Our hospital is the nuclear medicine referral hospital for radioisotopic synoviorthesis for all of Castilla-La Mancha.
ObjectiveTo describe the experience in the performance of radioisotopic synoviorthesis for arthritis refractory to other treatments in our hospital.
MethodologyObservational, descriptive and cross-sectional study protocolised through the review of the database of radioisotopic synoviorthesis performed between 2007 and 2017. Previous clinical data were collected (age, sex, pathology, previous treatments, previous infiltration and affected joint), and progress at 6 months after administering the isotope. An Excel database was created for a frequency analysis with SPSS 21.
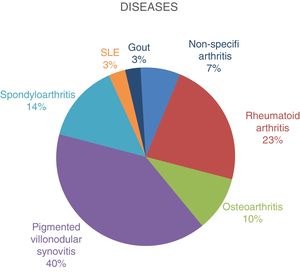
Results30 radiosynovitis interventions were performed. The most frequent pathologies in this order were: pigmented villonodular synovitis (40%), rheumatoid arthritis (23.3%), spondyloarthritis (13.3%), osteoarthritis (10%) and nonspecific arthritis (6.7%), followed by systemic lupus erythematosus and gout. After 6 months, 56.7% of the patients improved compared to 36.7% who remained the same. Likewise, none of them presented complications related to the procedure. Six point six percent of the patients were lost to follow-up.
Discussion and conclusionsIn patients with episodes of recurrent arthritis with associated joint effusion in one or two joints, refractory to systemic treatments, to local infiltrations with corticosteroids and for patients for whom other treatments may be contraindicated, we must consider the possibility of performing an isotope radiosinoviortesis, as it is a simple, safe technique with a success rate of more than 50%.
Nuestro hospital es el hospital de referencia en medicina nuclear para la realización de la sinoviortesis radioisotópica para toda Castilla La-Mancha.
ObjetivoDescribir la experiencia en la realización de la sinoviortesis radioisotópica en las artritis refractarias a otros tratamientos en nuestro hospital.
MetodologíaEstudio observacional, descriptivo y transversal protocolizado a través de la revisión de la base de datos de las sinoviortesis radioisotópicas realizadas entre 2007 y 2017. Se recopilaron datos clínicos previos (edad, sexo, proceso patológico, tratamientos previos, infiltración previa y articulación afectada) y evolutivos a los 6 meses tras administrar el isótopo. Se creó una base de datos Excel para un análisis de frecuencias con SPSS 21.
ResultadosSe realizaron 30 radiosinoviortesis, siendo las enfermedades más frecuentes, por este orden: sinovitis villonodular pigmentada (40%), artritis reumatoide (23,3%), espondiloartritis (13,3%), osteoartritis (10%) y artritis inespecíficas (6,7%), seguido de lupus eritematoso sistémico y gota. Tras 6 meses un 56,7% de los pacientes mejoraron frente a un 36,7% que seguían igual. Así mismo, ninguno de ellos presentó complicaciones relacionadas con el procedimiento. A un 6,6% de los pacientes se les perdió el seguimiento.
Discusión y conclusionesEn los pacientes con episodios de artritis de repetición con derrame articular asociado en una o 2 articulaciones, refractarias a tratamientos sistémicos, a las infiltraciones locales con corticoides y en aquellos pacientes en los que otros tratamientos puedan estar contraindicados, debemos considerar la posibilidad de realizar una radiosinoviortesis isotópica, pues es una técnica sencilla, segura y con una tasa de éxito superior al 50%.
Radioisotopic synoviorthesis (SR), or radiosynoviorthesis, is a non-encapsulated radionuclide therapy consisting of intra-articular injection of particles from a colloidal radioisotopic suspension (citrate, chromate or sulphate). The therapeutic objective is to achieve selective destruction of the synovial membrane, using short-range beta emitting radiotopes that allow the synovial membrane to be irradiated, respecting cartilage and bone. This technique is very useful for the local treatment of chronic joint diseases when they do not respond to conventional systemic or local therapy.1
SR was first described in 1952 by Fellinger and Schmid as a treatment technique for chronic synovitis. In 1968 Delbarre introduced the term radiosynoviorthesis.2 With regard to the choice of isotopes, it is recommended that high energy isotopes are used for large joints, while low energy isotopes should be used for small joints. Thus, Ytrium-90 is used to treat the knee due to its penetration depth (mean of 3.6mm), while Renium-186 is used in intermediate joints (mean penetration of 1.2mm) and Erbium-169 for small joints (mean penetration of .3mm).3,4
The main indications for this technique are arthritides with few radiographic alterations, which have not improved with conservative therapy and with a bone scan negative for synovitis in the late stage (relative indication). These arthritides are: pigmented villonodular synovitis, rheumatoid arthritis, spondyloarthritis, oseoarthritis with persistent synovial inflammation, microcrystalline arthritis and synovitis over a prosthetic joint.
There are 2 types of contraindication to this technique: absolute (unstable joint, intra-articular fracture and sepsis) and relative (pregnancy, moderately positive bone scintigraphy in late stage and Steinbrocker radiographic stages III and IV).5
In addition, two types of complications may occur: short-term complications such as septic arthritis, radiodermatitis, Baker's cyst rupture, lymphoedema, acute synovitis or flu-like syndrome, and long term complications such as chromosomal alterations due to the migration of radioactive particles through the lymphatic system.6
The referral department for all SR in Castilla La-Mancha is the Nuclear Medicine Department of the General University Hospital of Ciudad Real. Therefore the aim of our study is to describe the experience in the performance of SR in arthritis refractory to other treatments in our hospital.
Material and methodsWe included 30 patients from the Castilla La-Mancha health area, with arthritis refractory to the usual treatments. The usual treatments are corticoids, disease-modifying anti-rheumatic and biological drugs in cases of rheumatoid arthritis, spondyloarthritis and microcrystal diseases, and non-steroidal analgesics and anti-inflammatory drugs in cases of pigmented villonodular synovitis, osteoarthritis and non-specific arthritis. All the patients underwent SR from January 2007 to October 2017.
A review of the SR database of the Nuclear Medicine Department of the General University Hospital of Ciudad Real was conducted during the period 2007–2017. A database was created in Excel where the following information on the cases gathered was recorded:
- •
Age and sex.
- •
Disease suffered by the patient.
- •
Type of treatment prescribed.
- •
Previous injection with an intra-articular corticoid.
- •
Affected joint on which the SR is performed.
- •
Immediate complication after isotope administration.
- •
Progress 6 months following isotope administration.
Or the clinical history was reviewed and clinical improvement was defined if there were any of the following changes:
- 1.
Decrease greater than 25% on the visual analogue scale.
- 2.
No further episode of swelling in the affected joint.
- 3.
Greater than 25% improved mobility.
- 4.
Subjective manifestation of global improvement on the part of each patient.
The SR procedure was performed in nuclear medicine settings, where the radioisotopes were prepared and conditioned for intra-articular administration. The joint punctures were undertaken under local asepsis conditions and according to routine techniques. Intra-articular puncture was ensured by obtaining synovial fluid when possible and then the radiopharmaceutical was injected followed by 1ml of triamcinolone acetonide (40mg).
The information obtained was entered into a database and a description of frequencies was made.
ResultsThirty radiosynoviorthesis were performed in the past 10 years in patients with refractory arthritis, all on an outpatient basis and with no onset of immediate complications. Of the 30 patients, 20 were female and ten male, aged between 24 and 84 (mean of 46.37).
All of the patients were cases of recurrent arthritis, refractory to conventional treatments with analgesics and/or non-steroidal anti-inflammatory drugs, corticoids, disease-modifying anti-rheumatic drugs and/or biological drugs, intra-articular corticoid injections and arthroscopic “clean-up” surgery, according to each case.
The diseases for which SR was performed in the study period were, in this order: pigmented villonodular synovitis (40%), rheumatoid arthritis (23.3%), spondyloarthritis (13.3%), osteoarthritis (10%), non-specific arthritides (6.7%), followed by systemic lupus erythematosus and gout (Fig. 1).
Based on previous injection of the joint with triamcinolone acetonide, we observed that 9 of the 30 patients (30% of the patients) had previously undergone corticoid injection, 100% in the knee, and 7 of these 9 patients had a diagnosis of arthritis and/or osteoarthritis, and 2 of the 9 patients were diagnosed with villonodular synovitis (who had previously undergone arthroscopy for surgical synovectomy and biopsy).
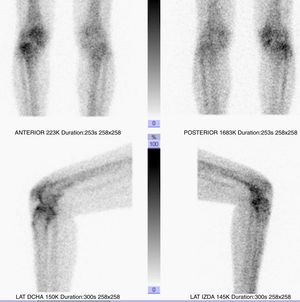
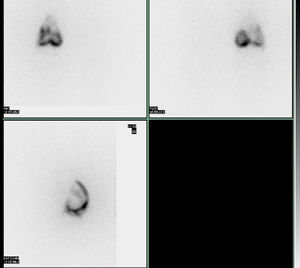
In our case series, the joints treated with radiopharmaceuticals were: 26 (87%) knee with Ytrium-90 (Figs. 2 and 3), 2 (6.7%) ankle with Renium-186 and one (3.3%) shoulder with Erbium-169.
After at least 6 months, 56.7% of the patients had experienced improvement, quantified with a decrease in VAS of more than 25%, reduced swelling, improved mobility of the patient of more than 25% and subjective patient assessment. Thirty-six point seven percent remained the same, whereas we could not determine the progress of the 6.6% of the patients who were lost to follow-up.
Discussion and conclusionsThere are different publications on the efficacy of SR in the treatment of arthritis refractory to systemic and/or local treatments. The majority of these publications7–11 date back 30 years, in which only the baseline situation of the joint was evaluated and the situation post undertaking the SR,11 and do not meet the criteria of evidence-based medicines in terms of methodology, sample size or comparison with other local therapies or placebo, as in the study carried out by Heuft-Dorenbosch with Ytrium.12
SR has many advantages in our environment, such as safety, less aggressiveness compared to surgical synovectomy, simplicity, low cost, repetition of the technique if control was not achieved first time, and it does not require hospitalisation. Furthermore, performing SR does not contraindicate a subsequent surgical synovectomy in cases where more than one SR has been performed.
Table 1 is included to observe the causal relationship between the patients included in the study and the procedure they underwent, which shows positive results (i.e. improvement) 6 months following this procedure, especially in the patients with a baseline disease of pigmented villonodular synovitis and spondyloarthritis, there being 100% improvement in the cases with these disease processes (and up to 2 out of 3 patients with osteoarthritis).
List of patients included in the study.
| Sex | Age | Disease | Previous treatment | Previous injection | Joint affected | Isotope used | Immediate complication | Progress at 6 months | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 49 | Non-specific arthritides | Corticoids+DMARDs | Yes | Knee | Ytrium-90 | No | Same symptoms |
| 2 | Female | 54 | Non-specific arthitrides | Anti-inflammatories | Yes | Knee | Ytrium-90 | No | Same symptoms |
| 3 | Female | 47 | Osteoarthritis | Anti-inflammatories | No | Knee | Ytrium-90 | No | Same symptoms |
| 4 | Male | 47 | Rheumatoid arthritis | Biologicals | No | Knee | Ytrium-90 | No | Same symptoms |
| 5 | Female | 49 | Rheumatoid arthritis | Corticoids+DMARDs | Yes | Knee | Ytrium-90 | No | Same symptoms |
| 6 | Male | 50 | Rheumatoid arthritis | Biologicals | No | Knee | Ytrium-90 | No | Same symptoms |
| 7 | Male | 57 | Rheumatoid arthritis | Anti-inflammatories | No | Knee | Ytrium-90 | No | Same symptoms |
| 8 | Male | 51 | Rheumatoid arthritis | Corticoids+DMARDs | Yes | Knee | Ytrium-90 | No | Same symptoms |
| 9 | Female | 30 | Rheumatoid arthritis | Corticoids+DMARDs | Yes | Knee | Ytrium-90 | No | Same symptoms |
| 10 | Male | 33 | Osteoarthritis | Anti-inflammatories | No | Knee | Ytrium-90 | No | Same symptoms |
| 11 | Male | 48 | Ostoarthritis | Corticoids+DMARDs | Yes | Knee | Ytrium-90 | No | Same symptoms |
| 12 | Female | 84 | Ostoarthritis | Corticoids+DMARDs | Yes | Knee | Ytrium-90 | No | Improvement |
| 13 | Female | 28 | Pigmented villonodular synovitis | Routine analgesics | No | Knee | Ytrium-90 | No | Improvement |
| 14 | Male | 53 | Pigmented villonodular synovitis | Anti-inflammatories | No | Knee | Ytrium-90 | No | Improvement |
| 15 | Female | 33 | Pigmented villonodular synovitis | Corticoids+DMARDs | No | Knee | Ytrium-90 | No | Improvement |
| 16 | Female | 62 | Pigmented villonodular synovitis | Corticoids+DMARDs | No | Knee | Ytrium-90 | No | Improvement |
| 17 | Female | 63 | Pigmented villonodular synovitis | Biologicals | No | Knee | Ytrium-90 | No | Improvement |
| 18 | Female | 54 | Pigmented villonodular synovitis | Corticoids+DMARDs | Yes | Knee | Ytrium-90 | No | Improvement |
| 19 | Male | 26 | Pigmented villonodular synovitis | Routine analgesics | No | Knee | Ytrium-90 | No | Improvement |
| 20 | Male | 27 | Pigmented villonodular synovitis | Routine analgesics | Yes | Knee | Ytrium-90 | No | Improvement |
| 21 | Female | 37 | Pigmented villonodular synovitis | Corticoids | No | Knee | Ytrium-90 | No | Improvement |
| 22 | Female | 46 | Pigmented villonodular synovitis | Routine analgesics | No | Knee | Ytrium-90 | No | Improvement |
| 23 | Female | 24 | Pigmented villonodular synovitis | Routine analgesics | No | Knee | Ytrium-90 | No | Improvement |
| 24 | Female | 51 | Pigmented villonodular synovitis | Anti-inflammatories | No | Knee | Ytrium-90 | No | Improvement |
| 25 | Female | 52 | Spondyloarthritis | Anti-inflammatories | No | Knee | Ytrium-90 | No | Improvement |
| 26 | Female | 46 | Spondyloarthritis | Routine analgesics | No | Knee | Ytrium-90 | No | Improvement |
| 27 | Female | 53 | Spondyloarthritis | Biologicals | No | Interphalangeal | Erbium-169 | No | Improvement |
| 28 | Female | 60 | Spondyloarthritis | Anti-inflammatories | No | Shoulder | Renium-186 | No | Improvement |
| 29 | Female | 60 | Systemic lupus erythematosus | Routine analgesics | No | Ankle | Renium-186 | No | Lost to follow-up |
| 30 | Male | 16 | Gout | Routine analgesics | No | Ankle | Renium-186 | No | Lost to follow-up |
We can conclude that in patients with repeated effusions in one or two joints refractory to conventional systemic or local treatments, such as intra-articular corticoid injections, or in patients for whom certain treatments may be contra-indicated, radioisotope synoviorthesis should be considered, given its success rate of 56.7% in our study.
Conflict of interestsThe authors have no conflict of interests to declare.
I would like to thank the Rheumatology Service, the Nuclear Medicine Departments and the Chronic Pain Treatment Unit for their collaboration and effort, because without them it would not have been possible to treat the patients in an appropriate manner and improve their quality of life, in a less aggressive way than the conventional.
Please cite this article as: Castro Corredor D, Martínez Bravo WR, Ramírez Huaranga MA, Mateos Rodríguez JJ, Rebollo Giménez AI, Anino Fernández J, et al. La sinoviortesis radioisotópica en el control de la sinovitis refractaria en Castilla La-Mancha. Una experiencia de 10 años. Reumatol Clin. 2020;16:485–489.