 20.5 was predictive of hospitalisation for severe infections.21
Insofar as fatality is concerned, we noted a significant association, with infectious episodes being the cause of death in more than half of the cases. In the study by García Vives et al., death was caused by infection in 50% of cases, directly related to infection in 34% of the cases or associated with active disease in 16% of the cases. Participants with severe infections experienced increased all-cause mortality.18
This study has several limitations because of its retrospective nature, which entails an inherent loss of data for analysis, and the small study population. We have not analysed the relationship between infections and cumulative steroid doses or route of administration.
Also of note, we would point out the need for active preventive management and early identification and treatment of infections in patients with necrotising vasculitis, in particular within the first three months of diagnosis, as this time period is a leading cause of mortality, rather than the vasculitis activity per se. Moreover, efforts must continue worldwide toward using lower doses of corticosteroids and maximising protection in older individuals, as well as in those with kidney failure or pulmonary involvement.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank Dr. Enrique Martins, of the laboratory of the Hospital de Alta Complejidad en Red Hospital el Cruce, for his altruistic contribution of the statistical analysis.