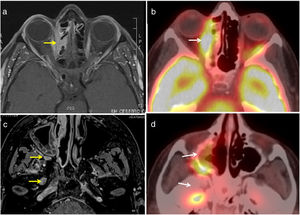
Tolosa-Hunt syndrome (THS) is defined as an idiopathic granulomatous inflammation of the cavernous sinus or superior orbital fissure, characterised by unilateral painful ophthalmoplegia with abnormalities on brain magnetic resonance imaging (MRI) consisting of an increase in size and hyper-uptake of the intravenous contrast medium in the affected cavernous sinus.1,2 It usually presents as a painful paralysis of the third cranial nerve, although it can affect any nerve of the cavernous sinus.1 Diagnosis is clinical and exclusionary. We present a case of THS as an initial presentation of sarcoidosis. This is a 55-year-old woman who consulted with a history of variable, intermittent, horizontal diplopia associated with right upper eyelid ptosis and mild pain. The symptoms had started progressively 4 years earlier and were diagnosed initially as orbital inflammatory disease. The patient also reported erythema nodosum 8 years earlier, and mild fatigue for several months. Physical examination showed paresis of the 6th and 3rd right cranial nerves, with ptosis and horizontal diplopia. In addition, hypaesthesia and allodynia in the territory of the first trigeminal branch (V1). The fundus of the eye was normal bilaterally. Cardiopulmonary, abdominal, skin and locomotor examination were within normal limits. In the complementary tests, blood count, biochemistry, systematic and urine sediment were normal, as well as ESR, PCR and angiotensin converting enzyme (ACE). Lumbar puncture showed normal opening pressure. analysis of cerebrospinal fluid showed no cells, and glucose, total protein and ACE levels were normal. MRI was performed showing swelling and increased extraocular muscles, with intracranial extension and involvement of the cavernous sinus (Fig. 1a and c). CT scan of the chest showed bilateral hilar lymphadenopathy and small, well-defined lung nodes. An 18F fluorodeoxyglucose PET/CT scan (Fig. 1b and d) showed normal uptake in the right orbit and the lymph nodes of the chest. An endoscopic biopsy of the endonasal cavernous sinus was performed, in which confluent, non-necrotising granulomas suggestive of sarcoidosis were found. Tuberculosis screening was negative.
Given these findings we started treatment with glucocorticoids, first 3 boluses of intravenous methylprednisolone from 1g/day and then prednisone at a tapering dose of 1mg/kg. There was rapid clinical improvement, although the orbital extension and established neurological damage showed less response, demonstrated on imaging tests. Given the response to steroids, immunosuppressants were not started.
In our patient, the orbital MRI findings suggested THS. After systemic examination and biopsy, we considered an unusual initial presentation of systemic sarcoidosis with major neurological symptoms. Isolated neurosarcoidosis is rare, since over 90% of patients also have sarcoidosis in other organs, especially the lungs and mediastinal lymph nodes.3 Cranial neuropathy is the most common manifestation of neurosarcoidosis.2 Diagnosing neurosarcoidosis is often difficult, because the clinical manifestations and findings of imaging studies can be mimicked by several other diseases. Brain MRI is the most sensitive diagnostic imaging test.3 This case highlights that sarcoidosis can present in unusual ways, masking neurological disorders.
Please cite this article as: Brandy-García A, Suárez-Cuervo C, Caminal-Montero L. Síndrome de Tolosa-Hunt como una presentación inicial de sarcoidosis. Reumatol Clin. 2021;17:178–179.