Chronic recurrent multifocal osteomyelitis (CRMO) is a rare idiopathic inflammatory disease that affects mainly children and young adults, resulting in significant morbidity especially if not diagnosed early. The clinical signs and symptoms are nonspecific, with a consequential delay in diagnosis. Radiological and histopathological criteria are important for its definition. Two cases of CRMO are reported, highlighting the diagnostic challenge and demonstrating the importance of timely investigations.
La osteomielitis multifocal recurrente crónica (CRMO) es una enfermedad inflamatoria idiopática rara que afecta a principalmente niños y adultos jóvenes, dando por resultado morbosidad significativa sobre todo si no se diagnostica a tiempo. Los signos y síntomas clínicos son inespecíficos, entorpecer y retrasar el diagnóstico. Las pruebas radiológicas e histopatológicas son esenciales para su definición. Se divulgan dos casos de CRMO, destacando el reto diagnóstico y demostrando la importancia de las investigaciones oportunas.
Chronic recurrent multifocal osteomyelitis (CRMO) is an idiopathic auto-inflammatory disorder of undefined origin affecting mainly children and young adolescent.1,2 Although, recent findings suggest the possibility of an abnormal regulation of IL-1β axis been involved in the pathogenesis, this is yet to be fully elucidated.3,4
It is considered a rare disorder, but its incidence is probably underestimated, with some studies demonstrating that CRMO could be more common than previously reported,5 with a comparable incidence with bacterial osteomyelitis in a 10-year retrospective study involving 105 children in Germany.6
This disease is generally benign but tends to follow a chronic or recurrent course, often the course is prolonged over several years with periodic exacerbations.7,8 It is generally regarded as benign, however complications have been reported in children and adolescence. These could be variable, from mild to debilitating asymmetries of limb length, vertebral collapse kyphosis, chronic spondylo-arthropathy, and stunting for early closure of the growth-cartilages.9 Therefore a correct and timely diagnosis is of utmost importance to reduce morbidity.
Here, we describe two cases of CRMO and demonstrate diagnostic features which help differentiate between bacteria osteomyelitis and CRMO.
Case PresentationCase 111 year-old referred with 3 months history of persistent left foot pain, associated with swelling, redness and some difficulty in weight bearing. There was a preceding history of fall, 4 weeks prior to the onset of this pain from a height but no penetrating injury. Apart from tonsillectomy at the age of 6, the past medical history was unremarkable. She last travel to Asia 2 years before the onset of this symptoms, and has been appropriately immunised for age with no significant medical and family history.
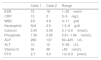
She examined well and appropriately grown for her age. She was unable to weight bear on her left foot, which was swollen, warm, and tender. The initial radiological investigations were reported as unremarkable with a normal metabolic bone profile. The inflammatory markers were persistently elevated with a peak Erythrocyte sedimentation rate (ESR) of 73mm/h and C-reactive protein (CRP) of 15mg/L (Table 1). Three weeks later, due to persistent pain, the X-ray was repeated (Fig. 1a) and followed by CT and MRI showing hyperintensity within the third metatarsal shaft, circumferential cortical thickening and periostitis. No penumbra sign was seen to suggest an abscess. She had serial radiological investigations, follow-up and was regularly discussed at the regional sarcoma multidisciplinary team (MDT) meeting. Due to deteriorating lesion on the images, a biopsy was obtained and commenced on a 6 weeks course of antibiotics with no improvement. The microscopy, culture and sensitivity (MCS), mycobacterium tuberculosis (TB) culture and polymerase chain reaction (PCR) for staphylococcus, streptococcus and kingella kingae were all negative. There was no clinical or radiological response to antibiotics.
Laboratory Results of Case 1 and 2.
| Case 1 | Case 2 | Range | |
|---|---|---|---|
| ESR | 73 | 16 | 1–20mm/h |
| CRP | 15 | 2 | 0–5mg/L |
| WBC | 8.5 | 4.8 | 4–11g/dl |
| Neutrophils | N/A | 2.5 | 1.5–8g/dl |
| Calcium | 2.40 | 2.59 | 2.1–2.6mmol/L |
| Phosphate | 1.56 | 0.95 | 0.81–1.94mmol/L |
| ALP | 266 | 137 | 60–425U/L |
| ALT | 10 | 12 | 0–36U/L |
| Vitamin D | 36 | 38 | >50nmol/L |
| PTH | 2.7 | 3.4 | 1.6–6.9pmol/L |
(a) X-ray of the right foot showing a focus of lucency in the distal metaphysis of the third metatarsal, extending to the growth plate with multi-lamellated periosteal reaction (b). MRI of the right ankle showing diffuse bone marrow oedema, fibular periosteal response, the localised medial fibular cortical defect and the tibiotalar joint effusion.
A whole body MRI allowed the diagnosis of CRMO. The patient received pamidronate infusion, with improvement in the leg lesion and reduction in pain. Her gait returned to normal, her pain settled and her radiographs showed remodelling of the metatarsal gradually over the following year.
Case 213 year-old previously fit and well male teenager was referred with 5 years of right ankle pain and swelling. There was no preceding history of trauma and no other constitutional symptoms. No associated pain or swelling in any other joints. Apart from hay fever, there was no significant past medical and family history of note. He was born at term with no developmental concern and fully immunise for age.
He examined well with a weight of 70kg, height 182cm and BMI of 21.3. Apart from right ankle swelling and tenderness on palpation, the rest of the physical examination was unremarkable. The initial X-ray at the referring hospital was reported as normal. He had insufficient vitamin D of 38nmol/L but the rest of the metabolic bone profile, including the renal functions, liver function and full blood counts were all normal. The ESR was slightly elevated at 16mm/h with a normal CRP of 2mg/L (Table 1). The X-ray and MRI series were subsequently reviewed at our MDT meeting and demonstrate diffuse bone marrow oedema, fibular periosteal response, localised medial fibular cortical defect and large tibiotalar joint effusion of the right distal fibula (Fig. 1b). Underwent joint aspirate, bone biopsy, debridement and sequestrectomy. The microscopy culture and sensitivity (MCS), polymerase chain reaction (PCR) for streptococcus, staphylococcus and kingella kingae, including culture for mycobacterium tuberculosis of the bone biopsy and joint fluid were all negative. The histopathology showed mild oedema and mild chronic inflammatory cellular infiltrate composed of lymphocytes and plasma cells. There is no evidence of granulomata or atypical cells to suggest malignancy. The base line immunological and auto-immune work up was also negative. He had a 6 week course of antibiotics due to worsening of the lesion with no improvement. The whole body MRI allowed for the diagnosis of CRMO. He received pamidronate infusion with significant improvement in the leg lesions and reduction in pain.
DiscussionThis case series highlight CRMO as a well-known differential diagnosis of bacterial osteomyelitis and the clinical manifestations are highly variable.10 The clinical presentation of warmth and redness in the context of swelling and pain makes it difficult to exclude bacterial osteomyelitis. Although swelling is a less prominent feature of bacteria osteomyelitis, it is not uncommon for it to be complicated by septic arthritis of the preceding joints. The absence of fever has generally been used as a discriminatory symptoms/signs. However, few studies have observed a mild to moderate fever in children with CRMO.9,11 We did not observe extra-articular manifestation, which has been reported in 20% of children presenting with CRMO and particularly helpful in the diagnosis of CRMO, but the insidious onset of the symptoms and signs couple with the fact that both children appeared well was consistent with previous studies and is typical of CRMO.11
Although, the lesion may affect any bone segment, the predilection for the lower extremities has been well documented, especially the metaphysis of long bone followed by clavicle, pelvis and spine in order of decreasing frequency.8,9 But these are not sufficient features to exclude bacterial osteomyelitis.
A number of laboratory investigations have been used to help with the diagnosis of bacterial osteomyelitis, even though they generally lack specificity. The presence of inflammatory markers such as an increased C-reactive protein (CRP) level and increased erythrocyte sedimentation rate (ESR) may be used as an adjunct to the diagnosis and for monitoring clinical response to treatment in bacterial osteomyelitis was not useful in this case series as we observed both a significantly elevated ESR and CRP.12–14 Although, by contrast, in most cases, the presence of persistently normal CRP and ESR levels usually rules out osteomyelitis.13
Additionally, this case demonstrates that MRI is a very sensitive method of investigation to substantiate suspected CRMO diagnosis. Both children examined using MRI had confirmed bone lesions. The typical MRI findings of bone cortical thickening, lytic lesions with sclerosis and bone oedema was seen.15 However, due to some atypical features of sequestra, consistent with possible chronic osteomyelitis, the children had a course of antibiotics. It is not unusual for CRMO to have been treated with course of antibiotics before the diagnosis is made due to the potential complication of delayed treatment. Nonetheless, a delay in diagnosing a non-bacterial osteomyelitis could also have a significant morbidity on children.16 CRMO is commoner in teenagers.6 Children presenting outside this age range should be thoroughly investigated for possible underlying malignancy, such as lymphoma in adult and leukaemia in younger ones.
CRMO diagnosis can be almost definite if typical skin lesions accompany characteristic bone lesions on MRI.17 Notwithstanding, the ‘gold standard’ for the diagnosis of bacterial osteomyelitis or bone malignancy still remained the presence of positive bone cultures and histopathologic examination of the bone.13 However in children with unusual or persistent symptoms, and where the facilities are available a whole body MRI should be considered to detect clinically in apparent lesions of CRMO in other part of the body.
ConclusionsCRMO continues to be a serious health problem worldwide, while representing an economic burden to any healthcare system. Missed and delayed diagnosis has a major impact on the quality of life of patients and is a substantial financial burden. A high index of suspicion and multidisciplinary approach involving radiologists, microbiologists with expertise in infectious diseases, orthopaedic surgeons and rheumatologist will reduce the diagnostic dilemma
Although this diagnosis can often be challenging to the investigating physician, but it is important to realise that an early diagnosis will lead to a more favourable outcome.
Authors’ ContributionsG.O. reviewed the literature, wrote the first draft, and coordinated the production of the manuscript B.J. and T.H. involved in the medical diagnosis, management and follow up of the patient. All authors read and approved the final manuscript.
FundingThere is no institutional, financial or material support for publishing the manuscript.
Conflicts of InterestThe authors declare there are no conflicts of interest.