Vaccination against pathogens such as influenza or pneumococcus is widely recommended for patients with rheumatoid arthritis; the prevalence of adherence to these vaccination programmes in Mexico is not known.
MethodsA cross-sectional descriptive study was carried out, through the application of a survey to adult patients with a diagnosis of rheumatoid arthritis treated in a tertiary hospital in Mexico City.
Results227 patients were included, vaccination against influenza was found in 31.3% and against pneumococcus in 17.6% of patients, the main reasons for non-compliance with the vaccination schedule were related to ignorance and the recommendation by doctors not to do so.
ConclusionsCompliance with the recommended vaccination schedules in the studied population is lower than those reported in other populations. The most important interventions to improve coverage should be aimed at educating both patients and medical personnel.
La vacunación contra agentes infecciosos como influenza y neumococo está ampliamente recomendada para pacientes con artritis reumatoide, no se conoce la prevalencia de adherencia a estos programas de vacunación en México.
MétodosSe realizó un estudio descriptivo trasversal, por medio de aplicación de encuesta a pacientes adultos con diagnóstico de artritis reumatoide atendidos en un hospital de tercer nivel en la Ciudad de México.
ResultadosSe incluyeron 227 pacientes, se encontró una prevalencia de vacunación contra influenza en 31,3% y contra neumococo en 17,6% de los pacientes, los principales motivos para el no cumplimiento del esquema de vacunación estuvieron en relación con el desconocimiento y a la recomendación por parte de los médicos de no hacerlo.
ConclusionesEl cumplimiento de los esquemas de vacunación recomendados en la población estudiada es mas bajo que los reportados en otras poblaciones. Las intervenciones mas importantes para mejorar la cobertura deben ir encaminadas a la educación tanto de pacientes, como de personal medico.
Patients suffering from autoimmune inflammatory diseases (AIDs), such as rheumatoid arthritis (RA), systemic lupus erythematosus, spondyloarthropathies, among others, have an increased risk of developing infections, derived from both the immunosuppressed state of the disease and the treatment used1. These are one of the main causes of morbidity and mortality in these subjects2.
Vaccination in patients with AIDs is widely recommended by different clinical practice guidelines against influenza, herpes zoster, Streptococcus pneumoniae (S. pneumoniae), Haemophilus influenzae, hepatitis A, hepatitis B, human papilloma virus, tetanus, and Neisseria meningitis3,4. However in developed countries such as the United States the vaccination rate against influenza in patients with RA is 45,8%5 while for S. penumoniae it is only 28,5%6. Worldwide the highest vaccination rates are found in France at a rate of 56.5%, whilst in Latin America there are reports in Uruguay of 46.4%, and in Argentina of 36.7%7.
There is little information in Mexico on the adherence of patients with RA and other AIDs to recommended vaccination schedules. One study evaluated adherence by rheumatologists in recommending vaccination to their patients, finding among the 122 professionals consulted that only 50% recommend immunisation against influenza and 36.07% against pneumococcus8. A study in France that evaluated vaccination coverage against influenza and pneumococcus in patients with inflammatory joint diseases on biologic therapy and the factors associated with non-adherence found that rheumatologists recommend vaccination against influenza in 79% of patients and against pneumococcus in 79% of patients, found that rheumatologists recommend vaccination against influenza by 79% and against pneumococcus by 78%, much higher percentages than those recommended by primary care physicians9, but these results present a challenge since the percentage of patients who adhere to the recommendations is even lower. The prevalence of RA patients in Mexico and much of Latin America who comply with the vaccination schedule recommended by clinical practice guidelines is unknown3,4.
Materials and methodsType of studyA descriptive cross-sectional study was conducted, including patients diagnosed with RA over 18 years of age, who attended the outpatient clinic at the rheumatology department of the Centro Médico Nacional 20 de Noviembre, in Mexico City between June and October 2020. The protocol was approved by the institutional ethics committee with registration number 446.2020.
The sample size was calculated using the formula for estimating a population proportion; Taking as the population 800 patients diagnosed with RA treated at the institution, in the case of influenza the reported vaccination frequency is 45.8%5, with a confidence interval of 95% and a precision of 5%, resulting in a total sample of 259 patients. In the case of pneumococcus, the reported vaccination frequency is 28.5%6, with a confidence interval of 95% and a precision of 5%, resulting in a total sample of 226 patients, with the value of 226 being taken as the minimum. The allocation of patients was carried out probabilistically by convenience, according to their attendance at the hospital, with the application of a survey conducted by the researchers in order to avoid incomplete completion of the forms, all patients were consulted about their voluntary participation and signed informed consent, and all the protective and social distancing measures recommended to avoid the spread of COVID-19 were applied.
Processing and statistical analysisThe data obtained through the data collection instrument were entered into the database elaborated in the SPSS software version 24, which was used for statistical analysis. To satisfy the general objective of the research, the prevalence of vaccination in the surveyed patients was calculated as the dependent variable; continuous data were described as mean ± standard deviation (SD) and categorical data as n (%). Chi-square test was applied to compare percentages. Bivariate analysis was performed to identify factors associated with influenza and pneumococcal vaccination.
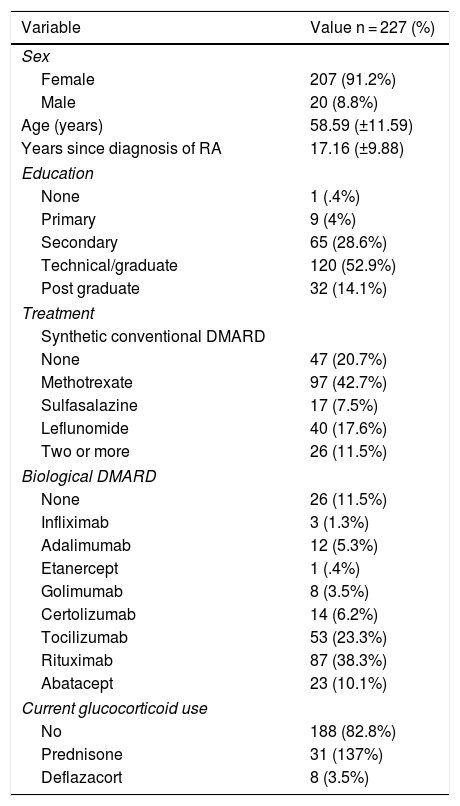
ResultsIn the end, 227 patients were included in the study. Table 1 summarises the characteristics of the population, including demographic data and treatment history.
Characteristics of the population surveyed.
| Variable | Value n = 227 (%) |
|---|---|
| Sex | |
| Female | 207 (91.2%) |
| Male | 20 (8.8%) |
| Age (years) | 58.59 (±11.59) |
| Years since diagnosis of RA | 17.16 (±9.88) |
| Education | |
| None | 1 (.4%) |
| Primary | 9 (4%) |
| Secondary | 65 (28.6%) |
| Technical/graduate | 120 (52.9%) |
| Post graduate | 32 (14.1%) |
| Treatment | |
| Synthetic conventional DMARD | |
| None | 47 (20.7%) |
| Methotrexate | 97 (42.7%) |
| Sulfasalazine | 17 (7.5%) |
| Leflunomide | 40 (17.6%) |
| Two or more | 26 (11.5%) |
| Biological DMARD | |
| None | 26 (11.5%) |
| Infliximab | 3 (1.3%) |
| Adalimumab | 12 (5.3%) |
| Etanercept | 1 (.4%) |
| Golimumab | 8 (3.5%) |
| Certolizumab | 14 (6.2%) |
| Tocilizumab | 53 (23.3%) |
| Rituximab | 87 (38.3%) |
| Abatacept | 23 (10.1%) |
| Current glucocorticoid use | |
| No | 188 (82.8%) |
| Prednisone | 31 (137%) |
| Deflazacort | 8 (3.5%) |
DMARD: Disease-modifying Anti-rheumatic Drug; RA: Rheumatoid Arthritis.
In the specific questions on influenza vaccination, we initially asked how many patients had current immunisation, i.e., had been vaccinated within the last year, with 71 patients (31.3%) responding affirmatively; we also analysed the distribution of this variable with respect to other independent variables, such as sex, schooling and type of treatment used, with no significant differences between groups. Finally, we studied long-term compliance with continuous influenza vaccination over the last 5 years, with 27 patients (11.9%) reporting having received the influenza vaccine.
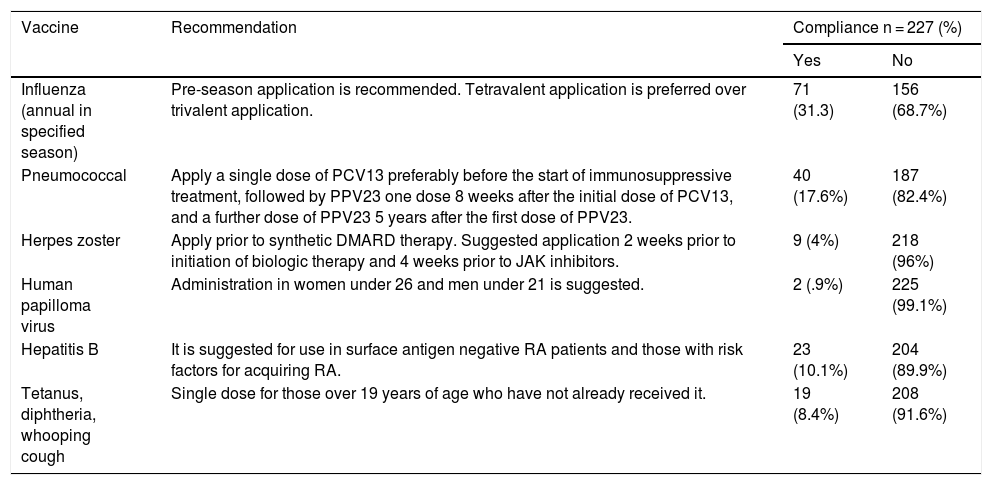
Regarding vaccination against S. pneumoniae, only 40 patients (17.6%) received immunisation against this microorganism in the last 5 years; this variable was also analysed by sex, schooling and type of treatment, with no significant differences between groups. The combined protection against pneumococcus (in the last 5 years) and influenza (in the last year) in the same individual was also investigated, with 29 patients (12.8%) fulfilling this condition. The study also asked about the application of other vaccines recommended by the Mexican College of Rheumatology for patients diagnosed with rheumatoid arthritis artritis8, and these data are summarised in Table 210.
Compliance with the vaccination schedule recommended by the Mexican College of Rheumatology for patients with a diagnosis of rheumatoid arthritis.
| Vaccine | Recommendation | Compliance n = 227 (%) | |
|---|---|---|---|
| Yes | No | ||
| Influenza (annual in specified season) | Pre-season application is recommended. Tetravalent application is preferred over trivalent application. | 71 (31.3) | 156 (68.7%) |
| Pneumococcal | Apply a single dose of PCV13 preferably before the start of immunosuppressive treatment, followed by PPV23 one dose 8 weeks after the initial dose of PCV13, and a further dose of PPV23 5 years after the first dose of PPV23. | 40 (17.6%) | 187 (82.4%) |
| Herpes zoster | Apply prior to synthetic DMARD therapy. Suggested application 2 weeks prior to initiation of biologic therapy and 4 weeks prior to JAK inhibitors. | 9 (4%) | 218 (96%) |
| Human papilloma virus | Administration in women under 26 and men under 21 is suggested. | 2 (.9%) | 225 (99.1%) |
| Hepatitis B | It is suggested for use in surface antigen negative RA patients and those with risk factors for acquiring RA. | 23 (10.1%) | 204 (89.9%) |
| Tetanus, diphtheria, whooping cough | Single dose for those over 19 years of age who have not already received it. | 19 (8.4%) | 208 (91.6%) |
PCV13: 13-valent pneumococcal conjugate vaccine; PCV23: 23-valent pneumococcal conjugate vaccine.
Source: Huang et al.10.
Finally, patients who did not comply with the recommended vaccination schedule were asked about the reason(s) for non-compliance; this question had five response options and patients could choose one or more options. The main reason for non-compliance was lack of knowledge about the indication to be vaccinated in 116 patients (51.1%), followed by 98 patients (43.2%), where their rheumatology doctor at some point advised them not to be vaccinated, 38 patients (16.7%) where doctors other than rheumatology also advised against it, finally 29 patients (12.8%) stated that for their own reasons they did not wish to do so, and 23 patients (10.1%) because the institution did not have the vaccines recommended by their doctor.
DiscussionRA and general patients with AIDs have an increased risk of contracting influenza compared to the general population5 and immunisation is widely recommended and has been shown to be effective in both prevention and reduction of morbidity and mortality. In Mexico, the majority of the population receives a trivalent vaccine with an immunogenicity that has been shown to be optimal in patients treated with any conventional synthetic (sDMARDs) or biological (bDMARDs) disease-modifying drug; except for rituximab, on which there is heterogeneous information, as some authors conclude that it has a lower response in the generation of antibodies11,12; while others show that there are no statistically significant differences in immunogenicity in treatment groups with bDMARDs sDMARDs and combined therapy with bDMARDs and sMARDs, compared to the healthy population; however, a lower rate of immunogenicity against influenza b antigen in the combined therapy group is noteworthy, This study is limited by the small number of participants and the lack of homogeneity with respect to age13. Furthermore, although it is not recommended by clinical guidelines, the suspension of methotrexate two weeks before to two weeks after the application of the vaccine improves the response12,14.
The present study found that 31.3% of patients surveyed had been vaccinated within the last year, a rate below those reported in the United States5 and in Latin America compared with Uruguay and Argentina7.
In the bivariate analysis of our study, we found no significant differences related to adherence in relation to sex, schooling or type of treatment, although patients with postgraduate studies had higher adherence rates.
As with influenza, patients with RA have an increased risk of infection by S. pneumoniae, and the disease is also more severe than in the rest of the population15. In Mexico, two vaccines are available: 23-valent and 13-valent4. In terms of immunogenicity, it has been evaluated with different treatment modalities, in terms of sDMARDs, especially methotrexate16 with antibody levels that persist for up to 10 years. In the case of patients treated with bDMARDs, studies have shown that they do not significantly affect immunogenicity17, with no significant differences between anti-TNF, tocilizumab or rituximab18.
In this study, 17.6% compliance with pneumococcal vaccination was found, lower than that reported in other series and, as with influenza, with non-significant differences in relation to sex, schooling and the treatment strategy employed. It is important to note the low percentage of combined vaccination, as only 12.8% had it, a topic that has not been addressed in other studies.
This research attempts to highlight as a secondary objective the causes for non-compliance with the vaccination schedule by patients, highlighting that the majority 51.1% were unaware that they belonged to a population with specific vaccination indications, and that another large percentage at some point in the evolution of the disease asked their rheumatologist who recommended that they not be vaccinated. Immunisation recommendations have been strengthened by scientific evidence over the last two decades, as there was no research on the immunogenicity and safety of immunisation in these patients.
A French study with a design very similar to the present one found that the main reasons for non-vaccination were forgetfulness and concern about adverse effects, perhaps related to higher rates of adherence on the part of doctors in recommending vaccination and patients in administering it9. A recent publication in northern Mexico asking patients about their knowledge of the influenza vaccine showed that 26.7% of those who had not been vaccinated and 13.5% of those vaccinated considered it unsafe and ineffective, 7.6% said it was not necessary and 11.7% considered that the influenza vaccine could worsen the symptoms of their underlying rheumatic disease19. Based on this, we can conclude that there is very heterogeneous information, especially in the way in which research addresses patient knowledge and the reasons for non-compliance with vaccination schedules; patient ignorance is an important factor in Mexico. Our study addresses an aspect not taken into account in other questionnaires on the role that physicians play in discouraging vaccination, requiring extensive campaigns throughout the country to educate medical personnel on the correct implementation of this practice.
This study has limitations due to the number of patients included, the selection bias, since the study was carried out during the COVID-19 pandemic, which meant that most of the patients surveyed were those receiving intravenous biological therapy. Patients with other treatment modalities only came for drug reformulation and this made it difficult for them to be included. In addition, the hospital where the research was carried out is a national reference centre attended by people with severe RA, of long standing and with failure of several lines of treatment.
In conclusion, this research reveals worrying coverage figures, with opportunities to improve and reinforce the adherence of RA patients to vaccination, emphasising education as a fundamental pillar and opening up opportunities for new studies such as the one cited by Figueroa et al.19, in which knowledge, fears and apprehensions are investigated, not only in patients, but also in doctors.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Tobar-Marcillo M, Guerrero-Solís C, Pool-Valda GO, Irazoque-Palazuelos F, Muñoz-López S. Vacunación contra influenza y neumococo en pacientes con artritis reumatoide. Reumatol Clín. 2023;19:49–52.