Transient osteoporosis is rare and idiopathic.1 It is characterised by arthralgias, radiographic periarticular osteopenia and spontaneous recovery. It was first described in the hip and in women who were in the last three months of their pregnancy.2 Only 10%–40%3 of patients affected develop this process in several joints, either simultaneously or successively, in the same limb or even in the contralateral side, which is then called transient migratory osteoporosis.4 The aim of this study is to present a case where the disease migrated to the contralateral knee and to an ankle.
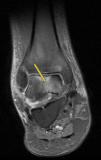
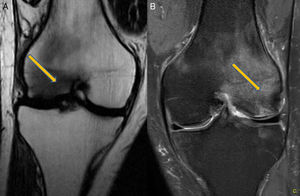
Clinical CaseA 41 year old male with no medical history of interest, presented at the surgery with right knee pain and minimum trauma. Diffuse bone marrow oedema involving the external condyle was reported. Four months later he presented with bone marrow oedema in the ipsilateral internal condyle (Fig. 1). In other magnetic resonance images we found new bone marrow oedema extension, in the internal femoral condyle of the contraleteral knee and later in the external condyle and pain in the right knee, the NMI of which also showed bone marrow oedema (Figs. 2 and 3). Treatment with NSAIDS was administered and partial load-bearing but this was ineffective.
He was diagnosed with transient migratory osteoporosis.
EvolutionModification of treatment to intramuscular calcitonin for 2 months led to an improvement of the gonalgia, with a drop on the VAS from 9 to 2 points, with 74 points on the Lysholm scale and 73 points on the AOFAS scale. After 12 months of follow-up the areas of bone marrow oedema were smaller in size.
DiscussionFor Ramberde,3 this disease appears in the hip (70%, where subchondral fractures may appear in 48.7%, of patients according to Klontzas et al.5), knee, ankle and foot, affecting middle aged adults, males (3:1) and pregnant women. It is self-limiting according to Swoopes et al.6 It has been associated with smokers, metabolic problems and overstraining injuries.7 For diagnosis, the following are useful: radiography (osteopenia),bone scintigraphy (homogenous increase in uptake), NMR5 (oedema, articular effusion, without osteonecrosis), bone density scan (demineralisation) or biopsy (chronic inflammation).
In the differential diagnosis its distinction is interesting, compared with the algodystrophy of Südeck, reflex sympathetic dystrophy or complex regional pain syndrome. This condition is painful after a traumatic event, sometimes with low intensity, and presents with allodynia (or intense pain on response to non painful stimuli), hyperalgesia, and vasomotor disorders with vegetative symptoms. In transient migratory osteoporosis these vegetative symptoms do not arise. Furthermore, the marrow bone oedema presents as an imaging pattern in the NMI characterised by low-intensity signals in T1 and high-intensity signals in STIR T2 in bone marrow. When this oedema appears in several joints without osteonecrosis images, and not in any isolated form, we would diagnose a transient migratory osteoporosis.
However, the algodystrophy of Südeck, reflex sympathetic dystrophy, complex regional pain syndrome, bone marrow oedema syndrome, transient osteoporosis (regional or migratory) and avascular necrosis have similar symptoms, they are idiopathic and present with marrow bone oedema in the NMR. They may therefore form part or be different stages of the same disease, included under the general term of bone marrow oedema syndrome.3
For Emad et al.,8 treatment consists of resting, decompression in the femoral head and drugs such as like calcitonin, pamidronate,9 zoledronate10 or alendronate.11 Treatment with injectable calcintonin must be limited to short term periods (it was only maintained for 2 months in our case), since current recommendations are for Paget's disease, prevention of acute loss of bone mass due to sudden immobility and hypercalcaemia caused by cancer. Intranasal treatment is not recommended due to the increase in the risk of tumours between 7% and 2.4% compared with placebo.7 We believe its use in transient migratory osteoporosis is only reserved for “report” cases like this one and that if in 4 weeks no response has been obtained, treatment with biphosphonates should be considered.10 When response is favourable, treatment should not be extended beyond 2 months.
To conclude, we could confirm that transient migratory osteoporosis is rare, idiopathic and self-limiting. It evolves with migratory pain on weight-bearing, diffuse periarticular osteopenia and bone marrow oedema in the NRM. Treatment is conservative.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that the procedures followed comply with the ethical standards of the Committee responsible for human experimentation, the World Medial Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have adhered to the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in this article. This document remains in the possession of the corresponding author.
Please cite this article as: Jiménez-Martín A, Gómez-Cobo R, Rubio-Gallardo Y, Pérez-Hidalgo S. Osteoporosis transitoria migratoria en miembros inferiores. Reumatol Clin. 2019;15:246–248.