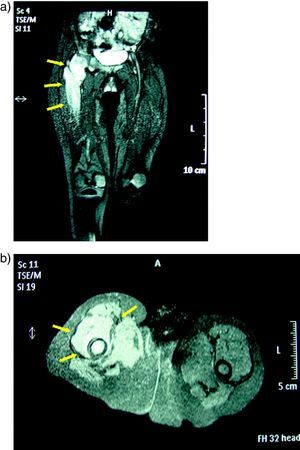
A 2-year-old patient of Romanian origin, with no prior history, presented limping of the lower right extremity lasting for 3 months. The child, a female, presented no fever and upon inspection presented aversion to walking and support with the affected limb. Upon examination there was evident pain and limitation to external rotation and hip abduction. The X-ray showed de-structuration of the femoral head (Fig. 1). Faced with the possibility of osteomyelitis, a magnetic resonance was performed which showed findings compatible with septic arthritis of the coxofemoral joint with proximal femoral osteomyelitis (Fig. 2a) and b)).
Because of the poor progression, the origin of the patient and the radiologic findings, a more ample study was undertaken, performing Mantoux testing which was positive (22mm) and a chest X-ray which posterior upper left lung lobe segment consolidation. Thorax CT was compatible with pulmonary tuberculosis (Fig. 3). A hip arthrotomy with cleansing of the zone and biopsy was performed. Zhiel-Nielsen staining showed acid-fast bacilli, and treatment with quadruple therapy (isoniazid, rifampicin, pyrazinamide and ethambutol) started. After 2 weeks of treatment the patient was able to support weight on the affected limb and after a month started walking again. After 2 months the examination was normal. Culture confirmed the presence of Mycobacterium tuberculosis sensitive to isoniazid and rifampicin and, after 2 months of quadruple therapy, ethambutol and pyrazinamide were discontinued and treatment with the remaining two drugs was continued for 10 more months.
Twelve months after completing treatment, the patient is asymptomatic, movement and examination of the hip resent no alterations, but the X-ray shows alterations in density at the level of the femoral head, with no collapse.
CommentBone and joint tuberculosis constitute 10%–20% of all cases of extrapulmonary tuberculosis and 2% of all cases of tuberculosis.1 The most frequent dissemination pathway is hematogenous and affects mainly the spine and less frequently the hip or the knees in the form of monoarthritis. As in the case of our patient, constitutional symptoms may be absent, delaying diagnosis.2 In endemic areas it is usually manifested in the first year after lung infection.3 The increase in multi-resistant strains has led to treatment with four simultaneous drugs and the identification of the strains’ sensitivity profile to antibiotics.4,5
Please, cite this article as: Iglesias Jiménez E, et al. Artritis tuberculosa en paciente de 2 años de edad. Reumatol Clin. 2011;7(6):417–8.