To know the situation of ultrasound in Spanish rheumatology.
MethodsA national survey addressed to all rheumatology units in hospitals with at least 200 beds. The questionnaire studied: (a) the availability and the model of the ultrasound equipment, (b) the degree of training, (c) the purpose and areas of ultrasound examination, (d) the usefulness, and (e) the relevance of ultrasound in the training of residents.
Results169 units of the 234 surveyed physicians answered the questionnaire. The availability of ultrasound equipment was high (90%), 38.7% of rheumatologists use ultrasound, although half of the units had a rheumatologist especially dedicated to performing them. Training plans have enabled the incorporation of ultrasound, but there are areas that could be improved. The utility in routine clinical practice was scored at 7.8 (0–10), and ultrasound was integrated in the diagnostic and therapeutic decisions. There is a broad consensus on the need to include ultrasound in the training of residents. Administration is adding ultrasound to the portfolio of specialty services.
ConclusionsIn just 15 years, ultrasound has become available in 90% of rheumatology units from being previously inexistent. Its use is extensive, integrated into clinical practice and linked to the decision making processes. Training plans have been effective, but areas for improvement were identified, and there is a broad consensus on the need to integrate ultrasound in residents’ training.
Conocer la situación de la ecografía en la reumatología española.
Material y métodosEncuesta nacional, dirigida a todas las unidades de reumatología de hospitales con mas de 200 camas. Se investigaba: a) disponibilidad de ecógrafos y tipo; b) grado de formación; c) finalidad y áreas de exploración ecográfica; d) utilidad asistencial, y e) importancia de la ecografía en la formación de residentes.
ResultadosRespondieron 169 unidades de las 234 consultadas. La disponibilidad de equipos de ecografía era alta (90%). El 38.7% de los reumatólogos utilizan el ecógrafo, aunque en la mitad de las unidades existía un reumatólogo especialmente dedicado a realizarlas. Los planes de formación han posibilitado la incorporación de la ecografía, pero se detectan importantes aspectos de mejora. La utilidad en la práctica clínica habitual se valoró en 7.8 (escala 0–10) y la ecografía se integraba en la toma de decisiones diagnósticas y terapéuticas. Es de destacar el amplio consenso sobre la necesidad de incluir la ecografía en la formación de residentes. La Administración está incorporando la ecografía a la cartera de servicios de la especialidad.
ConclusionesEn tan solo 15 años la ecografía ha pasado de la inexistencia, a estar disponible en el 90% de las unidades reumatológicas. Su uso es amplio, integrado en la práctica clínica y vinculado a la toma de decisiones en múltiples procesos. Los planes de formación han sido eficaces, pero se detectan áreas de mejora, y hay un amplio consenso sobre la necesidad de integrarla en la formación MIR.
Ultrasound is a technique recently introduced into the medical specialty of rheumatology. Ultrasound began to be used in our environment in the nineties, promoted by the Board of Directors of the Spanish Society of Rheumatology (SER), who developed a training program, launched in 1996, which remains currently active.1,2
For years, the idea which always defended by rheumatologists and that we had the opportunity to learn and the privilege to practice, is that ultrasound is a very useful tool in the diagnosis and treatment of many of the rheumatic disease. In our opinion and that of many international experts, ultrasound has significant advantages over other imaging techniques, with the possibility of studying the patient in real time and doing so in a safe, fast and efficient way.
Because the beginning of the SER school of ultrasound occurred 15 years ago, it is probably time to put aside individual thoughts and the discussions we have had during this time and see how it has actually influenced the introduction of ultrasound in shaping the clinical practice we now carry in our specialty.
Since no study has systematically investigated the degree of implementation of musculoskeletal ultrasound in rheumatology care units in Spain, the objective of this paper is to analyze the implementation, training and use of ultrasound in the Spanish units of rheumatology and eventually collect the opinions of the teaching units on the role of ultrasound in the formation of our future specialists in rheumatology.
Material and MethodsTo achieve the objective, a survey was designed by a scientific committee that developed the questions and set the universe, after determining that Spain has counted 277 hospitals with over 200 beds. The invitation to participate in the survey was made by e-mail, addressed to the rheumatology department heads, finding reception in 234 different centers, not being possible to locate all of the rheumatology service or department heads, or their mailing address, among other logistical problems. The survey questions were structured attempting to answer the following sections: (a) availability of B-mode and Doppler mode ultrasound (b) level of expertise and training in the ultrasound unit (c) purpose and common areas of ultrasound exploration, (d) value of the contribution of ultrasound to clinical practice, (e) evaluations of interest by the inclusion of ultrasound in medical training of interns and residents (MIR) of rheumatology.
First, the SER task force (ECOSER) sent a personal letter of invitation to participate in the survey to the head of each unit or whoever designated as best suited to answer it. After accepting the invitation, the survey was accessed online through an individual user name and password. The form comprised 3 parts 32, with 50 and 20 issues respectively, reaching a total of 102 questions, which was automatically sent to the database after completion of the form. Only one answer was allowed per site, and was carried out from 15 September to 20 October, 2011. The collected data was treated according to the Protection of Personal Data law 15/1999 of December 13.
Statistical AnalysisA descriptive analysis of each variable was performed, with determination of means, medians and standard deviations where necessary.
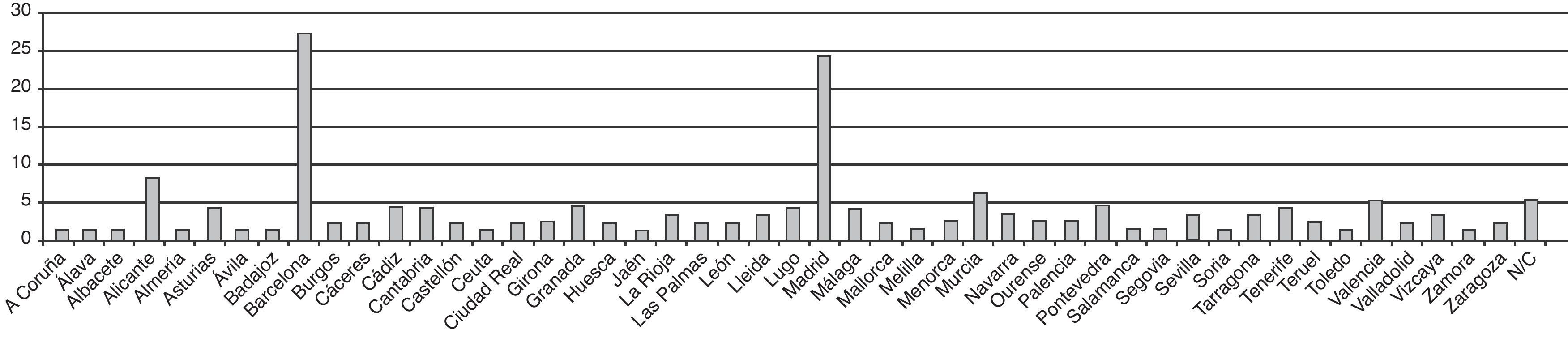
ResultsGeneral InformationOne hundred sixty-nine rheumatology units of the 234 contacted, responded (72%), distributed as 102 persons from 47 provinces (Fig. 1). The average age of rheumatology units was 20.6 years, with a standard deviation of 16.22, and the range was from 51 years to a few months (1960 to July 2011) and a median of 21 years. 117 had their own ward (69%) and 48 did not have it (29%), 2% did not answer this question. The number of rheumatologists in each unit varied from 1 to 17, with a mean of 4.
Ultrasound EquipmentThe availability of ultrasound equipment was high (90%) either because it belongs to the unit or it was being shared with another specialty. One hundred thirty-one of the 169 (77%) units surveyed had their own ultrasound. One hundred and twenty centers (72%) were equipped with Doppler ultrasound. The model was identified in 105 cases, with 18 high-end equipment, others being midrange. Another 22 units (13%) used the scanner from another service; in the case of these units, 17 indicated who owned the scanner, in most cases radiology (71%).
Human ResourcesThe mean number of people responsible for each ultrasound was 1.2. In 47% of the units it was a dedicated rheumatologist sonographer, compared with 46% of the units in which there was not a single person dedicated to this task, it being carried out by several individuals. Seven percent did not answer this section.
In each service, an average of 1.66 rheumatologists used the ultrasound. Compared to the average of each department's rheumatologists, 4.29, we could estimate that an average of 38.7% of rheumatologists used the ultrasound units.
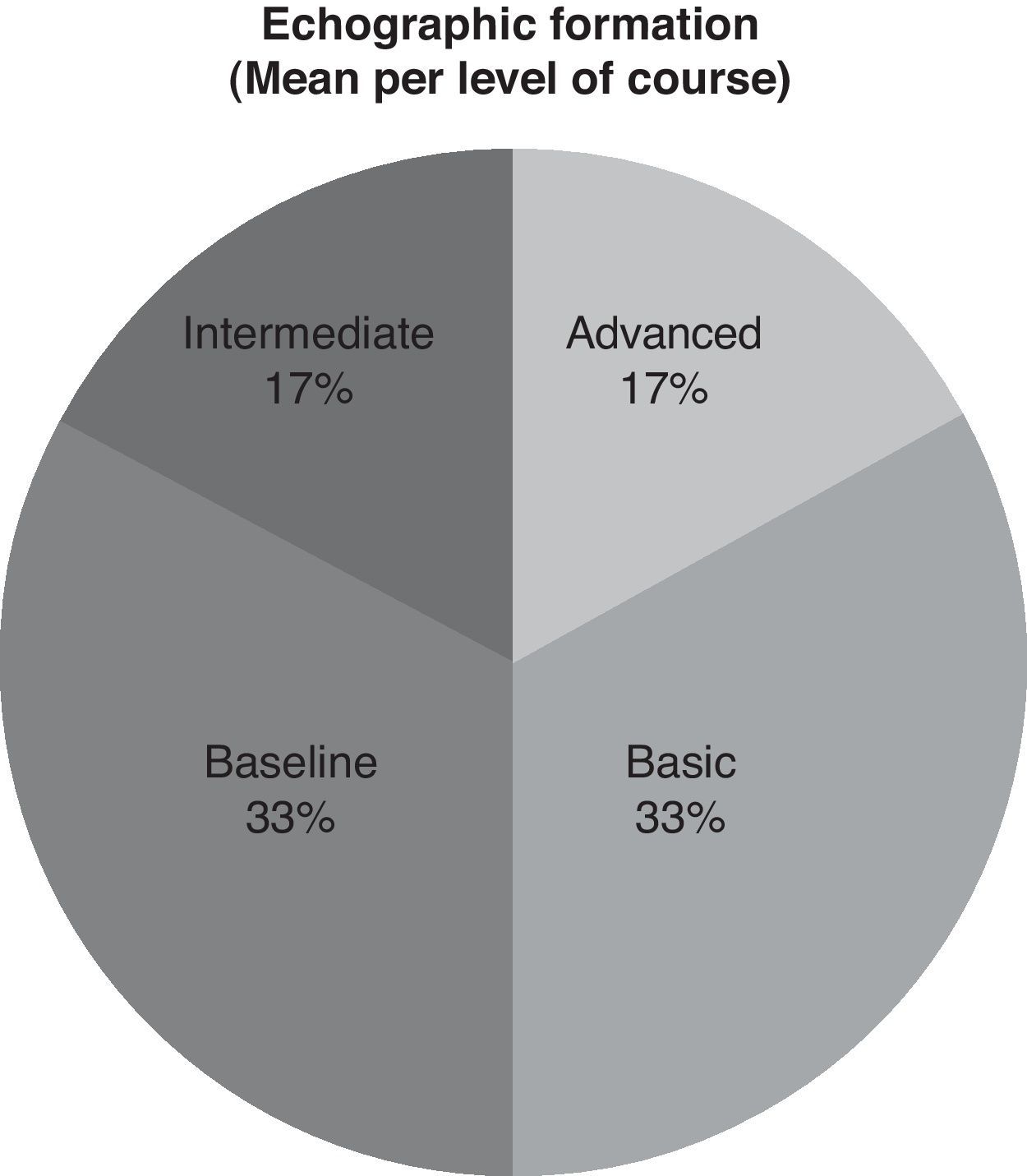
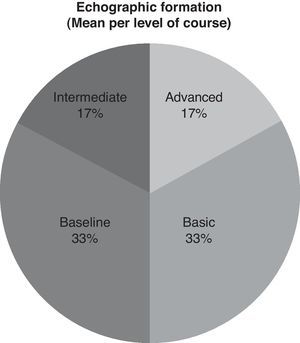
As for the training received by sonographers, 66% of cases had baseline knowledge (33% in each of these levels) and the remaining 34% advanced or intermediate, 17% being the same for each of these two categories (Fig. 2).
Ultrasound as ActivityOnly one-third of the units were referred ultrasound activity within the welfare activities through their own agendas. Twenty-five percent of the units did not answer this question in the rest was done as care activity without being seen as specific activity. In fact, the school management agenda holes reserved for performing ultrasound in 39% of respondents, compared to the remaining 61% that did not, as it is included in the covenant of goals even fewer cases, the 16% of respondents. Thirty-two percent of the units performed ultrasound to other specialties, with a 7% referred to officially as such by the centers while in the remaining 25% was done unofficially. The scans were performed at other specialties in most cases applied by internal medicine (86%).
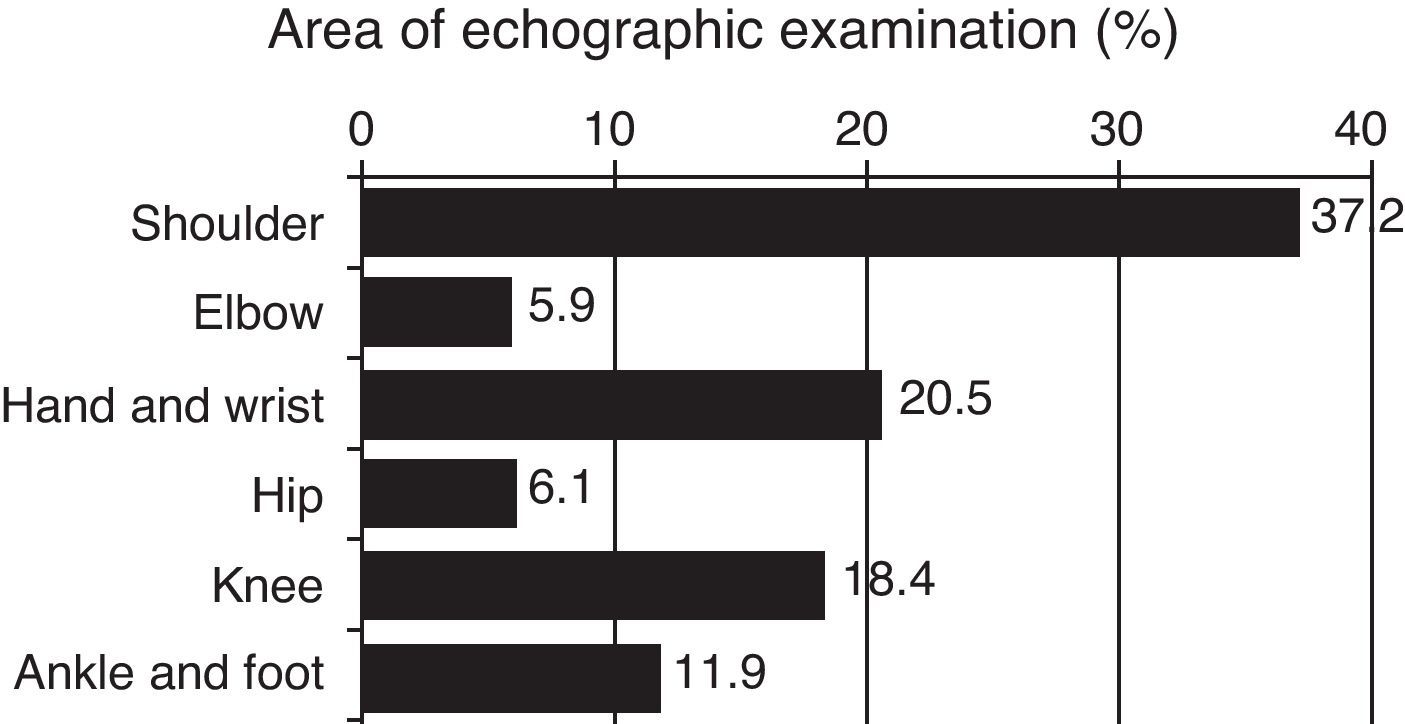
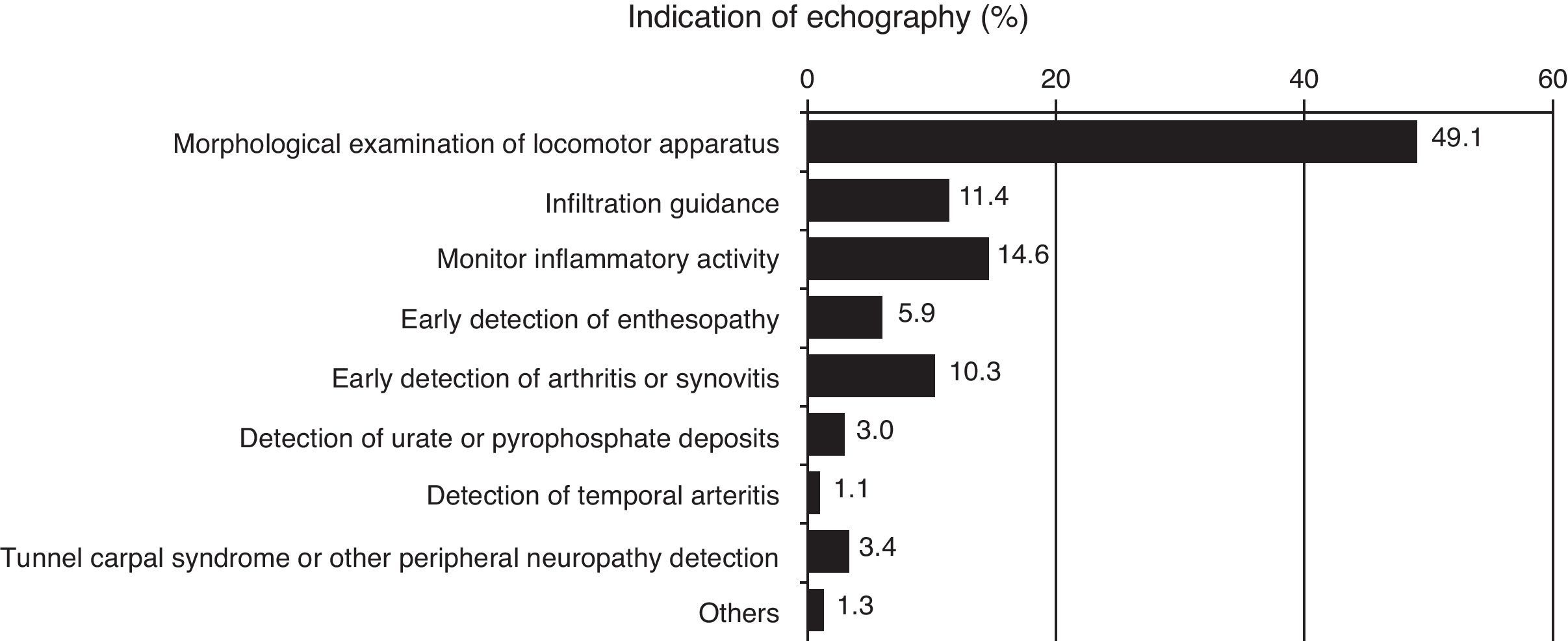
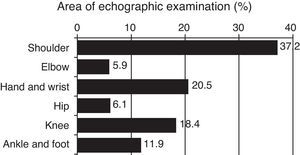
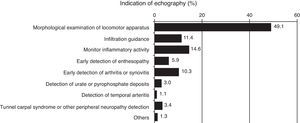
Ultrasound TypeWhen asked what the purpose of ultrasound was, the survey responses are shown in Figs. 3 and 4, in which a number is assigned to each of the different possibilities per 100 scans made.
UtilityIn the section determined to see the utility of ultrasound in clinical practice, respondents responded on a continuous scale from 0 to 10 (where 0=no importance and 10=highest importance), and the average relevance of the addition of ultrasound to the rheumatology unit being 7.8.
MIR Training in UltrasoundAs a group, residents had training in MIR rheumatology in 45 units, representing those who responded to the survey, or 100% of the academic units of our country.
Among teaching hospitals with MIR programs in rheumatology, ultrasound training was included in 21 vs 45 which had residents, which means that only 46.7% residents had specific training in this technique in the unit itself.
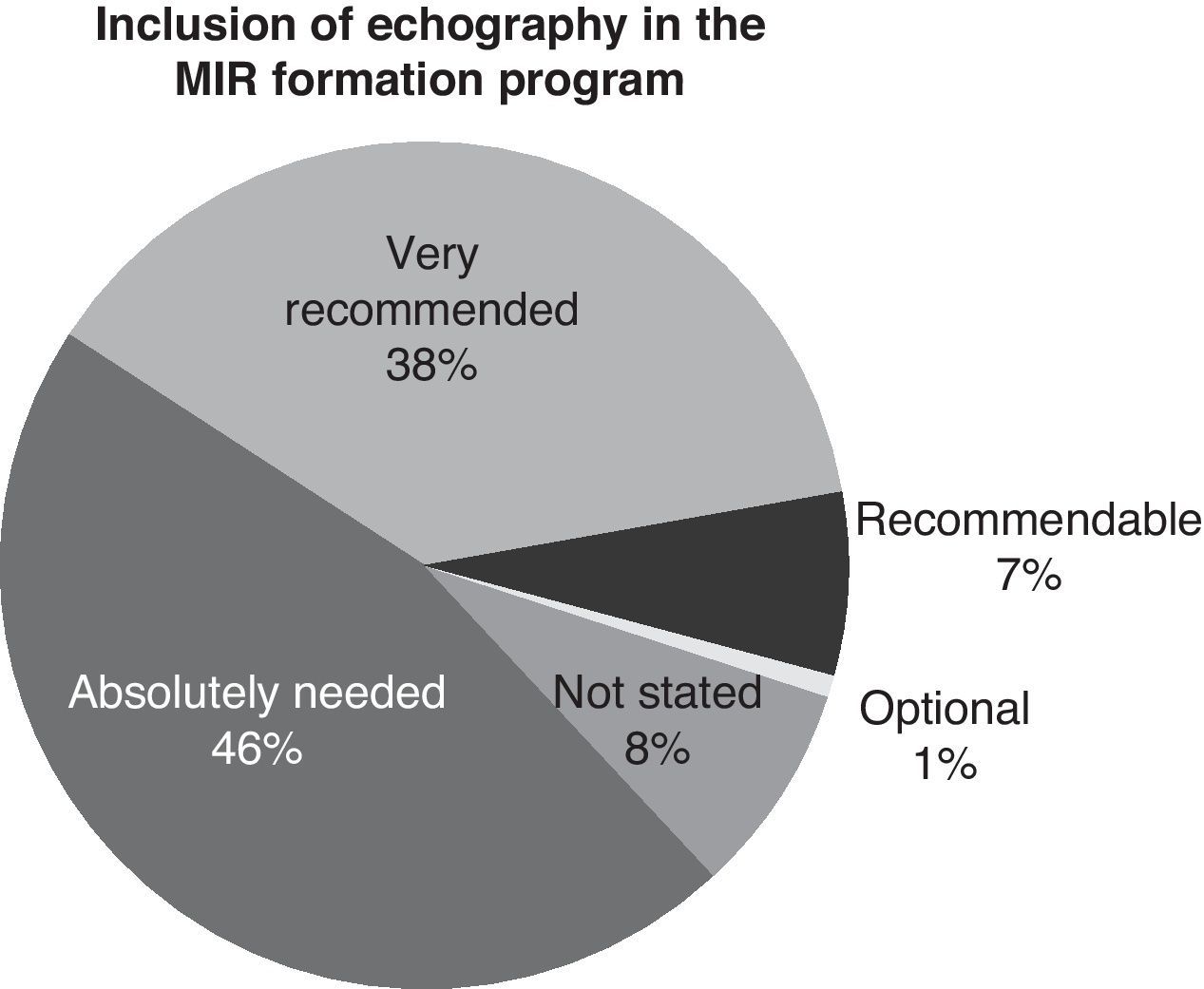
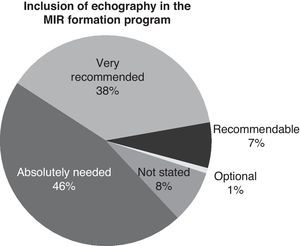
As to the question of what level of importance was given to the addition of ultrasound training in MIR, the results shown in Fig. 5 show that a majority had interests that included musculoskeletal ultrasound training programs related to the MIR, given that 91% were in favor of their inclusion.
DiscussionUltrasonography in rheumatology has emerged strongly in recent years. For a while its growth relied on a limited number of rheumatologists, enthusiastic pioneers who believed and practiced this technique and receiving strategic support of SER and the pharmaceutical industry, which developed an important role both in sponsorship training plans and in the purchase of equipment. Discussions have multiplied in our congress and the positions for and against have been probably changed over the years. Increasingly there have been numerous publications that have deepened the guidelines standardization and shown their validity, reproducibility and factibility.3–8
With the passage of 15 years since the first BE ultrasound course, it seemed interesting to analyze its results to quantify what has been the impact of training and what is the real situation in our country regarding rheumatological ultrasound, both from the point of view of both teachers and those in charge of assistance care. This type of analysis is fundamental if we want to know whether we do get results, and to plan possible actions or identify opportunities for improvement.
It should be noted that the response rate has been high, with 169 units that have completed the questionnaire, which makes the results can be considered representative and adequate geographical distribution. It should be noted that the availability of ultrasound in our units is high, reaching between equipment owned or shared 90% of total units. The teams are mostly mid-range or high, which is found to apply to clinical practice. In the area of human resources is interesting how on the one hand some units have promoted a dedicated or rheumatologist is specially trained to do ultrasound and how it coexists with another model in which multiple rheumatologists are able to do ultrasounds within the unit, both models even coexist in some units.
As for government, two readings can be made, one would be that, first, it only recognizes the ultrasound within the portfolio of specialty services, in 39% of cases. The other reading is that, despite the short time ultrasound has seen activity, 39% of centers have their activity defined as a distinct area. For the healthcare system, a technique considered standard practice would need to have been incorporated into the daily activities and accepted as valid and useful for practitioners. In this regard, we note that probably 80% of ultrasound units have been established in the last 6 or 7 years, which is a short time to be recognized by a health organization. In any case, this data can help health authorities demonstrate the importance of this technique in relation to our specialty. The concept of usefulness in clinical practice is reflected in the results, with a rating of 7.8 on a scale of 0–10 and, as seen in Fig. 4, ultrasound is closely used to making diagnostic and therapeutic decisions.
In the field of resident training it should be noted that, in the majority of sonographers, it is probably insufficient (or just basic introductory courses), and although these may have been complemented with training in symposia, conferences and specific courses, this is an area of improvement that needs attention. It is also noted that the survey reflects a state of opinion, because actually the Ultrasound School has formed in the last 5 years at least 60 rheumatologists at an advanced level and more than 120 in a middle level, making the survey reflect a greater desire for knowledge, not exactly a lack thereof, and in this respect note that the gap between supply and demand for training, recently quantified, is small.1 Also in the field of training, we should emphasize that the broad consensus is on the need to include ultrasound in a field integrated into MIR. It should be remembered that, currently, musculoskeletal ultrasound is not recognized as an essential technique, but between of its importance as a highly recommended techniques in the formation of a rheumatologist, the SAS/2855/2009 order of 9 October, approved and published the training program for the specialty of Rheumatology. Currently, the units are adapting their training, so that they may have their own training or rotation or can use other units or training schools sponsored by the SER with special programs for residents. However, it should be noted that almost half the units’ accredited teachers consider technology as essential knowledge for new rheumatologists, i.e. above the level proposed by the Ministry, a substantial change considering their position in 1996.
As limitations, we should note that the survey was intended only for hospitals over 200 beds, which could not represent outpatient care. In this regard, we note that some exceptions were made for minor private rheumatology practices in health areas attached to a hospital. That is, in this sense the survey is representative and that even private practice has, in most cases, public sector professionals that perform both functions, so their opinion was reasonably collected. Another limitation is that of the 277 centers surveyed, only 169 responses were obtained (61%); however, we must bear in mind that some of these centers are not exclusively dedicated to rheumatology and not included as a specialty, so the results were calculated with the 234 centers contacted, which would put the response rate at 72%, which may be acceptable while drawing conclusions.
In conclusion, the results show how ultrasound has gone in 15 years from non-existence to being implemented in almost all rheumatology units, its use is broad, including not only soft tissue or isolated joint scans, but used in making diagnostic and therapeutic decisions in various diseases, and training plans seem to have made possible the incorporation of ultrasound into clinical practice, but training still has considerable improvement opportunities, and in this sense, it is important to incorporate the views of MIR specialty training. Finally, in terms of administration, it appears that ultrasound is progressively being incorporated to the portfolio of specialty services.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of InterestAbbott Laboratories have made this study possible thanks to their logistical support without any intervention on the result analysis or on the manuscript itself.
To all of the participating rheumatologists and units.
Please, cite this article as: De Miguel E, et al. Situación de la ecografía en la reumatología española 2012. Reumatol Clin. 2012;8:310–14.