Rheumatoid nodules are a rare manifestation of lung disease associated with rheumatoid arthritis (RA). Their emergence and evolution in the course of the disease is variable. The diagnosis of pulmonary rheumatoid nodules may be suggested if they have a typical appearance in an appropriate clinical context, but an accurate diagnosis cannot be made based only on imaging tests. It is recommended to follow nodules and may be necessary to histologically differentiate them from tumors.
Los nódulos reumatoides son una manifestación rara de las enfermedades pulmonares relacionadas con la artritis reumatoide. Su aparición y evolución en el curso de la artropatía es variable. El diagnóstico de nódulo reumatoide pulmonar se puede sugerir si tienen una apariencia típica y en un contexto clínico adecuado, pero no se puede hacer un diagnóstico de certeza basándonos solo en las pruebas de imagen. Se recomienda el control de los nódulos y puede ser necesario el estudio histológico para diferenciarlos de lesiones tumorales.
Thoracic manifestations of RA include pleural disease, interstitial pneumonia, pulmonary vasculitis, airway disease and pulmonary rheumatoid nodules.1
Rheumatoid nodules are the most specific, although they are rare pulmonary manifestation.
This article reviews 5 cases of patients with pulmonary nodules in the context of RA with special attention to their symptomatology and radiological progression.
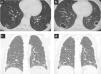
Clinical ObservationCase 1 (Fig. 1)This patient was a 72-year-old male, diagnosed with RA 5 years prior, a non-smoker, and rheumatoid factor (RF) positive. In the preoperative chest radiograph we detected lung nodules. Asymptomatic computed tomography of the chest shows multiple nodules, predominantly subpleural, some larger (3cm) and cavitated with irregular borders. During follow-up, a transthoracic biopsy, was performed and rheumatoid nodules werediagnosticated.1
Case 1. Typical and atypical nodules. (a) Preoperative chest radiograph with multiple pulmonary nodules. (b) CT scan of the chest: larger nodules in upper lobes, irregular surface and contour, neoplasia was ruled out by percutaneous biopsy and the diagnosis of rheumatoid nodules was reached. (c) CT scan of the chest: well demarcated, subpleural rounded nodules in lower lobes (parietal pleura, mediastinum, fissures (asterisk)), some isolated and cavitated (arrow). The radiographic appearance is typically of rheumatoid nodules.
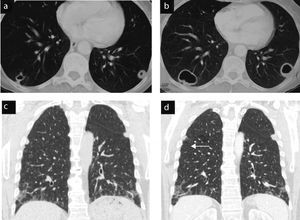
This patient was a 56-year-old woman, diagnosed with RA 5 years prior, smoker, and positive RF. A chest X-ray taken due to chest pain detected lung nodules. Computed tomography of the thorax found rounded nodules of 1–2cm cavitated, progressing in size and complicated by a pneumothorax. She underwent node resection surgery and an open pleural biopsy with a diagnosis of rheumatoid nodules. In subsequent tests all nodules disappeared.
Cases 2 and 3. Evolution of cavitated nodules. (a) and (b) Case 2: cavitated rheumatoid nodules that increase in size. The case was complicated and open pneumothorax produced a cavitated nodule on the pleura (pneumothorax image not shown). (c) and (d) Case 3: rounded subpleural nodules, in a patient with signs of interstitial lung disease. Control computed tomography of nodules show a slight decrease in size and cavitation (arrow).
This was a 53-year-old patient, diagnosed with palindromic rheumatism 6 years prior, and a smoker. RF has slowly turned positive. Interstitial lung disease associated with no respiratory symptoms. In a control CT, we detected, rounded subpleural lung nodules. Monitoring was proposed and computed tomography at 6 months shows that the nodules decreased in size and one of them had cavitated.
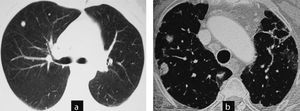
Case 4 (Fig. 3)This patient was a 66-year-old male, diagnosed with RA for 9 years, RF positive and an ex-smoker. A year ago he was diagnosed with interstitial lung disease with respiratory symptoms, moderate dyspnea and mild restrictive respiratory failure. A control CT detected, one year later, rounded subpleural pulmonary nodules. The patient required follow-up.
Cases 4 and 5. Different clinical settings: surgical biopsy or control image. (a) Case 5: chest CT: non-specific nodules in a patient without a diagnosis of joint disease and respiratory symptoms. The patient was diagnosed with necrotizing granulomas requiring surgical biopsy. The patient developed rheumatoid arthritis a year later. (b) Case 4: CT scan of the chest: nodules with typical radiological aspect of rheumatoid nodules, rounded, subpleural and multiple in a patient with rheumatoid arthritis associated with interstitial lung disease. Control image.
This patient was a 47-year-old woman with no known joint disease. A chest radiograph due to coughing and expectoration found multiple pulmonary nodules. Computed tomography revealed that the nodules were millimetric, rounded, predominantly peripheral, subpleural, located in the upper lobes. A surgical biopsy of the nodules was made with the diagnosis of necrotizing granulomas. A year after symptoms, she presented joint swelling and was diagnosed with RA. In subsequent tests the nodules were stable without associated respiratory symptoms.
DiscussionPulmonary rheumatoid nodules are a rare manifestation of RA. Their prevalence ranges from less than 0.4% in radiological studies to 32% in lung biopsies of patients with RA and suspicion of disease.2
It has been reported that they occur more frequently in male patients with positive RF, smokers and those with subcutaneous3 nodules.
Their appearance is related to the development of RA and is variable. They may appear and evolve or regress without any relation to the evolution of arthritis. They have also been reported in rare cases that precede the joint disease.4–6
They are mostly asymptomatic and do not require, in most cases, a specific treatment.
The development of nodules is also another unpredictable prognostic factor and may evolve in number and size as in case 1, regress spontaneously as in case 2, or remain unchanged as in case 5.
In the radiological semiology they are defined as rounded, multiple nodules, and more rarely as solitary nodules. They are preferentially located in the middle and superior peripheral lobe or pleural-based, with a size ranging from millimeters to 7cm. Up to 50% may cavitate, and be accompanied by an associated pleural effusion, pneumothorax or hydropneumothorax.3 Chest computed tomography is a complementary technique to simple X-rays and the most useful to identify and define the characteristics of the nodules, such as cavitation, morphology, and density as well as the most accurate technique to see the progression in size.
Of the reported cases, in 3 patients a histological diagnosis of the nodules was made. In 2, it was a presumptive diagnosis, but patients are clinically stable and nodules are unchanged or decreased in size in control imaging studies.
There are also descriptions of other cases of non-neoplastic lung nodules in the context of RA. Granulomas are rare and may occur in cases of nodular7 and cholesterol8 amyloidosis.
ConclusionIn a clinical setting of RA with the existence of pulmonary nodules, a radiological diagnosis is made in those with multiple, rounded, well-defined rheumatoid nodules of similar size and subpleural location. Unusually there is a need to consider the possibility of histological diagnosis to rule out tumors.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
DisclosuresThe authors have nothing to disclose.
Please cite this article as: Gómez Herrero H, et al. Nódulos pulmonares reumatoides: forma de presentación, métodos diagnósticos y evolución, a propósito de 5 casos. Reumatol Clin. 2012;8:212–5.