A 20-year-old male patient was referred for presentation of lytic lesions in an X-ray of the pelvis. He had had a history of chronic disabling lumbago since the age of 14, coinciding with a sport’s injury. He did not present with any family background of osteolysis. Physical examination reported ectomorpheus phenotype, lumbar rectification and painful palpation in the last lumbar vertebrae. There were no neurological changes. Nephropathy markers were negative.
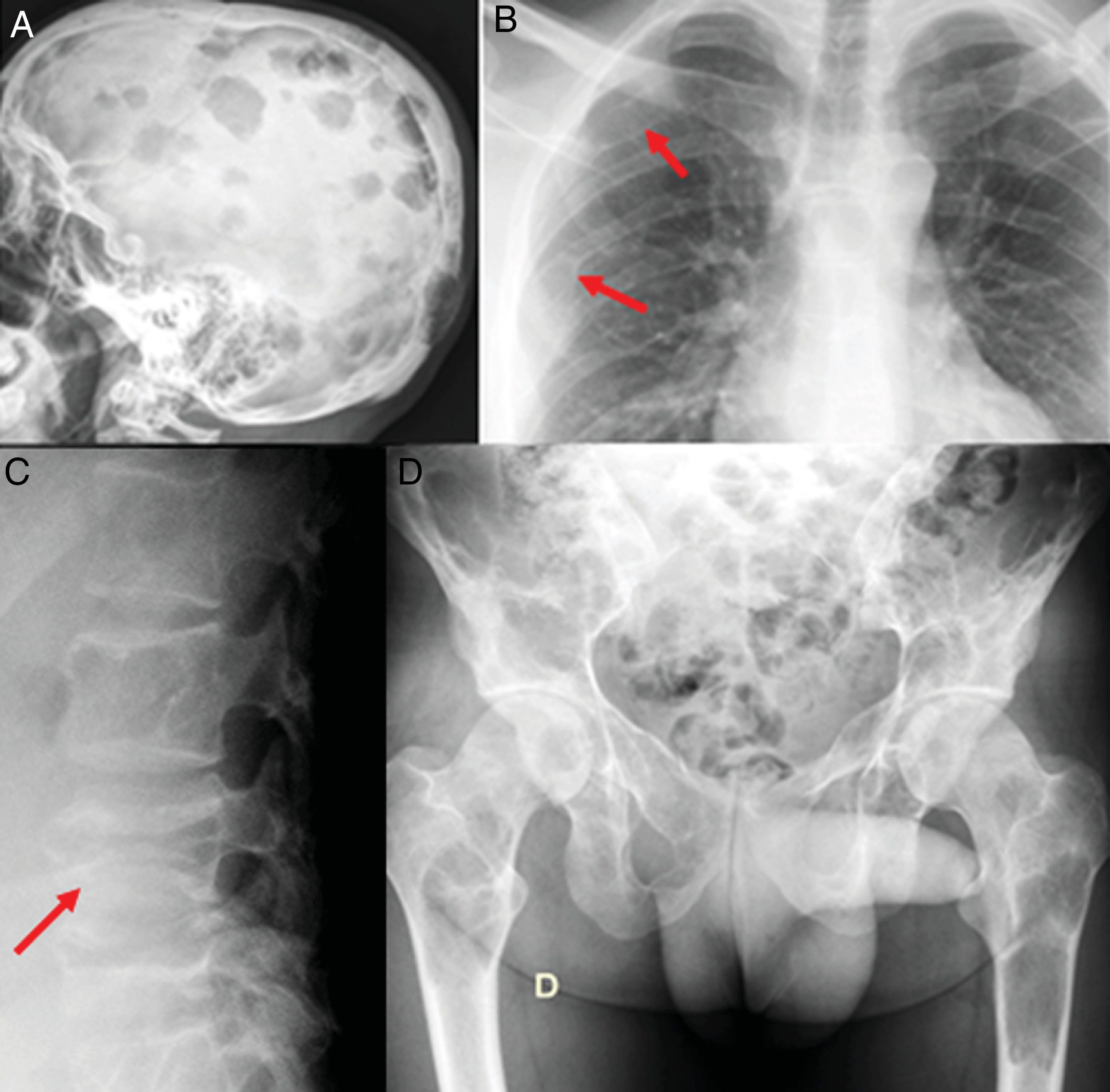
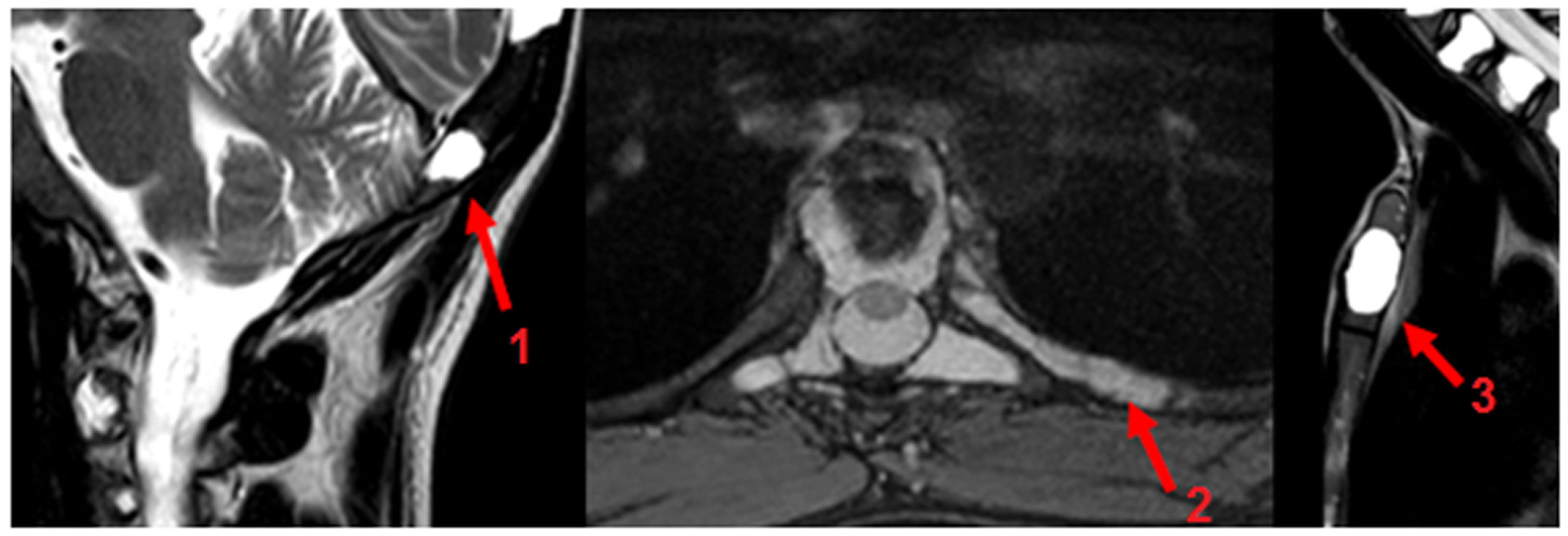
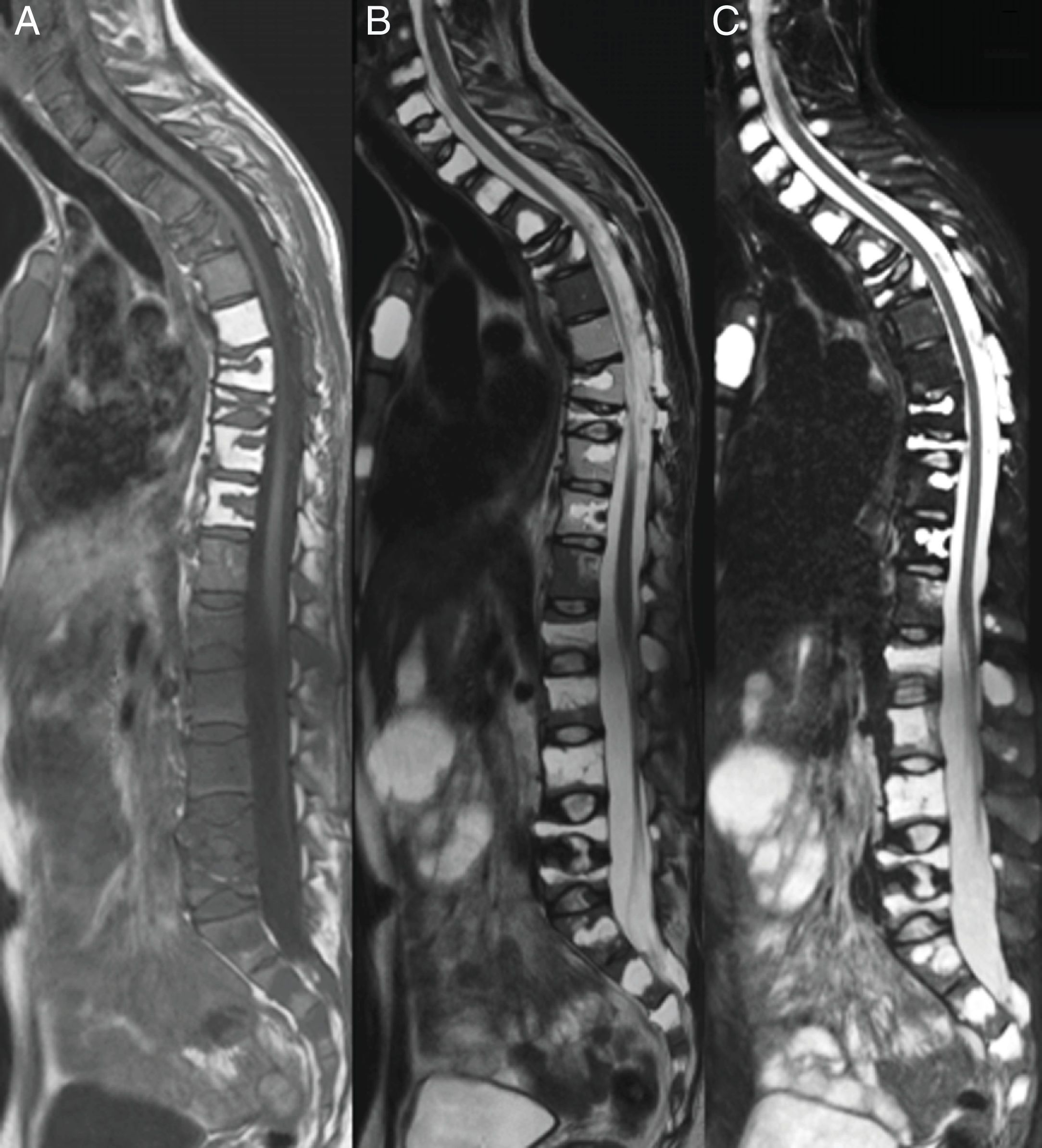
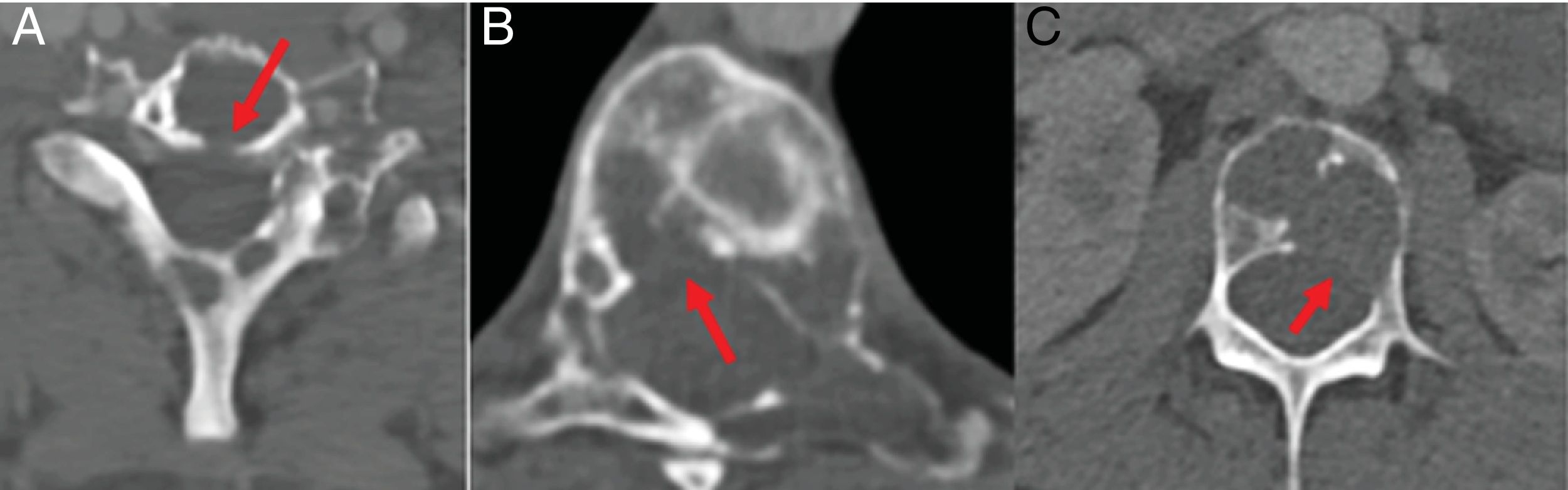
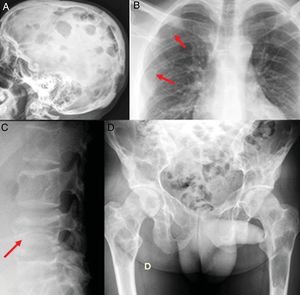
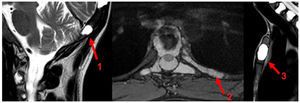
The radiological bone series showed lytic lesions in the skull vault, sacrum, pelvis, femurs, costal arches, and vertebra L4 (Fig. 1). Magnetic resonance confirmed the described osteolysis (Fig. 2, diffuse osteolysis in vertebral bodies and posterior elements of the cervical, dorsal and lumbar spine, multiple vertebral and dorsal flattening and secondary hyperkyphosis (Fig. 3). Computerised tomography demonstrated destruction of the cortical bone in vertebral bodies (Fig. 4).
Radiographic bone series. A) Multiple lytic lesions in skull vault with geographic sides and no sclerosis. B) The arrows show the osteolytic lesions in the right posterior fourth and sixth costal arches s. C) Fracture-flattening of L4. D) Extensive injuries in sacrum, pelvis, and both femurs.
MR images where multiple vertebral flattening can be visualised with secondary hyperphosis, in the sagittal plane of the cervical, dorsal and lumbar spine, enhanced in T1 (A), TT2 (B) and STIR (C). Multiple lesions which are hypointense in T1 and hyperintense inTT2-STIR with diffuse distribution.
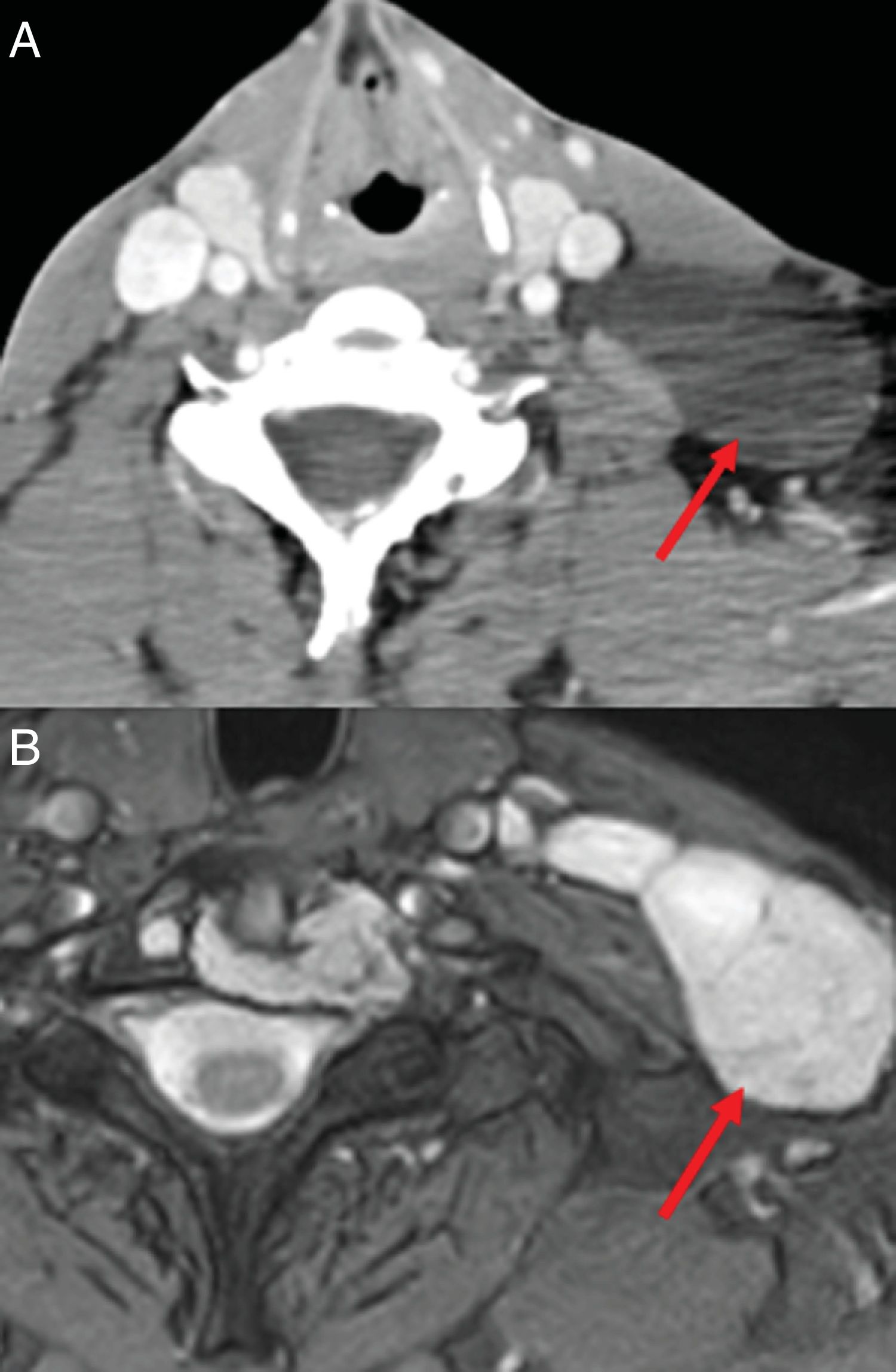
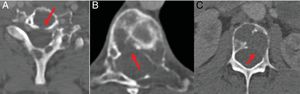
TC with view of cervical, dorsal and lumbar spine bone. Multiple lytic lesions with destruction of cortical bone (arrows). A) In the posterior margin of the vertebral Ct body. B) In the right posterolateral margin of the T8 vertebral body. C) In the left posterolateral margin of the L3 vertebral body.
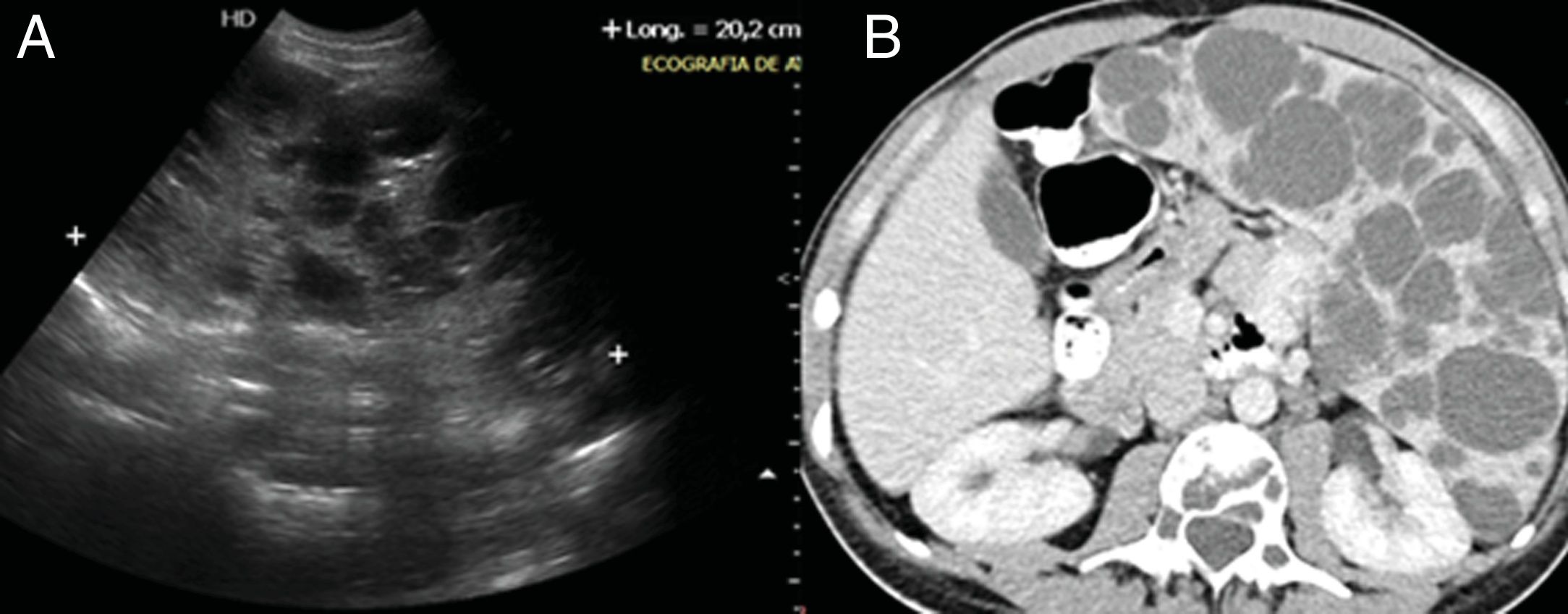
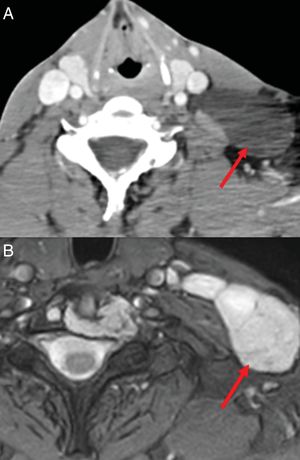
Imaging tests showed a left laterocervical lymphangioma (Fig. 5) and multicystic splenomegalia compatible with diagnosis of diffuse abdominal lymphangioma (Fig. 6). The bone biopsy revealed discreet medullar lymphoid infiltration, with no signs of malignancy.
Based on clinical, radiological and histopathological findings a diagnosis of Gorham-Stout syndrome was made. The patient rejected radiotherapy and began oral treatment with alendronic acid (70mg/week) and sirolimus (2mg/day) until the next control visit.
Discussion/commentGorham-Stout syndrome is a sporadic bone disease, 300 cases of which have been described,1 approximately 50 in the vertebral spine.2 It is characterized by a progressive osteolysis with no bone regeneration, with destruction of the cortical bone, triggered by non neoplasic lymphangiogenesis and hemangiogenesis at medullar level, which may infiltrate soft tissues and lead to fibrosis.3–5 Involvement is usually regional or multifocal,5 mostly in the axial skeleton.3 The evolutional course of the disease is unpredictable, with up to 16% mortality.6 Diagnosis is made by exclusion, ruling out lymphangiomatosis, which does not injure the cortical bone.3,7 Magnetic resonance with gadolium contrast agent is used to monitor patient evolution,8 showing lymphangiogenesis in the active lesions.9 Multifocal location and extensive involvement of the spine makes this case exceptional.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: López García IM, Lorenzo Domínguez MT, Fernández Martínez AM, Cuesta Marcos MT. Osteolisis generalizada en un paciente con síndrome de Gorham-Stout. Reumatol Clin. 2021;17:485–488.