Hypertrophic osteoarthropathy is an entity characterized by a triad of periostitis of long bones, clubbing and arthritis. Radiologically there are two patterns, one characterized by new bone formation which predominates in patients with pulmonary disease, and another by acro-osteolysis that is most frequently associated with congenital heart disease. We report the case of a 30-year-old man diagnosed with primary pulmonary hypertension for two years, developing hypertrophic osteoarthropathy with a mixed radiological pattern.
La osteoartropatía hipertrófica es una entidad caracterizada por la tríada de periostitis de huesos largos, acropaquias y artritis. Radiológicamente se distinguen 2 patrones; uno caracterizado por neoformación ósea que predomina en pacientes con patología pulmonar, y otro por acro-osteolisis que se asocia más frecuentemente con cardiopatías congénitas. Presentamos el caso de un varón de 30 años diagnosticado de hipertensión arterial pulmonar primaria desde los 2 años, que desarrolló una osteoartropatía hipertrófica con un patrón radiológico mixto.
Hypertrophic osteopathy (HOA) is a disease characterized by chronic proliferative periostitis of long bones, acropachy and arthritis.1,2 It can be divided according to its etiology in primary HOA, with no apparent underlying cause, familial aggregation and chronic progression; and secondary, associated with lung, cardiac, hepatic or intestinal diseases, with a tendency to bilateralism, symmetric and rapidly progressive. There are two distinct radiological patterns of HOA, one characterized by hypertrophia or bone neoformation, predominant in patients with lung disease (pneumic HOA) and which has its onset after puberty; and another with acroosteolysis, associated frequently with cyanotic congenital heart disease and which has its onset during childhood. Two variants have been seen in this last pattern, one in which the reabsorption of the distal phalanges makes them adopt a pyramidal form and another in which its massive destruction leads to the formation of flat surfaces.1,3 We present the case of a patient with primary pulmonary hypertension who developed HOA with a mixed radiological pattern.
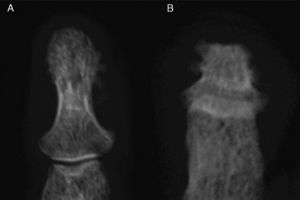
Clinical PresentationThe case is a 30-year-old male patient with a history of primary pulmonary hypertension without a shunt and followed by pediatric cardiology ever since. He had no other history of importance, including rheumatic disease or psoriasis. At age 29 he started presenting episodes of symmetric, additive polyarthritis which affected knees, ankles, shoulders, wrists and metacarpophalangeal joints, with important functional limitation. Physical examination found, in addition to generalized cyanosis and acropachy, no skin or nail lesions suggestive of psoriasis. Laboratory analysis found normal acute phase reactants, negative rheumatoid factor and positive low titer anti-CCP antibodies in a single determination. X-rays showed acroosteolysis of the distal phalanges of the hands and feet, severest in the latter, in which some of the phalanges adopted the form of a pyramid or had a flattened end, with important bone neoformation in both locations, especially the hands (Figs. 1 and 2). Both wrists observed, in addition to radiocarpal and intercarpal joint impingement, especially of the left side, no erosions. Long bones (tibia, peroneal, radial) had a cottony cortex and periosteal separation compatible with periostitis. A bone scyntigraphy showed moderate uptake in the distal phalanges of both hands, as well as right wrist and radium with a theoretical zone in the left semilunar.
Hand X-ray (A) in which there is a periosteal reaction on the radius. There is distal widening with hypertrophic changes and areas of osteolysis, with a good example on the right fourth finger. Juxtaarticular demineralization. Feet X-ray (B) observing marked destruction of the distal phalanges, some with flattened morphology and distal hypertrophy with bone proliferation. There is marked deformity of the fingers.
The patient was diagnosed with pneumic HOA and treated with low dose steroid (deflazacort 6mg/day), zoledronate (single 5mg dose) and calcium and vitamin D supplements. He responded rapidly to treatment with remission of arthritis and steroids were suspended after a few months; he only presented a single relapse which responded after 2 weeks of treatment with no further relapses.
DiscussionThis case involved a patient with underlying lung pathology of pediatric onset, who developed a late polyarthritis that led to the diagnosis of pneumic HOA. However, changes such as acro-osteolysis, new bone formation and periostitis probably had a longer evolution, but because these events often have a more insidious course and patients are often asymptomatic, it is usually detected in an incidental radiological study.
Previous studies have reported that foot affection is more frequent and more severe than that of the hand,1,4 as in our patient. Solid and continuous periosteal reaction in the long bones is also a common finding,3 such as the one our patient presented on the tibial and radial bones.
The mixed pattern combining acroosteolysis and bone neoformation in the same patient was what called our attention, however, some studies suggest that these patterns are not mutually exclusive and constitute a continuum in which initial stages have a predominance of proliferative changes with osteolysis in late stages.1 Another characteristic is that generally, areas of hypertrophy/osteolysis correspond with greater uptake in scyntigraphy,5 as seen in this case.
The patient had positive low titer anti-CCP antibodies in a single determination with no other criteria for rheumatoid arthritis nor with any compatible radiological lesions, nor did he require treatment with methotrexate or any other disease modifying drug. We have not found, in the reviewed literature, any relationship between HOA and anti-CCP positivity, thus considering a false positive case. The patient did not have any skin lesions or axial or enthesitic affection suggesting psoriatic arthritis; however, because it was a rapid onset case of polyarthritis with osteolytic and proliferative changes, psoriatic arthritis must be considered in the differential diagnosis.
The mechanism that leads to bone lesions in HOA is unknown. From the histological standpoint it is characterized by an excessive deposition of collagen, endothelial hyperplasia, edema and osteoblast proliferation in the distal parts of long bones, leading to subperiostic bone neoformation.6 Among the factors that intervene in these changes are endothelial vascular growth factor (VEGF),7 reflex vagal hyperstimulation,8 interleukin 11,9 paraneoplasic growth factors,10 hormonal alterations,11 circulating immune complexes,12 antiphopholipid antibodies,13 alterations in platelet function14 and endothelial activation.2
Treatment of secondary HOA corresponds to that of the underlying condition (for example, correction of the heart defect, treatment of cancer or infection, etc.). Symptomatic management of HOA includes non steroidal antiinlammatory drugs and steroids for joint pain,6 and bisphosphonates such as pamidronate15 and zoledronate16 which control pain due to periostitis, with antiosteoclastic activity that inhibits the expression of VEGF.17 Another drug employed is octeotride which has also shown activity on VEGF.18
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sifuentes Giraldo WA, et al. Osteoartropatía hipertrófica con acro-osteolisis y neoformación ósea en un paciente con hipertensión pulmonar primaria. Reumatol Clin. 2012;8:208–11.