Ultrasound has been included in the training of residents in rheumatology in recent years, as a result of its increased use in daily clinical practice. Our objective is to evaluate the perceived quality of ultrasound training of residents in rheumatology services in Spain.
Material and methodsOnline survey aimed at rheumatologists who began their training in rheumatology between 2009 and 2019.
ResultsOne hundred thirty-nine rheumatologists participated in the survey, of which 97.1% had at least one ultrasound machine in their training centre. Up to 51.1% performed a rotation in ultrasound and 56% had an ultrasound consultation. Access to SER courses was high (87.8%) while access to EULAR courses was limited (17.3%) and up to 69.1% of residents did not complete the competency accreditation. Training in evaluation of inflammatory joint activity, entheses and microcrystalline diseases received the highest scores. Evaluation of ultrasound training during the residency was good in 36% of cases, fair in 28.1%, poor in 18% and excellent in 12.9%. Of those surveyed, 88% consider their clinical practice as a rheumatologist to have improved.
ConclusionsMost residents have performed ultrasound rotations. Participation in SER ultrasound courses is high and moderate in EULAR courses, while only a minority completed the competency accreditation. The overall degree of satisfaction with training in ultrasound during residency is good and, in the opinion of residents, contributes to the improvement of their skills as rheumatologists.
La ecografía se ha incorporado en los últimos años a la formación de los residentes en reumatología, fruto de su creciente expansión en práctica clínica diaria. Nuestro objetivo es evaluar la calidad percibida de la formación en ecografía de los residentes en los servicios de reumatología de España.
Material y métodosEncuesta online dirigida a aquellos reumatólogos que iniciaron su periodo de formación en reumatología entre los años 2009 y 2019.
ResultadosCiento treinta y nueve reumatólogos participaron en la encuesta, y el 97,1% contaban con al menos un ecógrafo en su centro de formación. Hasta un 51,1% realizaron una rotación en ecografía y el 56% contaban con una consulta de ecografía. El acceso a los cursos SER fue alto (87,8%) mientras que fue limitado a los cursos EULAR (17,3%); el 69,1% de los residentes no completó la acreditación de competencias. La valoración más alta en el grado de formación lo recibieron la valoración de actividad articular inflamatoria, entesis y enfermedades microcristalinas. La valoración de la formación en ecografía durante la residencia fue buena en el 36% de los casos, regular en un 28,1%, mala en un 18% y excelente en un 12,9%. Un 88% de los encuestados considera que ha mejorado su práctica clínica como reumatólogo.
ConclusionesLa mayoría de residentes han realizado rotaciones en ecografía. La participación en los cursos de ecografía de la SER es alta, moderada en los cursos EULAR, mientras que solo una minoría completaron la acreditación de competencias. El grado global de satisfacción de formación en ecografía durante la residencia es bueno y, en opinión de los residentes, contribuye a la mejora de las competencias como reumatólogos.
Musculoskeletal ultrasound has become a useful tool in recent years that has been incorporated into clinical practice to aid decision-making in the diagnosis, activity, and treatment of rheumatic diseases1. As a result, training in this major field of rheumatology has entered the routine of rheumatology training specialists, and most European countries have specific national training programmes in this technique. Since 1996, the Spanish Society of Rheumatology (SER), through their School of Ultrasound, have developed a systematic ultrasound training programme that has promoted the implementation of the technique throughout the country as standard training for rheumatologists interested in using musculoskeletal ultrasound in our specialty. This ultrasound training system has been pioneering in Europe2, and in line with European recommendations3 offers 4 levels of continuous training, and provides teaching material prior to the courses, tutorials in the courses and progressive competency assessment overseen by the School’s tutors. Our country has a long tradition in training in ultrasound as applied to rheumatology, and according to data from a survey to determine the degree of ultrasound implementation and training in Europe, Spain was among the 4 countries reporting that more than 50% of rheumatologists had received specific ultrasound training, together with Bulgaria, Finland and Slovakia; only surpassed by Germany, at more than 80%4. In addition, Spain is among the countries offering the highest number of courses per year, the highest percentage of practical training compared to theoretical training, and the fewest students per tutor.
However, despite the efforts of the SER and particularly the SER School of Ultrasound, training in this essential imaging technique for rheumatologists may not be uniform among the different rheumatology departments with teaching accreditation. Putting training into practice depends on factors such as the availability of ultrasound equipment, staff qualified in musculoskeletal ultrasound, access to national and/or international ultrasound courses and residents being given the opportunity to complete rotations in musculoskeletal ultrasound within or outside their department.
The primary objective of the present study is to assess the perceived quality of the musculoskeletal ultrasound training of residents in rheumatology departments in Spain. The secondary objectives include establishing whether there are differences in the quality of training in musculoskeletal ultrasound according to the year in which the training period started.
Material and methodsA cross-sectional study was undertaken that included rheumatologists who started their training period in rheumatology between 2009 and 2019, and who answered an online survey (Table 1) to gather information on their training in ultrasound throughout their period as residents, and how they perceived its level of quality.
Questionnaire on perceived quality of ultrasound training.
| 1. Indicate the Autonomous Community and the year in which you started your training (e.g., Madrid 2010) |
| 2. Does your department have its own ultrasound equipment? |
| a) No |
| b) Yes, at least one machine |
| c) Yes, 2 or more |
| 3. If your department has a dedicated musculoskeletal ultrasound consultation, have you had the opportunity to undertake a rotation in this consultation? |
| a) There is a dedicated ultrasound consultation and I have completed a specific rotation in that consultation |
| b) There is a dedicated ultrasound consultation, but I have not completed a specific rotation there |
| c) There is no dedicated ultrasound consultation, but I have completed a specific ultrasound rotation in a different centre |
| d) There is no dedicated ultrasound consultation, and I have not completed a specific ultrasound rotation |
| 4. If you chose the first or third option in the previous question, please indicate the duration of the rotation (e.g., 2 months) |
| 5. During your training in rheumatology, did you take any of the SER School of Ultrasound courses? |
| a) Yes |
| b) No |
| 6. If you answered yes to the previous question, please indicate the highest level you reached during your training |
| a) Introduction |
| b) Basic |
| c) Intermediate |
| d) Advanced |
| e) Post-advanced |
| 7. During your training in rheumatology, did you take any of the EULAR ultrasound courses? |
| a) Yes |
| b) No |
| 8. If you answered yes to the previous question, please indicate the highest level you reached during your training |
| a) Introductory |
| b) Basic |
| c) Intermediate |
| d) Advanced |
| e) Teach the teachers |
| 9. If you have taken any of the ultrasound courses promoted by SER or EULAR, did you complete competency accreditation, either by the SER School of Ultrasound or by EULAR/EFSUMB? |
| a) I have completed accreditation of all the courses given by SER, but not by EULAR/EFSUMB |
| b) I have completed accreditation of all the courses given by EULAR/EFSUMB, but not by SER |
| c) I have completed accreditation of all courses given by SER and by EULAR/EFSUMB |
| d) I have completed accreditation of some of the courses given by SER and by EULAR/EFSUMB, but not of all the courses that I have taken |
| e) I have not completed accreditation of any of the courses given by SER or by EULAR/EFSUMB |
| f) I have not completed any of the courses during residency, therefore I did not complete the corresponding accreditation |
| 10. During your training in rheumatology, did you complete other ultrasound courses not given by SER or EULAR? |
| a) Yes, one |
| b) Yes, 2 or more |
| c) No |
| 11. If you answered yes to the previous question, specify which |
| 12. Please rank from 1 (maximum training) to 5 (minimum training) the level of training you received in the following musculoskeletal ultrasound applications during your residency |
| a) Assessment of inflammatory joint activity |
| b) Screening for microcrystalline diseases |
| c) Assessment of entheses |
| d) Ultrasound-guided procedures (arthrocentesis, infiltration, blocks, etc.) |
| e) Assessment of soft tissue disease |
| 13. Please rank from 1 (maximum training) to 3 (minimum training) the level of training received in the following ultrasound applications in extra-articular manifestations of rheumatic diseases |
| a) Vascular ultrasound |
| b) Ultrasound of major salivary glands |
| c) Lung ultrasound |
| 14. In general, how would you rate the level of training in musculoskeletal ultrasound during your residency training? |
| a) Excellent |
| b) Good |
| c) Fair |
| e) Poor |
| f) I have not received training in musculoskeletal ultrasound |
| 15. Choose the option that most closely matches your assessment of the ultrasound training your received during residency |
| a) Ultrasound training during residency has greatly improved my competency and clinical practice as a rheumatologist |
| b) Ultrasound training during residency has moderately improved my competency and clinical practice as a rheumatologist |
| c) Ultrasound training during residency has occasionally improved my competency and clinical practice as a rheumatologist |
| d) Ultrasound training during residency has not improved my competency and clinical practice as a rheumatologist |
| 16. Please specify any weaknesses or areas for improvement in musculoskeletal ultrasound training during residency |
The sources of information for data collection included: 1) list of residents completing their training period in the last 10 years provided by the National Commission of Rheumatology, 2) list of residents accessing the ultrasound school courses provided by the SER during their training period in the last 10 years, and 3) responses from an online survey given to the subjects of the study which was disseminated through the ECOSER email group, the SER newsletter, and social networks during November and December 2019. The first two signatories of the study designed all the questions of the survey. The aspects to be evaluated in the survey included: 1) access to SER and EULAR ultrasound courses, 2) completion of the SER or EULAR ultrasound course competency accreditation, 3) access to specific rotations in musculoskeletal ultrasound (within or outside their department/unit)4, access and degree of satisfaction with ultrasound training in its different aspects including non-musculoskeletal examinations, and 5) degree of overall satisfaction with ultrasound training during residency. Table 1 shows all the questions evaluated. The data collected were processed in accordance with Organic Law 15/1999, of 13 December, on the Protection of Personal Data. To evaluate how perceived quality has evolved over the last decade, the total number of respondents was divided into two groups according to the year in which they began their residency period (2009–2013 and 2014–2019) and the variables included in the survey were compared between the two groups.
Statistical analysisA simple descriptive analysis of the results obtained was performed. Absolute values and percentages were determined for categorical variables, medians, and interquartile range (25–75) for ordinal variables, and mean and standard deviation for quantitative variables. The χ2 test was used to compare percentages between the two groups. An error of less than P < .05 was considered statistically significant.
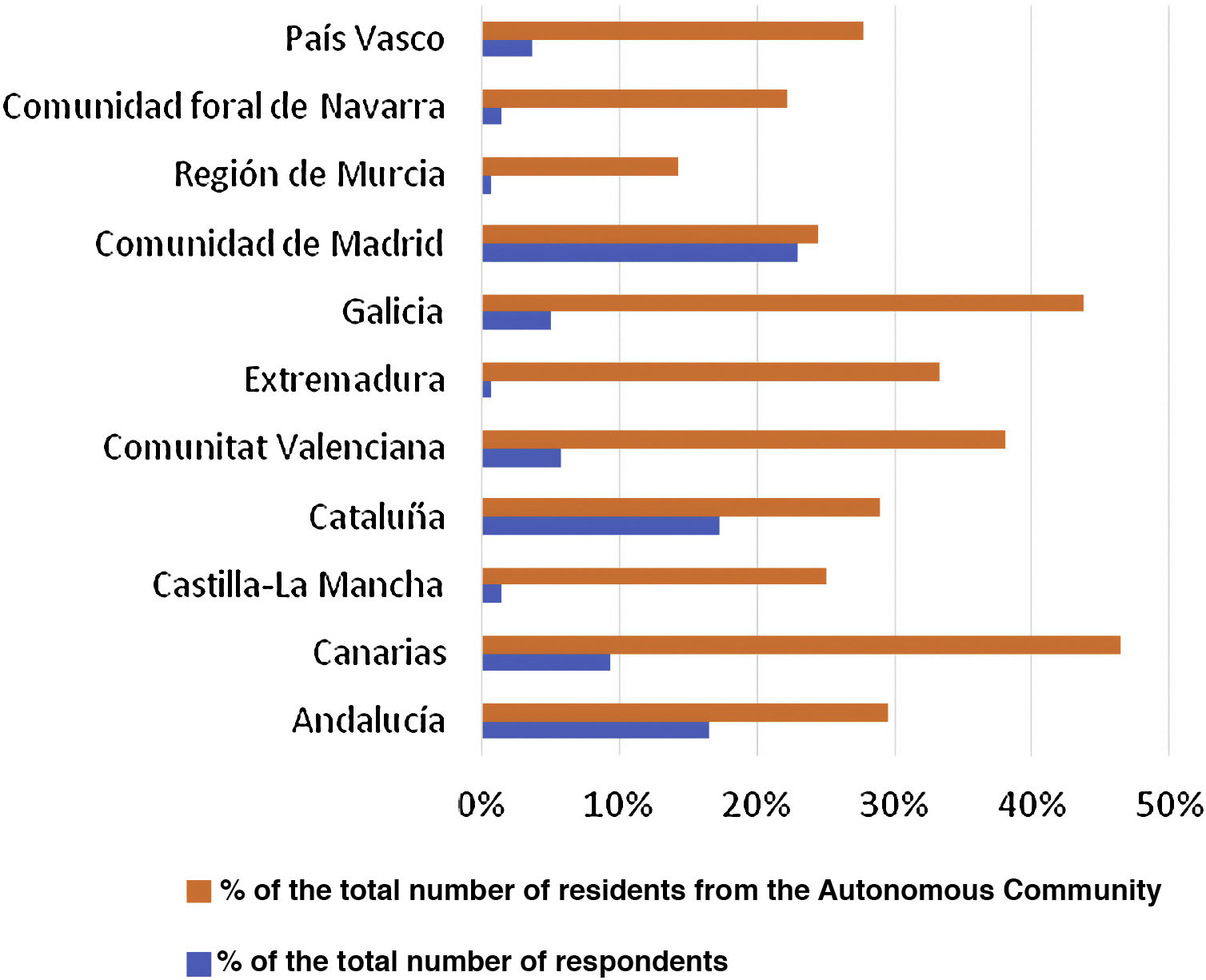
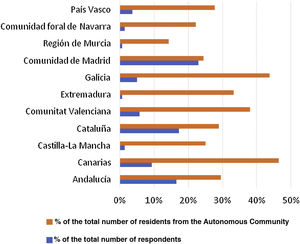
ResultsScope of the surveyA total of 139 responses were obtained over the period the survey was disseminated, corresponding to 31.2% of the target population (445 residents in the last 10 years). The scope of the survey was lower than theoretically expected (46.5% for a 95% confidence level and a 5% margin of error). Fig. 1 shows the distribution of respondents per autonomous community, as well as the ratio of responses to residents in each autonomous community. Four autonomous communities (Principado de Asturias, Castilla and Leon, Cantabria, and Aragon) with centres with teaching accreditation were not represented in the survey.
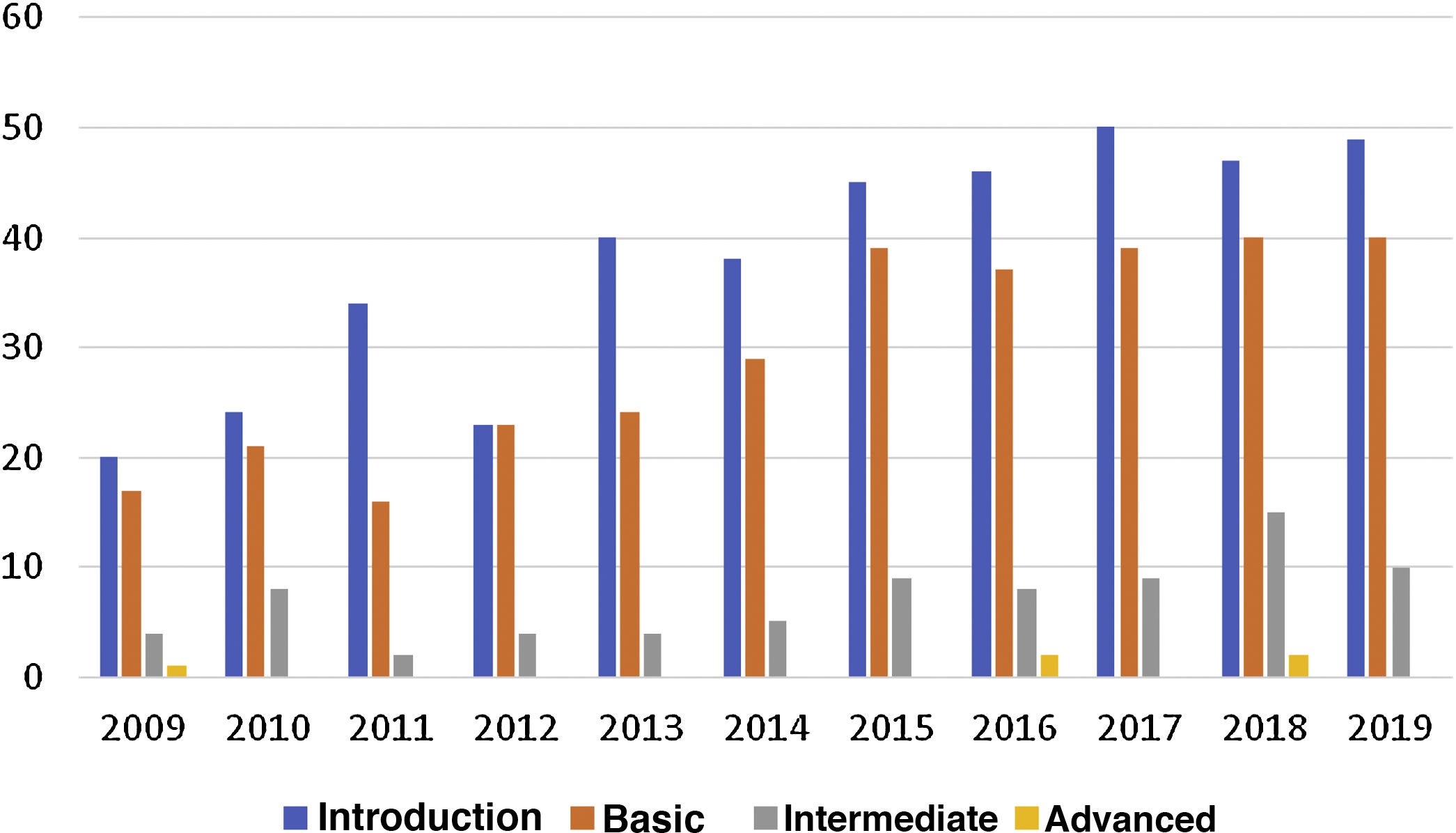
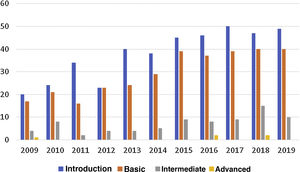
Access to Spanish Society of Rheumatology ultrasound coursesThe number of residents per year has remained stable over the last decade. However, there has been a gradual increase in both supply and demand for ultrasound courses from residents in Spain, especially at the introductory, basic, and intermediate levels (Fig. 2). Access to advanced level courses is very limited for residents, as the training programme offered by the SER generally starts in the second year of residency and because one course is offered each year, they usually finish their training at the School as associate specialists.
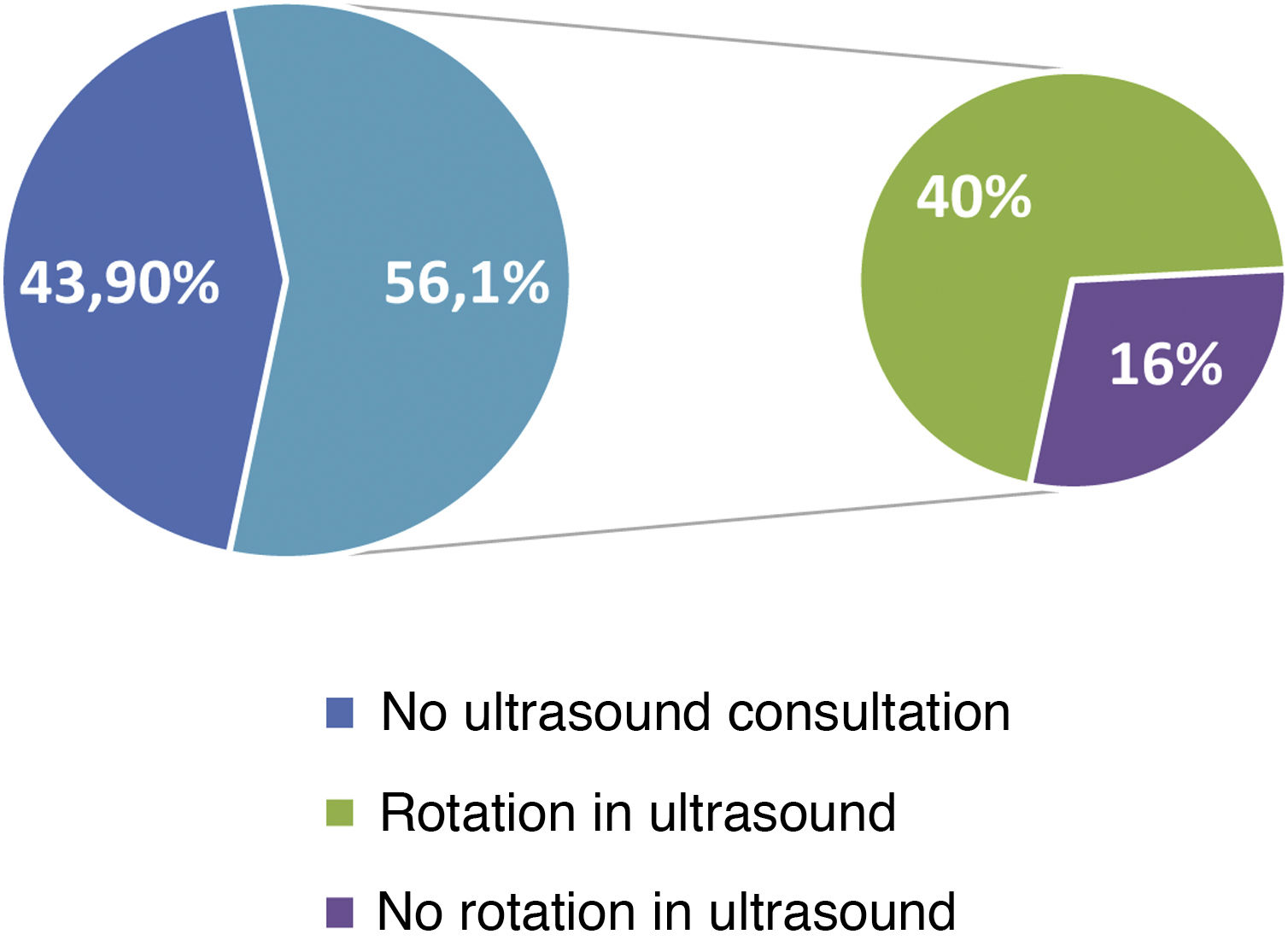
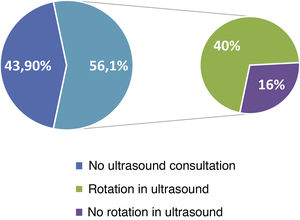
Availability of ultrasound equipment and access to specific ultrasound rotationsOf the respondents, 97.1% have ultrasound equipment in their training centre, and 59% have at least 2 different ultrasound machines available to residents. Regarding access to specific ultrasound rotations, 78 (56.1%) have a dedicated ultrasound consultation, but 22 (16%) do not have access to that ultrasound rotation (Fig. 3). Although the availability of ultrasound equipment is high in centres with teaching accreditation, 61 (43.9%) of the respondents completed their residency in centres without a dedicated ultrasound consultation. In general, 51.1% of the residents were able to undertake a specific rotation in ultrasound within or outside their department, with a mean (SD) duration of 2.9 (1.8) months.
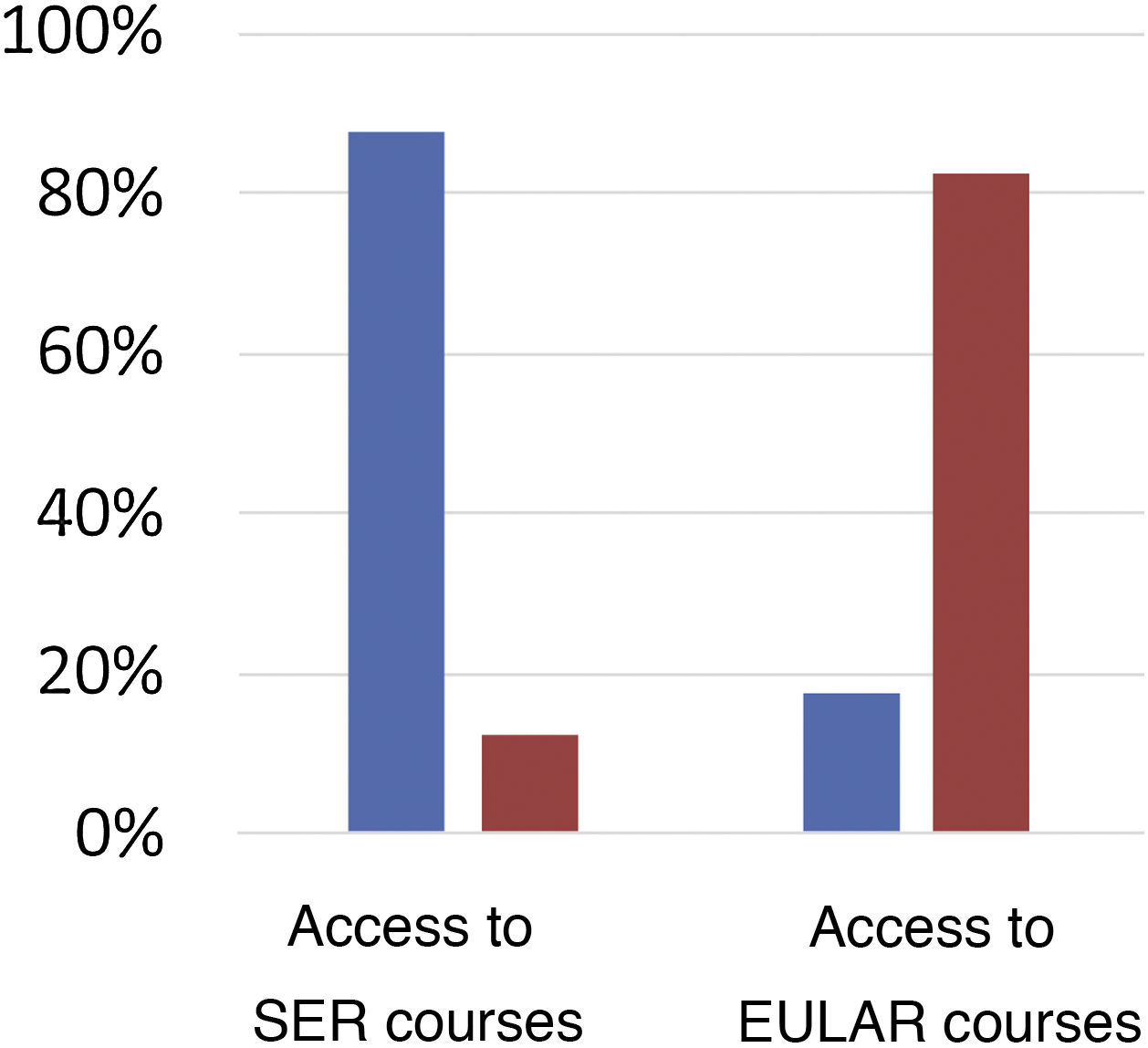
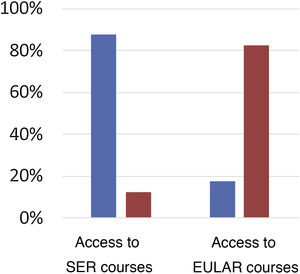
Access to ultrasound training coursesOf the total number of respondents, 122 (87.8%) had taken one of the courses offered by the SER School of Ultrasound during the residency period (Fig. 4). The maximum level reached at the end of the residency was: Introductory (14.39%), Basic (40.29%), Intermediate (16.55%) and Advanced (7.19%). Only 24 (17.3%) of the total accessed any of the EULAR ultrasound courses during the residency period, the “Introductory” level was accessed most frequently (66.67%). Of the residents who attended SER or EULAR courses, 69.1% did not go on to complete competency accreditation, and only 5% completed competency accreditation for all the courses they attended. A total of 48.2% undertook other ultrasound courses not promoted by the SER or EULAR during their residency.
Assessment of competency acquired in ultrasound during the residency periodIn the section that aimed to assess ultrasound training in certain areas, respondents gave their subjective opinion of the training received on an ordinal scale from 1 (maximum training) to 5 (minimum training). They scored assessment of inflammatory joint activity expressed as median [interquartile range] highest (1 [1–3]), followed by assessment of entheses, screening of microcrystalline arthritis ultrasound data, use of ultrasound-guided techniques and assessment of soft tissue pathology (3 [2–4], 3 [2–4], 3 [2–4] and 3 [2–5], respectively). The degree of training received in the use of extra-articular ultrasound was scored from 1 (maximum training) to 3 (minimum training), and vascular ultrasound scored highest (1 [1–2]), followed by salivary gland ultrasound (2 [2–3]) and pulmonary ultrasound (3 [2–3]).
Overall assessment and perceived usefulness of ultrasound training during residencyAssessment of the ultrasound training during residency was good in 36% of the cases, fair in 28.1%, poor in 18%, and excellent in 12.9%. Up to 5% indicated that they had not received any training in ultrasound. Eighty-eight percent of the respondents considered their clinical practice and skills as rheumatologists to have improved.
Evolution of the perceived quality of ultrasound training over the last decadeFinally, we sought to assess whether there were differences between the different variables studied according to the year of starting residency training. Residents who started their residency in the last 5 years (between 2014 and 2019) had greater access to ultrasound rotations compared to those who started residency between 2009 and 2013 (63.3 vs. 40.4%; P < .05). We found no statistically significant differences between groups in terms of access to ultrasound equipment, overall assessment, or perception of the usefulness of the training received during residency (Table 2).
Differences in perceived quality of training between residents who started their residency training between 2009–2013 and 2014–2019.
| Total | 2009−2013 | 2014−2019 | P-Value | |
|---|---|---|---|---|
| n = 106a | n = 57 (53.8%) | n = 49 (46.2%) | ||
| Access to ultrasound in the department itself, n = 105 | ||||
| No | 2 (1.9%) | 1 (1.8%) | 1 (2.1%) | .782 |
| One | 41 (39%) | 24 (42.1%) | 17 (35.4%) | |
| Two or more | 62 (59%) | 32 (56.1%) | 30 (62.5%) | |
| Access to ultrasound rotation, n = 106 | ||||
| Yes | 54 (50.9%) | 23 (40.4%) | 31 (63.3%) | .019 |
| Overall assessment, n = 106 | ||||
| Excellent | 13 (12.3%) | 5 (8.8%) | 8 (16.3%) | .191 |
| Good | 35 (33%) | 19 (33.3%) | 16 (32.7%) | |
| Fair | 33 (33.1%) | 16 (28.1%) | 17 (34.7%) | |
| Poor | 18 (17%) | 14 (24.6%) | 4 (8.2%) | |
| No training | 7 (6.6%) | 3 (5.3%) | 4 (8.2%) | |
| Perceived improvement in competency and clinical practice, n = 98 | ||||
| Great | 33 (33.7%) | 18 (34.6%) | 15 (32.6%) | .537 |
| Moderate | 32 (32.7%) | 14 (26.9%) | 18 (39.1%) | |
| Occasional | 21 (21.4%) | 12 (23.1%) | 9 (19.6%) | |
| None | 12 (12.2%) | 8 (15.4%) | 4 (8.7%) | |
In the last two decades, the use of ultrasound in rheumatology has become widespread in the management of many rheumatic diseases1. Ultrasound facilitates many musculoskeletal examinations but has recently reached a turning point as its use has extended from the musculoskeletal system to extra-articular disease, such as vascular ultrasound in the diagnosis of giant cell arteritis5, ultrasound of salivary glands in Sjögren’s disease6, or lung ultrasound for the diagnosis of diffuse interstitial lung disease7. This has led to this imaging technique being gradually incorporated into specific training programmes in rheumatology. To date, there are no studies that specifically evaluate the perceived quality of training in musculoskeletal ultrasound for residents in rheumatology departments in Spain, and therefore we believe that this study promoted by the SER ultrasound group (ECOSER) may help identify the strengths and weaknesses of this training for our residents.
According to data from a recent survey on access to imaging techniques in rheumatology in Europe8, ultrasound is included in national training programmes in 65% of European countries. Most national societies organise ultrasound training courses, and most include different levels of training. Spain is one of the European countries with the highest access for rheumatologists to the practice of ultrasound (more than 60%). In terms of the different European countries’ national training programmes, Spain offers the highest number of courses per year, followed by Germany. In Spain, the duration of these courses is also the second longest (between 5 and 10 days), only surpassed by France. It is also the country that offers more practical than theoretical training (80% practical and 20% theoretical), and is among the countries with the fewest students per tutor in practical sessions (4 students on average). According to data published in 2011, the demand for training in ultrasound of the locomotor system by SER members has increased progressively since the SER School of Ultrasound was created, but it has been much more marked since 20042. Most notably demand among rheumatology residents has soared since 2011, which reflects the rapid expansion of ultrasound in our specialty. Furthermore, the current training programme for rheumatology residents, drawn up in 2002 and published in the Official State Gazette in October 2009, ranks ultrasound as an important and highly recommended technique for rheumatologists in training9.
The availability of equipment and qualified teaching staff in centres with teaching accreditation is a requirement to ensure adequate ultrasound training. Almost all the respondents (97.1%) have access to ultrasound equipment in their departments and 59% have 2 or more. However, only 61.1% undertake specific ultrasound rotations, and 16% of the total number of residents, even though they have dedicated ultrasound consultations in their departments, have no access to ultrasound. It is essential therefore, to improve access for these rotations, and ultrasound must be considered in drawing up training plans for residents in every centre.
According to the data obtained, residents in our specialty have gained greater access in recent years to ultrasound training through courses at the SER School of Ultrasound (Fig. 2), especially at the introductory and basic levels. These data demonstrate, on the one hand, the efforts by the School to increase their offer and, on the other hand, residents’ growing interest in starting training in this imaging technique. Of the respondents, almost 9 out of 10 took one of the School’s courses during their residency, but only a minority took intermediate and advanced courses. This could be because the SER ultrasound training programme generally starts in the second year of residency and therefore, as one course is offered per year, the advanced course is usually taken after residency has come to an end. Greater effort is needed in the future to ensure that most residents complete all levels of training offered during their residency.
According to recent EULAR recommendations10, competency assessment during rheumatology training is essential to guide learning and ensure quality of care. They also state that competency assessment should be a structured and continuous process that takes place regularly throughout the residency period. According to the results of the present survey, although there is wide access to ultrasound courses promoted by the SER or EULAR, completion of these courses with competency accreditation is low (5% of the respondents). This means that most residents have not completed competency accreditation in performing ultrasound by the time they have started as associate specialists. Promoting competency accreditation for the courses taken should be a joint effort by course promoters, teachers, resident tutors, and the students themselves, as a fundamental way of evaluating, correcting, and progressing in learning.
Ultrasound in rheumatology has expanded in recent decades to cover a wide range of examinations, often beyond the musculoskeletal system. Assessment of inflammatory activity is the most frequent indication for ultrasound examination in rheumatology and receives the highest score in level of training, according to the residents. Although extra-articular examinations are less frequent, vascular ultrasound received the highest score in level of training. The quality of training perceived by the residents is generally positive (almost half the respondents rate it as good to excellent), although almost 20% rate it as poor. Nevertheless, most of the respondents perceive the training they received as useful for their future practice and skills as rheumatologists.
As a secondary objective, we analysed how different aspects have evolved in relation to quality of training over the last decade. Access to ultrasound equipment and the overall assessment of the quality and usefulness of the training received do not seem to differ significantly between the two periods studied (2009−2013 and 2014−2019). There has been greater access to ultrasound rotations in recent years, a sign of residents’ interest in specific training in this field, and ultrasound has been progressively included in each centre’s training plans.
The study has some significant limitations. Firstly, the scope of the survey was smaller than theoretically expected, which may limit the validity of the results obtained. Moreover, participation in the survey from autonomous communities with centres with teaching accreditation was not uniform, and some communities were not represented.
ConclusionsIn summary, ultrasound training during residency training has increased over the last decade. Most residents have completed ultrasound rotations outside or within their training centre. Participation is high in SER ultrasound courses, and moderate in EULAR courses, whereas only a minority of residents completed competency accreditation for the courses taken. Although access to national training courses is high, competency accreditation is an area for future improvement. The residents generally perceive the quality of training as good and that it will improve their practice as rheumatologists in the future.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Molina Collada J, Mayordomo L y Grupo de Trabajo de Ecografía de la Sociedad Española de Reumatología (ECOSER). Calidad percibida de formación en ecografía musculoesquelética en los servicios de reumatología españoles. Reumatol Clin. 2022;18:349–354.