Fibromyalgia is a chronic disease of unknown etiology characterized by widespread muscle pain, with occupational, familial, social, physical and psychological performance involvement. The multidisciplinary approach to the disease leads to improvement in quality of life and symptomatology.
ObjectivesTo evaluate the improvement of activities of daily living (ADL) and quality of life following a multidisciplinary intervention (Health Primary Care and Occupational Therapy).
Materials and methodsPretest–posttest study performed with a simple random sample of 21 patients with fibromyalgia (range 16–55 years). The measurement was performed with the Barthel scale (ADL), the scale of Lawton and Brody (IADL), the FIQ questionnaire, and no standardized surveys to assess the pre- and post-intervention situation. An intervention on motor skills (basic motor skills, pool exercise, outdoor exercise, restructuring, occupational performance and graded activity and intervention in ADL) was performed, combining pharmacological control of their symptoms and treatment.
Results and conclusionsFibromyalgia patients are not fully satisfied with their treatment; Primary Care receives a score of 6.89, and Hospital Care 5.79, improving the Barthel, Lawton and Brody and FIQ indexes, being statistically significant (P<.05). After the combined procedure the number of independent women in ADL and IADL increases.
La fibromialgia es una enfermedad crónica de etiología desconocida, caracterizada por dolor muscular generalizado, afectando al desempeño ocupacional, familiar, social, físico y psicológico. El abordaje multidisciplinar de la enfermedad aporta mejoría en la calidad de vida y sintomatología del paciente.
ObjetivosValorar la mejoría de actividades de la vida diaria (AVD) y calidad de vida tras una intervención multidisciplinar (Atención Primaria y Terapia Ocupacional).
Material y métodoEstudio pretest-postest, con muestreo aleatorio simple, en 21 pacientes con fibromialgia (rango 16–55 años). La medición se realiza con la escala de Barthel (ABVD), la escala de Lawton y Brody (AIVD), cuestionario FIQ y encuestas no estandarizadas para valorar situación pre y postintervención. Se realizó una intervención sobre psicomotricidad (psicomotricidad básica, ejercicio en piscina, ejercicio al aire libre, reestructuración, desempeño ocupacional y actividad graduada e intervención en ABVD), asociando control farmacológico de su sintomatología y tratamiento.
Resultados y conclusionesLos enfermos de fibromialgia no están totalmente conformes con el tratamiento que reciben, Atención Primaria recibe una valoración de 6,89, y la Atención Hospitalaria de 5,79, mejorando los índices de Barthel y de Lawton y Brody, y el cuestionario FIQ, de forma estadísticamente significativa (p<0,05). Tras la intervención combinada, aumenta el número de mujeres independientes en ABVD y AIVD.
Fibromyalgia (FM) is a chronic disabling disease of unknown etiology1 whose main symptom is widespread pain, followed by fatigue and lack of sleep. It represents an emerging health problem, with a prevalence between 3% and 6% of the worldwide population; most patients present it between 20 and 50 years of age, and it is more common in women, with a male to female ratio of 16:10.2 It occupies 15% of the demand for outpatient care of Rheumatology and 5%–10% of primary care visits,3 leading to an approximate expenditure of 11000 million euros/year in Spain, both in direct and indirect costs.4
The5 scientific-technical approach is very limited, needing a biopsychosocial approach to the disease, as well as adjunctive therapies such as6 aerobic exercise, strength training, stretching or flexibility, cognitive behavioral therapy, meditation and feedback7; the goal is for each individual to know their various physiological stimuli, with the possibility to modify them in their favor, and practice and learn to control them better.8 Occupational Therapy is a useful tool because it has effects on occupational functioning, cognitive and physical skills, resulting in improved performance of activities of daily life and more interaction with the global context.
The effectiveness of multidisciplinary management is currently being evaluated in order to provide the most comprehensive care for this difficult and complex group of patients9 and an improvement in their daily lives, both in quality of life and independent or dependent mild activities of daily living as well as moderate activities of daily living (ADL), and for moderate dependent instrumental activities of daily living (IADL).10
The objective of this study is to evaluate the effect of a multidisciplinary intervention in patients with FM.
Materials and MethodsSampleIn a population in the Health Area of Talavera de la Reina (Toledo), with 128000 inhabitants, with a prevalence of FM of 2.4%,11 a confidence interval of 95% and a margin of error of 7%, we obtained a sample size of 19 people (3.0 Epidat Program), to which we added the non-response rate of 10% from a direct interview, obtaining a total of 21 people on a database of 446 patients with FM, all with a hospital diagnosis performed in the rheumatology clinic. Participants were contacted by telephone interview, informing them of the type of study.
Inclusion CriteriaWomen between 16 and 55 years, residing in the Health Area of Talavera de la Reina (Toledo) with FM who have no other problem that causes them mental or physical disability.
Exclusion CriteriaOther physical illnesses that hinder intervention and have not featured, in the 6 months prior, major life events (bereavement, moving, etc.).
MeasurementsWe used the Fibromyalgia Impact Questionnaire (FIQ)9 designed to quantify the overall impact of FM on several dimensions (functionality, perception of pain, stiffness and fatigue, sleep disorder, depression, anxiety and ability to work in paid and domestic labor). In the case of having gainful employment, the FIQ assesses the degree to which FM has affected this activity.12 The assessment of the daily impact of FM was performed by the IADL, which are those activities that support everyday life at home and in the community, that may require more complex interactions than those used in ADL (Lawton and Brody scale).13 For those ADL designed to personal care,14 the Barthel scale was used. For the perception of the disease and the health system related to FM, we used a questionnaire created ad hoc (Appendix 1 [available online]).
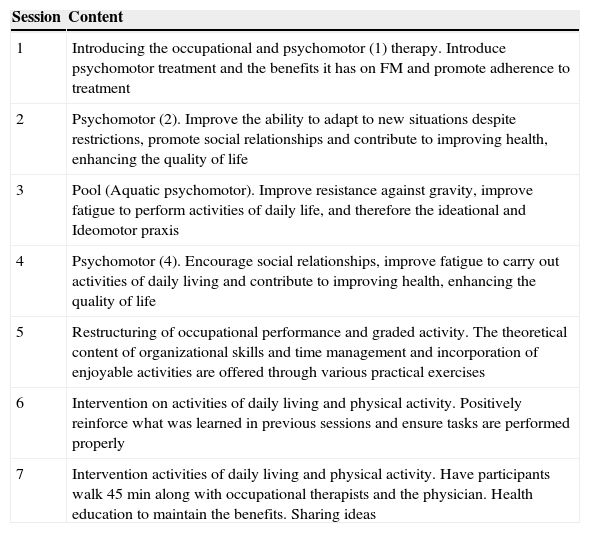
Design and InterventionPretest–posttest study performed with simple random sampling using the Wilcoxon test, and the statistical analysis with SPSS 15.0. Only patients who attended at least 5 of the 7 sessions were analyzed. The study was conducted between February and May 2012 and consisted of 2 parts. The first part was done by examination in primary care with 3 appointments (before, during and after the intervention), in which the patients spoke of their disease, treatment of their symptoms (analgesics, tramadol, paracetamol, pregabalin and/or ciclobenzapirine) as well as their usual medication for concomitant diseases, and conducting health education in FM, and occupational therapy sessions, with 7 sessions of between 60 and 120min (Table 1).
Occupational Therapy Sessions and Content.
| Session | Content |
|---|---|
| 1 | Introducing the occupational and psychomotor (1) therapy. Introduce psychomotor treatment and the benefits it has on FM and promote adherence to treatment |
| 2 | Psychomotor (2). Improve the ability to adapt to new situations despite restrictions, promote social relationships and contribute to improving health, enhancing the quality of life |
| 3 | Pool (Aquatic psychomotor). Improve resistance against gravity, improve fatigue to perform activities of daily life, and therefore the ideational and Ideomotor praxis |
| 4 | Psychomotor (4). Encourage social relationships, improve fatigue to carry out activities of daily living and contribute to improving health, enhancing the quality of life |
| 5 | Restructuring of occupational performance and graded activity. The theoretical content of organizational skills and time management and incorporation of enjoyable activities are offered through various practical exercises |
| 6 | Intervention on activities of daily living and physical activity. Positively reinforce what was learned in previous sessions and ensure tasks are performed properly |
| 7 | Intervention activities of daily living and physical activity. Have participants walk 45min along with occupational therapists and the physician. Health education to maintain the benefits. Sharing ideas |
All participants were requested verbal consent. The project was approved by the Research Committee of the Health Care District of Talavera de la Reina.
ResultsResponse was obtained from 20 patients with a mean age of 40 years (range 16–55 years). In a previous survey, when asked on knowledge of occupational therapy, 50% answered yes. 75% knew about psychomotor therapy. 95% of patients believed that an intervention from Occupational Therapy helped FM and, when asked whether they found improvement with treatment received before surgery, 70% responded no. 10% answered that almost always other people took seriously their disease, 55% said sometimes, 25% almost never and 10% never. As to whether doctors take seriously all presenting symptoms, 10% answered always, 10% almost always, 60% sometimes and 20% rarely.
The work of the primary care physician was viewed more positively than the Hospital Care Physician, with a difference of nearly a point on an analog scale of 0–10, in which the GP got a 6.89 and hospitalist care 5.79. 100% of FM patients fully consider that their needs are not met, but consider that public health helps. The family was, for 50% of the patients, who most understood them, followed by other patients with FM 25%, and 10% healthcare professionals.
In the post-survey, all participants thought that the intervention helped them and should be included within the treatment they currently receive.
The initial quality of life (QOL) of the study group was of 74.41 (range 63.0–93.8) placing them in the FIQ as vital moderate (50–75) to severe involvement (>75). After the speech, the QOL minimum was 36.09 (mild vital involvement) and a maximum of 60.61 (moderate vital involvement), showing a clear improvement in the overall health, so a degree of involvement of QOL as measured by the FIQ, goes from moderate to severe to moderate to mild, with a statistically significant difference (P<.05).
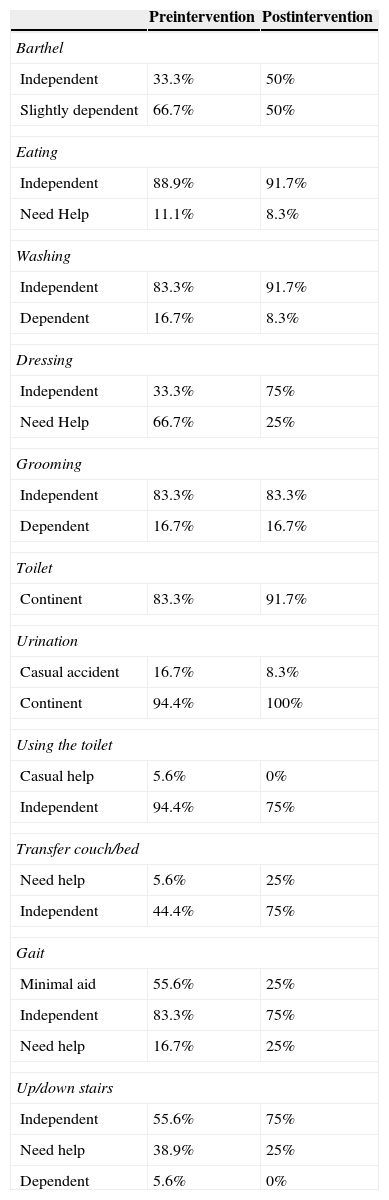
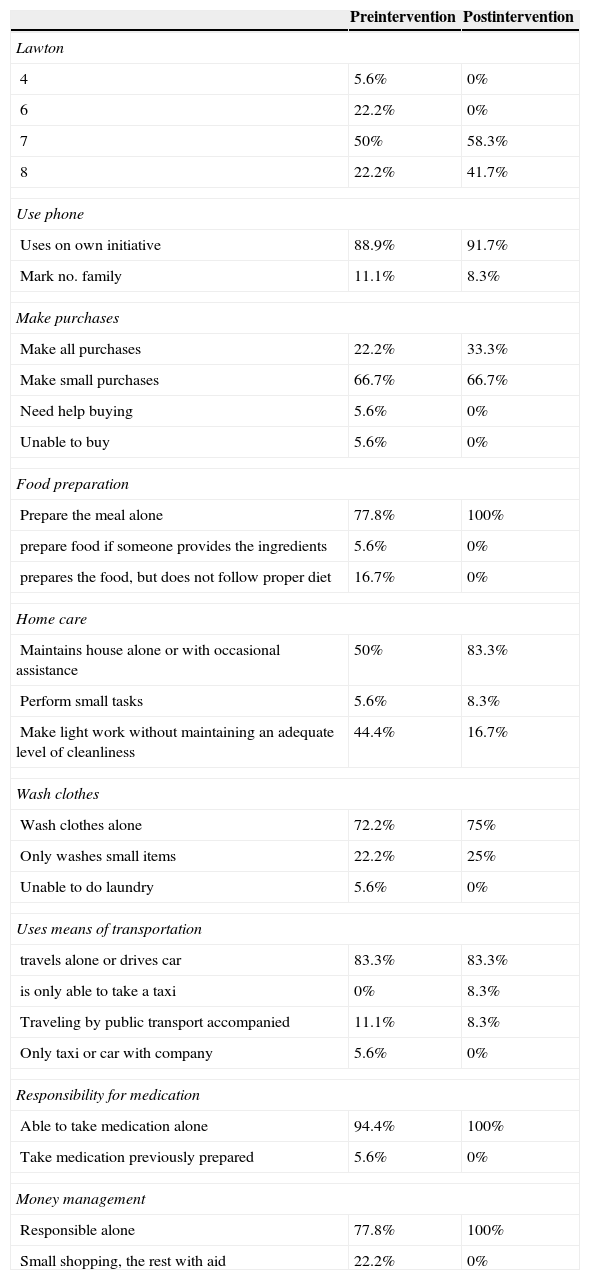
Regarding the degree of independence in ADL, in the pre-intervention study, 33.3% of patients were independent and 66.7% has a slight dependence, and subsequently 50% of them were independent, and 50% had mild dependence (Table 2). Regarding the degree of independence in IADL, of those participating in the pre-intervention study, 22.2% had a score of 8, 50% had a rating of 7, 22.2% a rating of 6 and 5.6% a rating of 4. The scale of Lawton and Brody is most useful for women, as many men did not realize some of the activities studied. In the subsequent evaluation, 41.7% had a score of 8 and 58.3% a rating of 7 (Table 3).
Results of the Barthel Pre-Intervention and Post-Intervention Scale.
| Preintervention | Postintervention | |
|---|---|---|
| Barthel | ||
| Independent | 33.3% | 50% |
| Slightly dependent | 66.7% | 50% |
| Eating | ||
| Independent | 88.9% | 91.7% |
| Need Help | 11.1% | 8.3% |
| Washing | ||
| Independent | 83.3% | 91.7% |
| Dependent | 16.7% | 8.3% |
| Dressing | ||
| Independent | 33.3% | 75% |
| Need Help | 66.7% | 25% |
| Grooming | ||
| Independent | 83.3% | 83.3% |
| Dependent | 16.7% | 16.7% |
| Toilet | ||
| Continent | 83.3% | 91.7% |
| Urination | ||
| Casual accident | 16.7% | 8.3% |
| Continent | 94.4% | 100% |
| Using the toilet | ||
| Casual help | 5.6% | 0% |
| Independent | 94.4% | 75% |
| Transfer couch/bed | ||
| Need help | 5.6% | 25% |
| Independent | 44.4% | 75% |
| Gait | ||
| Minimal aid | 55.6% | 25% |
| Independent | 83.3% | 75% |
| Need help | 16.7% | 25% |
| Up/down stairs | ||
| Independent | 55.6% | 75% |
| Need help | 38.9% | 25% |
| Dependent | 5.6% | 0% |
Results of the Lawton and Brody Preintervention and Postintervention Scale.
| Preintervention | Postintervention | |
|---|---|---|
| Lawton | ||
| 4 | 5.6% | 0% |
| 6 | 22.2% | 0% |
| 7 | 50% | 58.3% |
| 8 | 22.2% | 41.7% |
| Use phone | ||
| Uses on own initiative | 88.9% | 91.7% |
| Mark no. family | 11.1% | 8.3% |
| Make purchases | ||
| Make all purchases | 22.2% | 33.3% |
| Make small purchases | 66.7% | 66.7% |
| Need help buying | 5.6% | 0% |
| Unable to buy | 5.6% | 0% |
| Food preparation | ||
| Prepare the meal alone | 77.8% | 100% |
| prepare food if someone provides the ingredients | 5.6% | 0% |
| prepares the food, but does not follow proper diet | 16.7% | 0% |
| Home care | ||
| Maintains house alone or with occasional assistance | 50% | 83.3% |
| Perform small tasks | 5.6% | 8.3% |
| Make light work without maintaining an adequate level of cleanliness | 44.4% | 16.7% |
| Wash clothes | ||
| Wash clothes alone | 72.2% | 75% |
| Only washes small items | 22.2% | 25% |
| Unable to do laundry | 5.6% | 0% |
| Uses means of transportation | ||
| travels alone or drives car | 83.3% | 83.3% |
| is only able to take a taxi | 0% | 8.3% |
| Traveling by public transport accompanied | 11.1% | 8.3% |
| Only taxi or car with company | 5.6% | 0% |
| Responsibility for medication | ||
| Able to take medication alone | 94.4% | 100% |
| Take medication previously prepared | 5.6% | 0% |
| Money management | ||
| Responsible alone | 77.8% | 100% |
| Small shopping, the rest with aid | 22.2% | 0% |
There were statistically significant differences in pre-post intervention in ADL, IADL and QOL (P<.05).
DiscussionFM is a highly prevalent and disabling disease11 which, together with the high demand in the clinics, both primary care and Hospital Care (20% of consultations of Rheumatology),15 and expenditure per patient per year poses an important expense to the health system (€10 000 patient year). Patients were classified as a difficult approach, largely due to non-existence of an actual cure.15
Most of the people who participated in the study expressed a social inadequacy and misunderstanding about their disease; 90% stated that the people around them are not serious about their disease, causing them difficulties in their daily lives.
Some of the most affected parameters in people with FM ADL are sleep and rest,16 leading to insomnia at night, which causes tiredness on waking in the morning.
The ADL disabilities that were more common were going up and down stairs, and in the most affected in people with FM, the AIVD most affected was “shopping”, which assures us the dependence of these patients and their limitations in daily life, which is inherent in their illness.
In our statement, we released a set of guidelines from the Occupational Therapy and psychomotor aspects to exercise the mind, while moderate exercise, demonstrated as beneficial in this disease.6,15
After this study, despite not having, (limitation of the study), a control group by the difficulty to obtain controls to these particular cases, it has been shown that the combined multidisciplinary intervention significantly improved (P<.05) quality of life, as in the embodiment of the people affected in their ADL due to FM and, therefore, the effectiveness of the combined multidisciplinary therapy to treat this disease is demonstrated.
With this multidisciplinary approach we approximate the current problem, in which the Hospital Care physician (mainly Rheumatology) reaches the diagnosis, monitors and treats the disease, prolonging the reviews in time, acting on cases of exacerbation and worsening of the disease and working with primary care physicians in maintaining the health status of the patient, helping other health professionals (occupational therapists, psychologists, physiotherapists, etc.) and thus opening the door for future research with more time on this approach.
Drug treatment has failed to be, by itself, the treatment of choice for treating FM (90% doubt that the health system takes seriously their disease), although many others have been tested.15 Currently, drug treatment is the only option used from the health system perspective and this means that people with FM are unhappy with the system, even raising questions about whether doctors believe their illness. Non-pharmacologic treatments have demonstrated their effectiveness, such as physical exercise, psychotherapy, feedback and occupational Therapy.6–8 However, they do not appear in the portfolio of health systems, translating into an increased workload in healthcare. This lack in resources is one of the reasons why people with FM are not fully addressed by the system.15
These results support the idea that the treatment of FM should be done from17–21 a multidisciplinary perspective, not only pharmacological medical treatment, supported by scientific evidence and directed mainly by Rheumatology, but by primary care as well, and that treatment should be a cofactor in the disease, including other types of treatment, be it psychiatric, psychological or from the Occupational Therapy and Physiotherapy perspctive.16 To treat these patients it is not enough to have a unique approach; it must be approached from several levels, such as social, personal and family, helping the sick and their environment, making a biopsychosocial approach to the disease and not reducing us to a medical approach.15 Fibromyalgia is not a muscle or a bone breaking, it is a person who suffers from a crippling disease.
The multidisciplinary team, supported in primary care due to their closeness, trust and patient accessibility, make it the axis of maintenance treatment, using a biopsychosocial approach. In patients with FM it is demonstrated that a multidisciplinary intervention approach significantly improves their quality of life and performance.
Ethical ResponsibilitiesProtection of persons and animalsThe authors declare that the performed procedures conformed to the ethical standards of the committee responsible for human experimentation and were in accordance with the World Medical Association Declaration of Helsinki.
Data confidentialityThe authors state that patient data do not appear in this article.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors have no disclosures to make.
Please cite this article as: Gonzalez Gonzalez J, del Teso Rubio MM, Waliño Paniagua CN, Criado-Alvarez JJ, Sanchez Holgado J. Tratamiento sintomático y del dolor en fibromialgia mediante abordaje multidisciplinar desde Atención Primaria. Reumatol Clin. 2015;11:22–26.