Takayasu's arteritis (TA), also known as “pulseless disease”, is the third most common vasculitis in childhood. It is a chronic, idiopathic, granulomatous vasculitis that involves large vessels. It occurs most commonly in females with a 4:1 ratio over males; the average age of appearance is 26 years. Its cause is unknown.
Here we report the case of a 7-year-old girl, with type III TA according to the Numano classification, in the ischemic phase, treated with corticosteroids and immunosuppressive agents and early angioplasty due to the severity of the disease. The outcome was satisfactory.
The diagnosis of TA in children under 10 years of age is made only in 2% of them. The delay in diagnosis reaches a mean of 19 months. The course of the disease is variable despite surgical and immunosuppressive treatment.
La arteritis de Takayasu (AT) o «enfermedad sin pulsos» es la tercera vasculitis más frecuente en la infancia. Es crónica, idiopática, granulomatosa y afecta a vasos grandes. Afecta a las mujeres, con una relación 4:1; con una edad promedio de 26 años. Su causa es desconocida.
Presentamos el caso de una niña de 7 años y 7 meses de edad, con AT tipo III de la clasificación de Numano, en fase isquémica, a la que se le inició tratamiento con glucocorticoides e inmunosupresores, así como angioplastia temprana, por la severidad del cuadro clínico. Tuvo una evolución satisfactoria.
El diagnóstico de AT antes de los 10 años se realiza en el 2% de los pacientes; el retraso en el diagnóstico es en promedio de 19 meses; el curso de la enfermedad es variable a pesar del tratamiento inmunosupresor y quirúrgico.
Takayasu's arteritis (TA) is the third most common vasculitis in childhood after Henoch Schönlein and Kawasaki's1 disease. Its cause is unknown but it is known to be mediated by T cells and antibodies which are not organ-specific, although antiaorta and antiendothelium antiannexin V antibodies have been occasionally reported.1
There is a possible intervention of tuberculosis as a cause, with granulomas and Langhan's giant cells found, whose morphology resembles tuberculous lesions in patients with TA. There is a high incidence of positive intradermal tuberculin.2
The average age of presentation is 11.4 years, 20% of cases were diagnosed before age 19 and 2% before age 10. There is a delay in diagnosis of 19 months.2
In childhood, the clinical picture is nonspecific, with possible fever, malaise, anorexia, myalgia, joint pain, abdominal pain, hypertension, hypertensive retinopathy, heart failure, headache and seizures. The presence of murmurs and absence of pulses are present in the ischemic stage of the disease.2
The course of the TA is variable, despite the use of corticosteroids, which reduce by 50% the progression of the lesions; immunosuppressive therapy (methotrexate/azathioprine/mycophenolate mofetil) leads to a better control of the disease and prevents restenosis.3
Stenosis is not reversible and early angioplasty is required in patients with renovascular hypertension, severe claudication, stroke, myocardial infarction, renal artery stenosis, moderate regurgitation of the aortic valve and the presence of more than 3 stenotic4 sites. Early diagnosis and appropriate treatment prevents complications related to the disease.
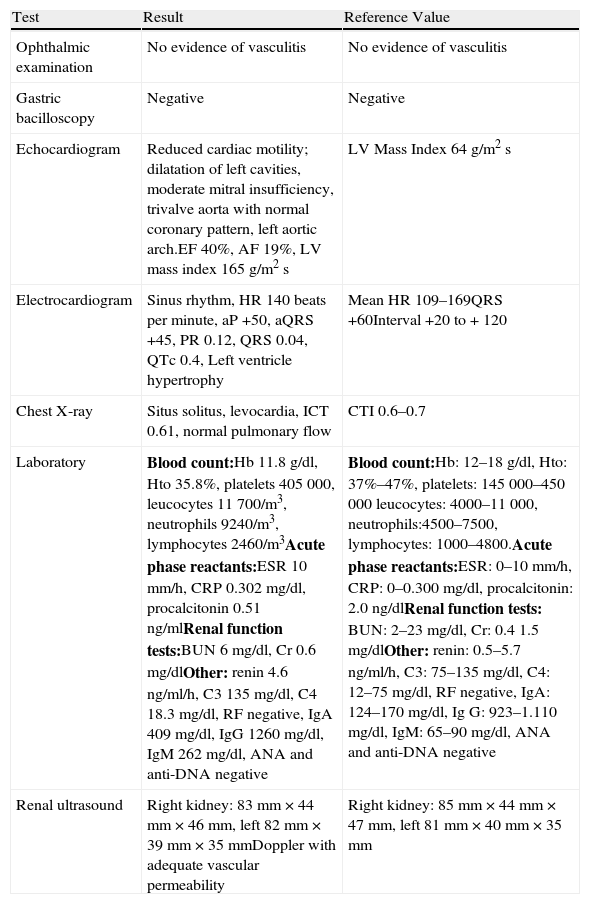
Case ReportThe case is a female patient, 7 years and 7 months old, previously healthy, from the State of Mexico. She began her current illness a month earlier, with malaise, myalgia, vomiting, claudication, headache, tinnitus, fosfenus, tinnitus, abdominal and chest pain. She was admitted to a second level hospital for hypertension and heart failure and was sent to a third level hospital due to absence of pulses and left ventricular hypertrophy. She was admitted due to hypertension, absence of pulses (left brachial and lower limbs), an aortic pansystolic grade II/VI murmur, hepatomegaly and claudication. Her study protocol can be seen in Table 1.
Diagnostic Approach to the Patient.
| Test | Result | Reference Value |
| Ophthalmic examination | No evidence of vasculitis | No evidence of vasculitis |
| Gastric bacilloscopy | Negative | Negative |
| Echocardiogram | Reduced cardiac motility; dilatation of left cavities, moderate mitral insufficiency, trivalve aorta with normal coronary pattern, left aortic arch.EF 40%, AF 19%, LV mass index 165g/m2s | LV Mass Index 64g/m2s |
| Electrocardiogram | Sinus rhythm, HR 140 beats per minute, aP +50, aQRS +45, PR 0.12, QRS 0.04, QTc 0.4, Left ventricle hypertrophy | Mean HR 109–169QRS +60Interval +20 to + 120 |
| Chest X-ray | Situs solitus, levocardia, ICT 0.61, normal pulmonary flow | CTI 0.6–0.7 |
| Laboratory | Blood count:Hb 11.8g/dl, Hto 35.8%, platelets 405000, leucocytes 11700/m3, neutrophils 9240/m3, lymphocytes 2460/m3Acute phase reactants:ESR 10mm/h, CRP 0.302mg/dl, procalcitonin 0.51ng/mlRenal function tests:BUN 6mg/dl, Cr 0.6mg/dlOther: renin 4.6ng/ml/h, C3 135mg/dl, C4 18.3mg/dl, RF negative, IgA 409mg/dl, IgG 1260mg/dl, IgM 262mg/dl, ANA and anti-DNA negative | Blood count:Hb: 12–18g/dl, Hto: 37%–47%, platelets: 145000–450000 leucocytes: 4000–11000, neutrophils:4500–7500, lymphocytes: 1000–4800.Acute phase reactants:ESR: 0–10mm/h, CRP: 0–0.300mg/dl, procalcitonin: 2.0ng/dlRenal function tests: BUN: 2–23mg/dl, Cr: 0.41.5mg/dlOther: renin: 0.5–5.7ng/ml/h, C3: 75–135mg/dl, C4: 12–75mg/dl, RF negative, IgA: 124–170mg/dl, Ig G: 923–1.110mg/dl, IgM: 65–90mg/dl, ANA and anti-DNA negative |
| Renal ultrasound | Right kidney: 83mm×44mm×46mm, left 82mm×39mm×35mmDoppler with adequate vascular permeability | Right kidney: 85mm×44mm×47mm, left 81mm×40mm×35mm |
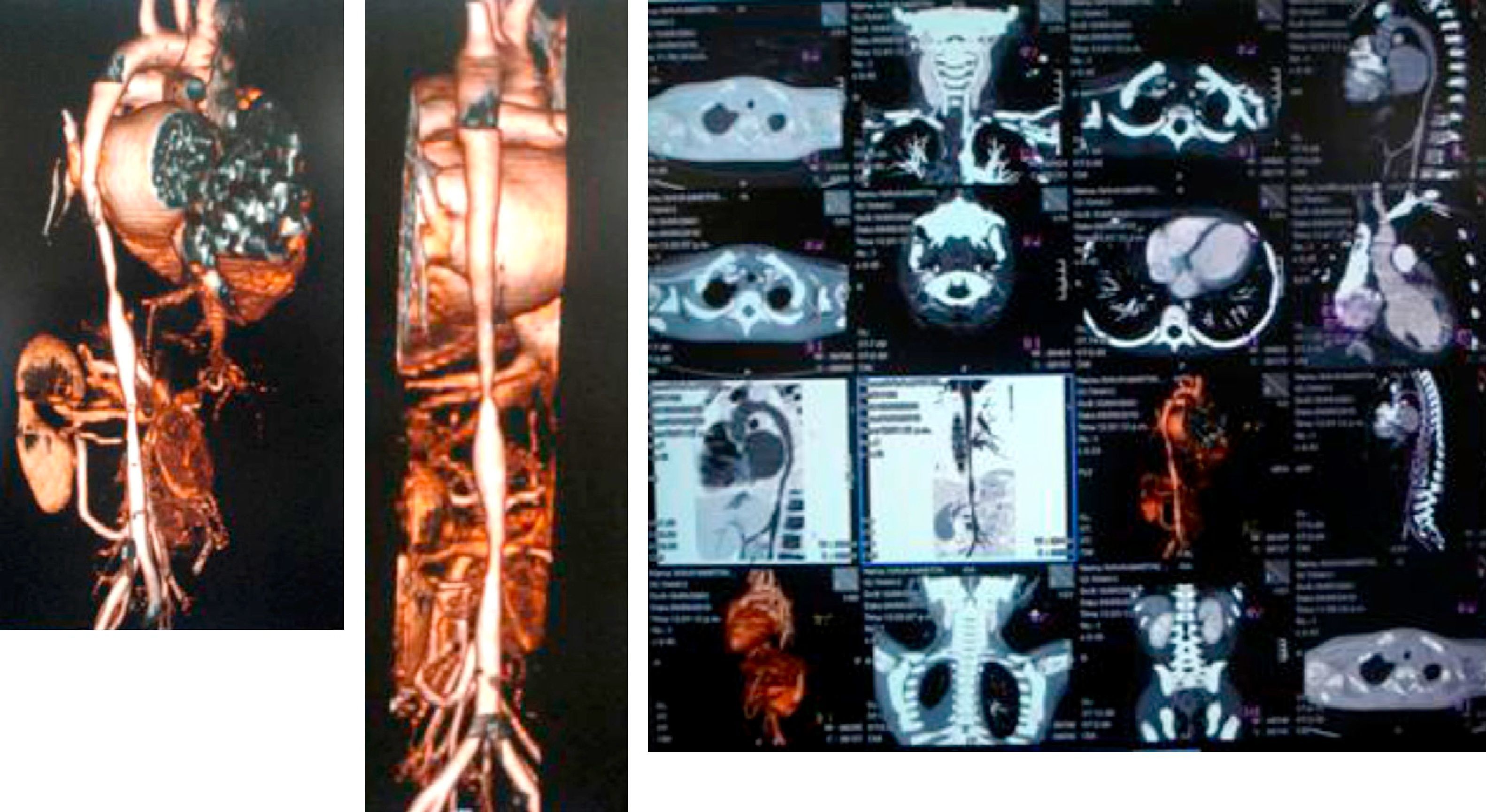
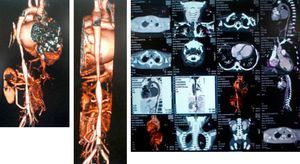
A computed tomography scan revealed hypoplasia of the right vertebral artery (V4), left subclavian stenosis and narrowing of the descending aorta with arteritis data on the wall, yuxtadiafragmática and transverse diameters of 4.5–5.0mm. Were also stenosis in the origin of the superior mesenteric artery (3.3mm) and significant stenosis in the origin of the right renal artery (Fig. 1).
The diagnosis of TA III was based on the following: decreased peripheral arterial pulses and limb claudication, pressure difference greater than 10mmHg, murmur over the aorta, arterial hypertension and angiographic abnormalities (thoracic ascending and abdominal aorta and renal arteries).
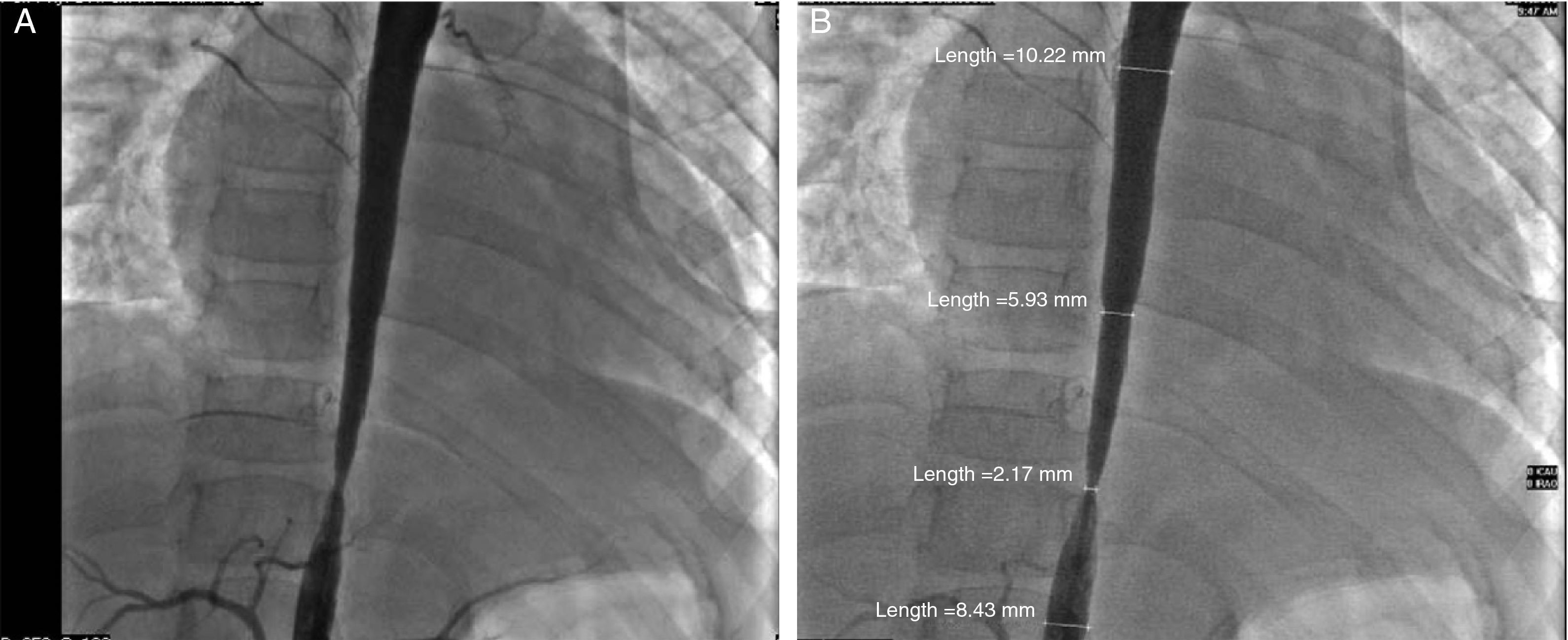
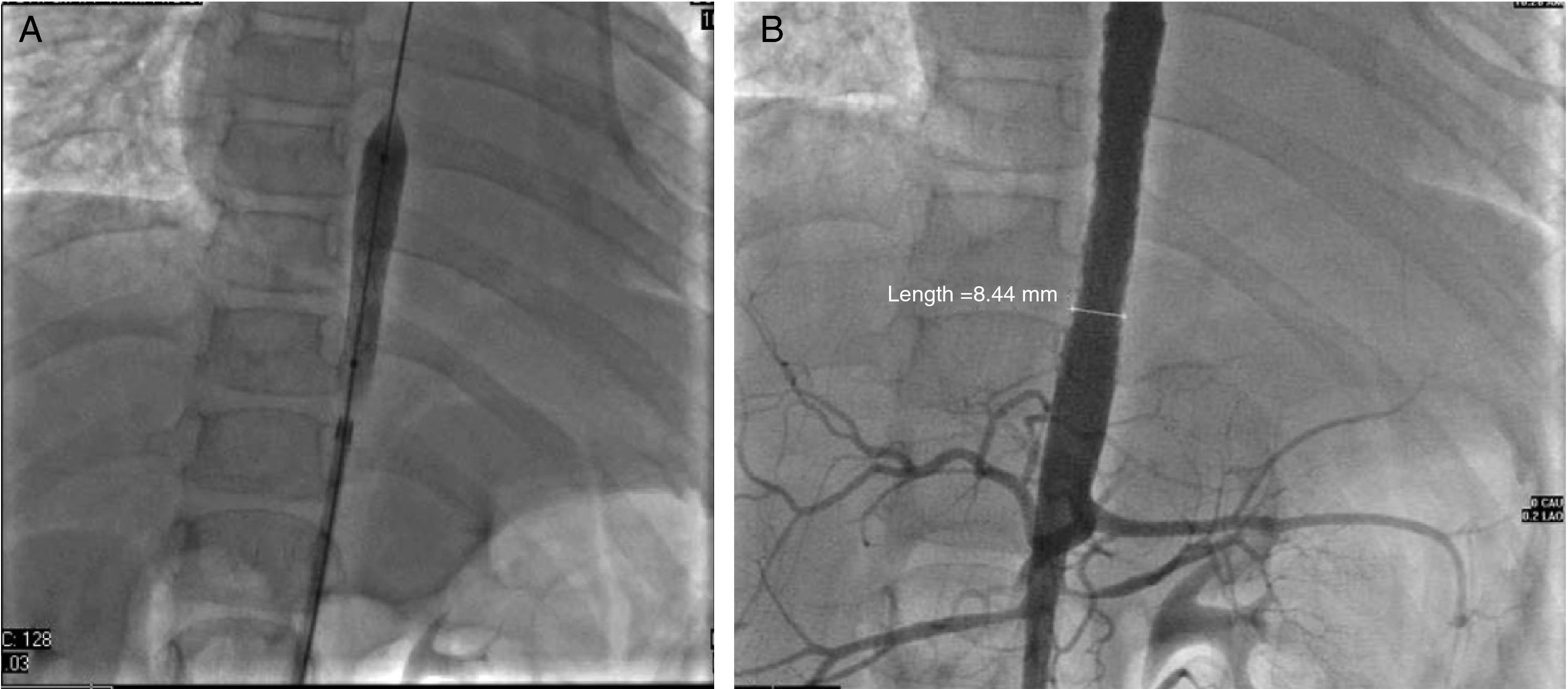
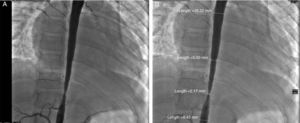
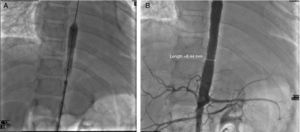
Glucocorticoids and methotrexate were initiated. Cardiac catheterization was performed due to the presence of more than 3 sites of stenosis. We documented diastolic dysfunction, mild mitral regurgitation; severe stenosis of the thoracoabdominal aorta with a gradient of 50mmHg and nonsevere renal artery stenosis (10mmHg gradient) (Fig. 2A and B). Angioplasty was performed in which two stents were placed in the stenotic area, with a postsurgical gradient of 0 (Fig. 3A and B). She is currently asymptomatic with no residual gradient. She no longer receives glucocorticoids but is receiving methotrexate, folic acid, vitamins A, C and D, aspirin, furosemide, spironolactone, and captopril.
TA represents 1.5% of vasculitidies in childhood, with 2% of cases diagnosed before age 10. Their course is variable, depending on the degree of activity, time of diagnosis, presentation and associated symptoms and the effect on other organs. They may have multiple relapses despite treatment.5 The inflammatory process causes thrombosis in the affected arteries, progressive appearance of stenosis, dilation and aneurysms. Antiplatelet therapy with low dose aspirin reduces the frequency of ischemic events.6,7
Treatment is based on the use of glucocorticoids and immunosuppressive therapy. The use of ACE inhibitors is controversial due to their renal effects, but can be considered for use in patients with normal renal function. Surgical correction with angioplasty techniques is effective, increasing 5 years survival to 80%–95%.8 Restenosis occurs in 31.7% during the first year. The risk decreases by 50% with the use of corticosteroids and immunosuppressants. Follow-up angiography should be performed every 12 months.9
The experience in our country has been described by Lupi-Herrera in a series of 107 patients with TA, whose ages ranged from 11 to 30 years, with a mean age 26 years.6,7 The major clinical manifestations were asthenia, weight loss, headache, claudication, and hypertension. Stenosis occurred in the thoracic aorta (25% upper/lower 67%), subclavian (85%) and renal (62%) arteries. A higher morbidity was associated with the Mexican phenotype, severity of disease expression and variations depending on the medical and surgical treatment employed.10
Worldwide experience is very similar, but with few cases reported in the pediatric literature. The studies conclude that it is a condition that must be actively suspected in order to initiate early treatment to decrease mortality. In our country, there are few publications and experience regarding treatment. In this case report, a good clinical history with an appropriate semiology made it possible to steer towards an accurate diagnosis, providing an opportunity for the patient to receive adequate medical and surgical treatment.
Conflict of InterestThe authors declare no conflict of interest.
The authors of this article would like to thank Dr. Jose Agustin Ramirez Barreto for his help in translating this article.
Please cite this article as: Mendiola Ramírez K, et al. Arteritis de Takayasu tipo III en un paciente pediátrico. Reporte de caso y revisión de la literatura. Reumatol Clin. 2012;8:216–9.