Our objective was to describe the variability in the management of spondyloarthritis (SA) in Spain in terms of healthcare resources and their use.
MethodsA review of 1168 medical files of patients seen in randomly selected Spanish hospital rheumatology departments. We analyzed demographic variables and variables related to the consumption of health resources.
ResultsThe total number of visits to rheumatology were 5908 with a rate of 254 visits/100 patient-years. The total number of visits to rheumatology specialty nurses was 775, with a rate of 39 visits/100 patient-years, and there were 446 hospitalizations, representing a rate of 22 per 100 patient-years. The number of admissions due to SA was 89, with a rate of 18 admissions/100 patient-years. Total visits to other specialists were 4307 with a rate of 200/100 patient-years. The total number of orthopedic surgeries was 41, which leads to a rate of 1.8 surgeries/100 patient-years.
ConclusionsThe data regarding visits to the rheumatologist and prosthetic surgery of patients with in Spain are similar to most studies published in our environment, however, other aspects concerning the use of health resources are different compared to other countries. These data may help to understand and improve organizational aspects of management of SA in Spanish hospitals.
Describir la variabilidad en el manejo de las espondiloartritis (EsA) en España en términos de consumo de recursos sanitarios y la utilización de técnicas.
MétodosRevisión de 1.168 historias clínicas de pacientes con EsA atendidos en servicios de reumatología de hospitales españoles, seleccionadas aleatoriamente. Se analizaron las variables sociodemográficas y las variables relacionadas con el consumo de recursos sanitarios.
ResultadosEl número total de visitas médicas a reumatología fue de 5.908, con una tasa de 254 consultas/100 pacientes-año. El número total de visitas a enfermería reumatológica fue de 775, con una tasa de 39 visitas/100 pacientes-año, y se produjeron 446 ingresos, lo que representa una tasa de 22 por 100 pacientes-año. El número de ingresos debidos a la EsA fue de 89, con una tasa de 18 ingresos/100 pacientes-año. El total de visitas a otros especialistas fue de 4.307, con una tasa de 200/100 pacientes-año. El número total de cirugías ortopédicas fue de 41, lo que da lugar a una tasa de 1,8 cirugías/100 pacientes-año.
ConclusionesLos datos de visita al reumatólogo y de cirugía protésica de pacientes con EsA en España son similares a la mayoría de los estudios publicados en nuestro entorno; sin embargo, otros aspectos referentes al uso de recursos sanitarios son diferentes en comparación con otros países. Estos datos pueden contribuir para conocer y mejorar aspectos organizativos del manejo de la EsA en los hospitales españoles.
The eMAR II study is a study of variability in the treatment of rheumatoid arthritis (RA) and spondyloarthritis (SpA) in Spain. We define variability in clinical practice as the differences within a group of patients in relation to any aspect of the same clinical practice.
Variability of clinical practice is a very common phenomenon in medicine, and is responsible for the improper use of different procedures, with a subsequent unnecessary use of resources and possible collateral damage to the patient and costs for the health system.1–8 These reasons justify the need to understand variability, its determinants and effects, in order to design realistic strategies to help improve the quality of clinical practice.
In this sense, the results of the first study of variability in the treatment of RA in Spain (eMAR I), made 10 years ago, showed a wide variability in the use of different health resources, diagnostic procedures and therapeutic monitoring of patients with RA who, in many cases, is independent of the characteristics of the patient or the severity of the disease.7,8
In the 10 years since the eMAR I, care for RA and other inflammatory joint diseases type has undergone a revolution due to various factors including the availability of new treatments, better understanding of these processes, the growth of rheumatology care in our country and the development of other important research. The eMAR II evaluates the potential impact of these events in the practices of management of RA and in SpA. In the latter group of diseases has been is poorly studied.9,10 The objective of this paper is to describe the variability in the management of SpA in Spain in terms of healthcare resource utilization (physician visits, hospitalizations, etc.) and the use of techniques (radiography, ultrasound, etc.). The results of this study may serve greatly in the constant improvement of management of patients in our country.
Material and methodsDesign, Patient Selection and Data AcquisitionThe eMAR II study (2009–2010) is a cross-sectional study designed to analyze variability in the management of patients with RA in Spain.11 100 hospitals were contacted, 46 accepted and 54 rejected participation.
The sample consisted of medical records or files of patients seen in rheumatology departments of Spanish hospitals with at least one visit to a rheumatologist in the 2 years preceding the date of study onset. We performed a stratified random sampling of regions (CC. AA.), of second level hospitals (first-level units or UPE) and patients (second-stage units). To avoid the lack of representation associated with the homogeneity of UPE of very different size in the first stage, sampling with probability proportional to its size was performed and a random selection was carried out, equiprobabilistic of patients in each center. The smaller CC. AA. were clustered with larger ones in order to get all of them represented.
Once the sampling of centers was done, we contacted them requesting a list of all patients diagnosed with RA and SpA who had been treated during the 2 years prior to the start of the study at least once. Upon receipt of these lists, we conducted a random sampling of patients in each center for inclusion into the study.
The sample size was calculated according to the hypothesis that the proportion of patients who have needed an intervention has risen from 18% in eMAR I to 26% in eMAR II. Under this assumption and with an alpha error of 5%, a power of 80%, taking into account 15% of unlocalized or incomplete files, with a design effect of 2.5, we obtained a sample size of 1410 patients for each of the study arms (one for the RA and the other for SpA).
The data for the past 2 years were extracted from the patient's history and collected in standardized data collection databases, writing up “Instructions” to complete. They were subsequently entered into an electronic database specifically designed for this research project.
VariablesWe collected: (a) sociodemographic variables: age, sex, marital status, education level, place of residence, distance to the hospital from the place of residence, (b) clinical data: age at onset of SpA, duration of disease, and (c) variables related to the consumption of health resources: medical visits and rheumatology nursing service needs, medical visits to other departments and its use by rheumatology, number and type of non-medical visits, hospital admissions (number, cause, department, relationship with SpA), orthopedic events (number, type, infections, infections, complications, comorbidity, death), additional tests (laboratory, imaging, etc.), consumption of drugs (non steroidal anti-inflammatory drugs [NSAIDs], glucocorticoids, disease-modifying drugs [DMARD]).
Statistical AnalysisWe performed a descriptive analysis of the dependent and independent variables using measures of central tendency (mean or median) and dispersion (standard deviation and 25 and 75 quartile) for continuous variables, as adjusted for not normally distributions, and percentages for qualitative variables. We calculated the total number, the average value, expressed as median, and the rate of different health resources. For the calculation of rates we used, as the numerator, the total of each resource, and as the denominator the number of patients with information using that resource multiplied by 2 years of exposure.
The estimates were adjusted to the sampling design using the svy commands in Stata 9.0 (StataCorp, College Station, USA).
ResultsSociodemographic Characteristics of PatientsOf the estimated sample (n=1410), valid information was obtained for 1168 patients with SpA, which represents 82.8% of the theoretical sample. The origins of the patients in relation to CC. AA. were as follows: Andalucía, Ceuta and Melilla: 204, Asturias, Cantabria and the Basque Country: 77; Balearics and Valencia: 90, Canary 79, Castile and Leon and Extremadura: 148; Castilla-La Mancha and Murcia: 84; Catalonia: 148; Galicia: 23; Madrid: 224, and Navarra, La Rioja and Aragon: 90.
Of the patients included, 68% were male. The median age (P25–P75) was 49.2 (39.7–60.5) years, median age of onset of SpA was 30.4 (23.2–39.8) years and the duration of disease 105.1 (48.4–192.5) months. Although some variables were not available in a number of patients, it should be noted that most were married (79%) and had some form of education (95%). About half of patients that lived in the same town in which the hospital stood and for those who resided in a different location, distance to hospital was more frequently between 20 and 50km.
52.8% of patients had an active working life for more than 50% of the study period of 2 years, with 8.3% of cases presenting periods of temporary disability, and a median number of episodes of temporary disability of one.
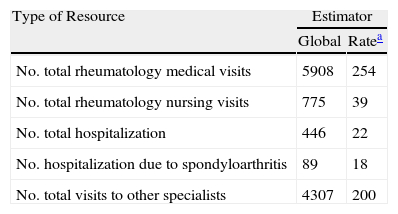
Resource ConsumptionValuesThe total number of visits to rheumatology was 5908, with a median of 4 (3–6) and a rate of 254 visits/100 patient-years. The total number of rheumatology nursing visits was 775, with a rate of 39 visits/100 patient-years, and there were 248 admissions, representing a rate of 22 per 100 patient-years. The number of admissions due to SpA was 89, with a rate of 18 admissions/100 patient-years. Total visits to other specialists were of 4307 (a rate of 200/100 patient-years). Over half of these patients did not undergo nursing visits or hospital admissions (see Table 1).
Global Value, Rate and Average of the Different Assistance Resources Consumed by Patients with Spondyloarthritis in the Past 2 Years.
| Type of Resource | Estimator | |
| Global | Ratea | |
| No. total rheumatology medical visits | 5908 | 254 |
| No. total rheumatology nursing visits | 775 | 39 |
| No. total hospitalization | 446 | 22 |
| No. hospitalization due to spondyloarthritis | 89 | 18 |
| No. total visits to other specialists | 4307 | 200 |
| Median (P25–P75) | |
| No. rheumatology medical visits | 4,0 (3.0–6.0) |
| No. rheumatology nursing visits | 0 (0–0) |
| No. hospitalization | 0 (0–0) |
| No. visits to other specialists | 2 (0–5) |
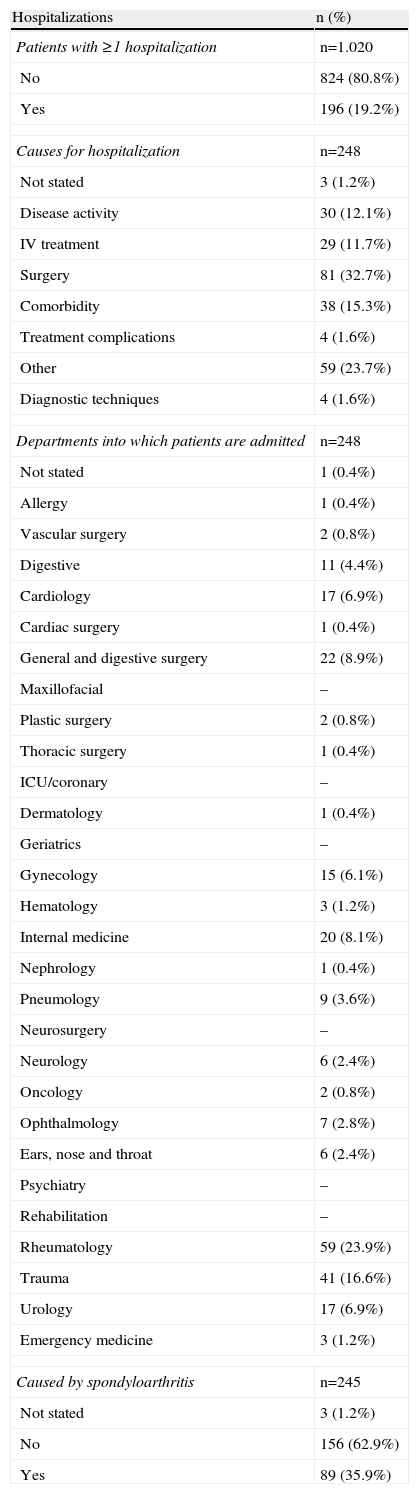
19% of the patients experienced at least one hospitalization during the 2-year study. Total hospitalizations were 248 (Table 2). The most common causes of admission were surgery (32.7%), presence of comorbidity (15.3%) and disease activity (12.1%).
Hospitalizations in the Past 2 Years: Number, Causes and Departments.a
| Hospitalizations | n (%) |
| Patients with ≥1 hospitalization | n=1.020 |
| No | 824 (80.8%) |
| Yes | 196 (19.2%) |
| Causes for hospitalization | n=248 |
| Not stated | 3 (1.2%) |
| Disease activity | 30 (12.1%) |
| IV treatment | 29 (11.7%) |
| Surgery | 81 (32.7%) |
| Comorbidity | 38 (15.3%) |
| Treatment complications | 4 (1.6%) |
| Other | 59 (23.7%) |
| Diagnostic techniques | 4 (1.6%) |
| Departments into which patients are admitted | n=248 |
| Not stated | 1 (0.4%) |
| Allergy | 1 (0.4%) |
| Vascular surgery | 2 (0.8%) |
| Digestive | 11 (4.4%) |
| Cardiology | 17 (6.9%) |
| Cardiac surgery | 1 (0.4%) |
| General and digestive surgery | 22 (8.9%) |
| Maxillofacial | – |
| Plastic surgery | 2 (0.8%) |
| Thoracic surgery | 1 (0.4%) |
| ICU/coronary | – |
| Dermatology | 1 (0.4%) |
| Geriatrics | – |
| Gynecology | 15 (6.1%) |
| Hematology | 3 (1.2%) |
| Internal medicine | 20 (8.1%) |
| Nephrology | 1 (0.4%) |
| Pneumology | 9 (3.6%) |
| Neurosurgery | – |
| Neurology | 6 (2.4%) |
| Oncology | 2 (0.8%) |
| Ophthalmology | 7 (2.8%) |
| Ears, nose and throat | 6 (2.4%) |
| Psychiatry | – |
| Rehabilitation | – |
| Rheumatology | 59 (23.9%) |
| Trauma | 41 (16.6%) |
| Urology | 17 (6.9%) |
| Emergency medicine | 3 (1.2%) |
| Caused by spondyloarthritis | n=245 |
| Not stated | 3 (1.2%) |
| No | 156 (62.9%) |
| Yes | 89 (35.9%) |
IV: intravenous.
Hospital services with the highest percentage hospitalizations in patients with SpAs were trauma (16.7%), rheumatology (23.9%), internal medicine (8.1%) and general and digestive surgery (8.9%). Other services had a percentage of hospitalizations of less than 7%.
Of the 245 patients who responded to specific questions, 89 (35.9%) had been hospitalized due to SpA. Finally, the most common causes of hospitalization due to rheumatic disease were similar: surgery (32.6%), disease activity (31.5%), administration of IV therapy (32.6%), comorbidity (4.5%) and complications of treatment (3.4%).
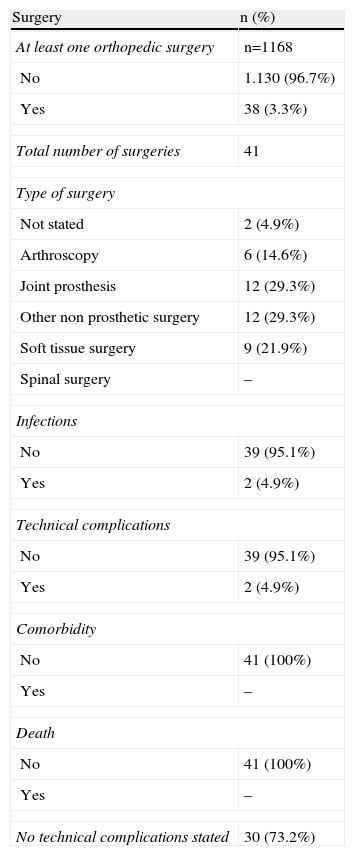
Orthopedic SurgeryA total of 38 SpA patients had at least one event of orthopedic surgery, which represents 3.3% over a duration of 8.8 years, respectively. However, given that the same patient may have undergone several surgeries, the total number of these was 41, which gives rise to a rate of 1.8 surgeries/100 patient-years (Table 3).
Orthopedic Surgery: Type and Morbidity/Mortality in the Past 2 Years.
| Surgery | n (%) |
| At least one orthopedic surgery | n=1168 |
| No | 1.130 (96.7%) |
| Yes | 38 (3.3%) |
| Total number of surgeries | 41 |
| Type of surgery | |
| Not stated | 2 (4.9%) |
| Arthroscopy | 6 (14.6%) |
| Joint prosthesis | 12 (29.3%) |
| Other non prosthetic surgery | 12 (29.3%) |
| Soft tissue surgery | 9 (21.9%) |
| Spinal surgery | – |
| Infections | |
| No | 39 (95.1%) |
| Yes | 2 (4.9%) |
| Technical complications | |
| No | 39 (95.1%) |
| Yes | 2 (4.9%) |
| Comorbidity | |
| No | 41 (100%) |
| Yes | – |
| Death | |
| No | 41 (100%) |
| Yes | – |
| No technical complications stated | 30 (73.2%) |
The most common types of surgery were joint prosthesis (14.6%), surgery without prostheses (29.3%) and soft tissue interventions (21.9%). Only 2 underwent arthroscopies (4.9%). The most common causes of surgical morbidity were infections (4.9% of interventions) although the lack of surgical complications was more frequent (73.2%).
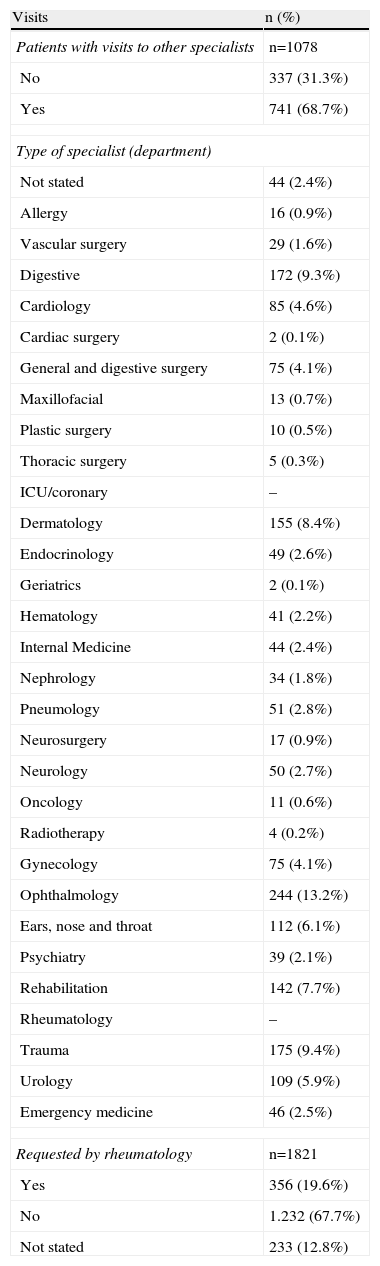
Visits to Other Specialists68.7% of patients with SpA had made at least one visit to other medical specialists (Table 4) in the past 2 years, with a median of 2 (0–5) and the total number of consultations 4307, representing a rate of 199.8 visits to other specialists/100 patient-years (Table 1).
Visits to Other Specialists in the Past 2 Years.
| Visits | n (%) |
| Patients with visits to other specialists | n=1078 |
| No | 337 (31.3%) |
| Yes | 741 (68.7%) |
| Type of specialist (department) | |
| Not stated | 44 (2.4%) |
| Allergy | 16 (0.9%) |
| Vascular surgery | 29 (1.6%) |
| Digestive | 172 (9.3%) |
| Cardiology | 85 (4.6%) |
| Cardiac surgery | 2 (0.1%) |
| General and digestive surgery | 75 (4.1%) |
| Maxillofacial | 13 (0.7%) |
| Plastic surgery | 10 (0.5%) |
| Thoracic surgery | 5 (0.3%) |
| ICU/coronary | – |
| Dermatology | 155 (8.4%) |
| Endocrinology | 49 (2.6%) |
| Geriatrics | 2 (0.1%) |
| Hematology | 41 (2.2%) |
| Internal Medicine | 44 (2.4%) |
| Nephrology | 34 (1.8%) |
| Pneumology | 51 (2.8%) |
| Neurosurgery | 17 (0.9%) |
| Neurology | 50 (2.7%) |
| Oncology | 11 (0.6%) |
| Radiotherapy | 4 (0.2%) |
| Gynecology | 75 (4.1%) |
| Ophthalmology | 244 (13.2%) |
| Ears, nose and throat | 112 (6.1%) |
| Psychiatry | 39 (2.1%) |
| Rehabilitation | 142 (7.7%) |
| Rheumatology | – |
| Trauma | 175 (9.4%) |
| Urology | 109 (5.9%) |
| Emergency medicine | 46 (2.5%) |
| Requested by rheumatology | n=1821 |
| Yes | 356 (19.6%) |
| No | 1.232 (67.7%) |
| Not stated | 233 (12.8%) |
The distribution of services most frequently consulted was: ophthalmology (13.2%), trauma (9.4%) and digestive (9.3%). Interestingly, consultation with other rheumatology service was requested by 19.6% of cases (Table 4).
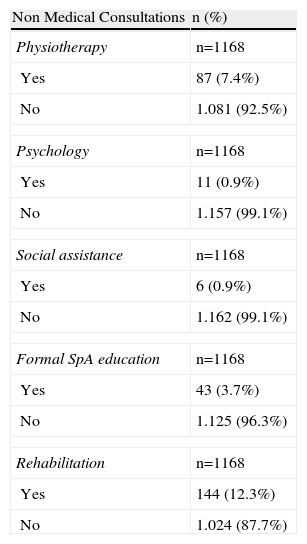
In relation to medical consultations, as shown in Table 5, the proportion of patients who underwent these was less than 8%, the most common being visits to physiotherapists. Another aspect to consider is that 12.3% of patients had a rehabilitation session made during the study period. Finally, more than half of the patients did not make any visits to other non-medical professionals, resulting in median values of 0 (Table 5).
Non Medical Personnel Consulted by the Patients With Spondyloarthritis in the Past 2 Years.
| Non Medical Consultations | n (%) |
| Physiotherapy | n=1168 |
| Yes | 87 (7.4%) |
| No | 1.081 (92.5%) |
| Psychology | n=1168 |
| Yes | 11 (0.9%) |
| No | 1.157 (99.1%) |
| Social assistance | n=1168 |
| Yes | 6 (0.9%) |
| No | 1.162 (99.1%) |
| Formal SpA education | n=1168 |
| Yes | 43 (3.7%) |
| No | 1.125 (96.3%) |
| Rehabilitation | n=1168 |
| Yes | 144 (12.3%) |
| No | 1.024 (87.7%) |
| Median (P25–P75) | |
| No. visits to other non medical personnel | 0 (0–1) |
SpA: Spondyloarthropathies.
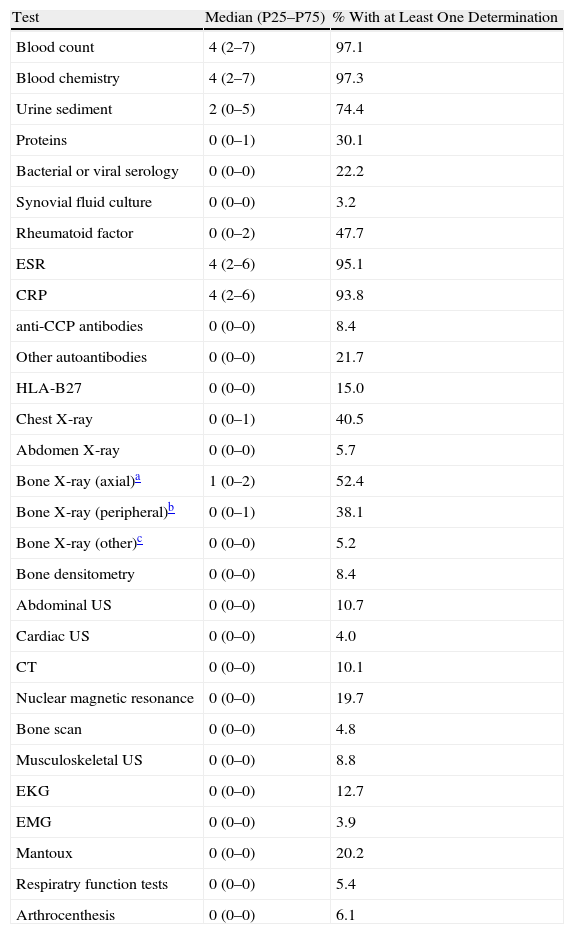
Testing The tests performed more frequently in patients in the past 2 years were: blood count, biochemistry, and erythrocyte sedimentation rate (the median values of all three was 4), C reactive protein (median 4) and urinary sediment (median 2) We noted that more than half of the patients had no HLA-B27 determination, which produces a median of 0 (Table 6).
Laboratory, Imaging and Other Tests Performed on Patients With Spondyloarthritis in the Past 2 Years.
| Test | Median (P25–P75) | % With at Least One Determination |
| Blood count | 4 (2–7) | 97.1 |
| Blood chemistry | 4 (2–7) | 97.3 |
| Urine sediment | 2 (0–5) | 74.4 |
| Proteins | 0 (0–1) | 30.1 |
| Bacterial or viral serology | 0 (0–0) | 22.2 |
| Synovial fluid culture | 0 (0–0) | 3.2 |
| Rheumatoid factor | 0 (0–2) | 47.7 |
| ESR | 4 (2–6) | 95.1 |
| CRP | 4 (2–6) | 93.8 |
| anti-CCP antibodies | 0 (0–0) | 8.4 |
| Other autoantibodies | 0 (0–0) | 21.7 |
| HLA-B27 | 0 (0–0) | 15.0 |
| Chest X-ray | 0 (0–1) | 40.5 |
| Abdomen X-ray | 0 (0–0) | 5.7 |
| Bone X-ray (axial)a | 1 (0–2) | 52.4 |
| Bone X-ray (peripheral)b | 0 (0–1) | 38.1 |
| Bone X-ray (other)c | 0 (0–0) | 5.2 |
| Bone densitometry | 0 (0–0) | 8.4 |
| Abdominal US | 0 (0–0) | 10.7 |
| Cardiac US | 0 (0–0) | 4.0 |
| CT | 0 (0–0) | 10.1 |
| Nuclear magnetic resonance | 0 (0–0) | 19.7 |
| Bone scan | 0 (0–0) | 4.8 |
| Musculoskeletal US | 0 (0–0) | 8.8 |
| EKG | 0 (0–0) | 12.7 |
| EMG | 0 (0–0) | 3.9 |
| Mantoux | 0 (0–0) | 20.2 |
| Respiratry function tests | 0 (0–0) | 5.4 |
| Arthrocenthesis | 0 (0–0) | 6.1 |
Anti-CCP: anti-CCP antibody, EKG electrocardiogram, EMG: electromyogram, HLA-B27: human leukocyte antigen B27; US: ultrasound; X-ray: plain film, CT: CT scan, CRP C-reactive protein, ESR: erythrocyte sedimentation rate.
With regard to imaging, the most demanded study was plain X-ray with axial projection (median=1). The rest of the tests showed median values of 0 because they were not performed in most patients. The same results were observed for other tests such as respiratory function tests and arthrocentesis (Table 6).
Use of Drugs81.2% of patients had received NSAIDs for SpA in the past 2 years, 33% on demand. Only 20% had used glucocorticoids and 62.6% some kind of DMARD, of which almost 100% were methotrexate or sulfasalazine.
DiscussionVariability in clinical practice refers to the differences we find in it. That is, patients are not always managed the same way. The variability in clinical practice is admissible if, for example, there is no evidence that a particular technique, system or drug is superior to the rest, when the specific characteristics and preferences of patients so require it, or when resources are not available. However, it is unacceptable when it is caused by deficiencies in the skills of the physician, poor organization of the institution, ignorance or a deliberate decision not to use a practices for which there is proven evidence of superiority, which may seriously harm the patient and consume resources unnecessarily.
Although not always easy to prove, it seems that there are differences in management (variability) of SpA (among countries, hospitals, doctors, etc.), More specifically the use of diagnostic, monitoring or drug therapy and rehabilitation. At times it may even appear that, as a result of this variability, improper use of resources may occur, that is, these differences cannot be justified by the severity of illness, patient preferences, and so on.
The data we have presented come from the eMAR II study and allow us to know the use of health resources in patients with SpAs in Spain. Among the variables collected we find visits to physicians and other professionals, hospital admissions, orthopedic surgery, additional tests and the consumption of drugs. They are all important variables in our clinical practice.
On the other hand, random selection of centers and patients makes the results reliably reflect how we are managing health resources in our country and the representativeness of the sample relative to the general population. In addition, we have included community hospitals with under 200 beds and large reference hospitals with more than 1000 beds and other exclusive hospital with additional outpatient care.
As for the results obtained in relation to medical visits, we found that, on average, patients visited the rheumatologist at least 4 times a year. Quite similar results have been found in Germany,12 Canada,13 United States.14 or Brazil,15 although not all of these studies included the full spectrum of SpA.
On the other hand, in relation to visits to other specialists, our study found a median of 2 visits. This information was not collected equally in the published series, so comparison is difficult. However, it is curious that most of them were not requested by the rheumatologist. And although it is possible that other reasons exist for not asking for consultations related to SpA, if we consider that the services most frequently visited in our study were ophthalmology, orthopedics, digestive and dermatology, it is reasonable to assume that many of them really did have a relationship with SpA.
Non-medical consultations made by patients with SpA were generally very low. These include physiotherapy, psychology, social worker or education, and were significantly lower than those reported in other series.13,16 These differences may be due to the fact that their severity was different but in the case of SpA in our country also that these resources were being underused or there was no access to them.
Following hospital admission, they were not very common, being the most common surgery, followed by co-morbidity and disease activity. Less than half were directly related to the ESA. In other countries have reported income rates rather similar to those reported in this trabajo.12 Other studies have also shown that the average hospital stay for these patients is small, one or a few days.16–19
The rate of orthopedic surgery in our study was very low, the most frequent procedure being joint prosthesis, non-prosthetic surgeries and soft tissue surgeries. There were no surgical complications in most cases. Other studies have found low rates of orthopedic surgery in patients with SpA.13,19,20 This is most likely due to the average age of these patients, which was clearly inferior to those with other diseases such as RA or osteoarthritis of the knee and hip.
Finally, in regard to additional laboratory testing, the most frequent were blood count, biochemistry and ESR, with a median of 4. Compared with other studies, our median is slightly inferior,16,21 although a single study that measured the number of laboratory tests per patient per year showed it to be very elevated.15
The most common imaging tests were plain X-rays with axial projection (including cervical, thoracic, lumbar, iliac or pelvis) with a median of one. Other imaging or additional tests were not performed in most patients. The case of skeletal X-rays calls our attention, because on the basis of various consensus and practice guidelines published in our country,9,10,22,23 and used either for the evaluation of the disease or in the context of biological therapies, a greater number of some of them would be expected.
In summary, our work has been detailed the use of healthcare resources by patients with SpA in Spain. Visit data to the rheumatologist and prosthetic surgery are similar to most studies published in our environment, but other aspects concerning the use of health resources are different from what was expected and/or different compared to other countries. Furthermore, these data may contribute to understand and improve organizational aspects of management of SpA in Spanish hospitals.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence is in possession of this document.
Conflict of InteresteMAR II study was funded by Abbott Laboratories.
emAR II study group: C. Escudero, N. Chozas, I. Maries, A. Fernandez, F. Medina, I. Ureña, V. Irigoyen, M. Lopez, P. Espiño, S. Manrique, E. Collantes, P. Font, D. Ruiz, M. Granados, M.J. Pozuelo, I. Moreno, J.M. Pina, R. Roselló, C. Vázquez, J. Beltrán, F.J. Manero-Ruiz, A. Pecondón, E. Giménez, F. Jimenez, J. Marzo, M. Medrano, J. Babío, T. Tinturé, S. González, C. Ordás, M.E. García, L. Espadaler, J. Fernandez, J. Fiter, A. Naranjo, S. Ojeda, J. Tornero, J.A. Piqueras, E. Júdez, C. López, J. Medina, G. Iglesias, M. Alvarez, J. Alegre, M.R. Colazo, J.L. Alonso, B. Alvárez, C. Montilla, S. Gómez, R. López, M. Sánchez, S. Castro, S. Ordóñez, D. Boquet, J. Calvet, D. de la Fuente, V. Rios, M. Nolla, A. Martínez-Cristóbal, R. Negueroles, M.L. Muñoz, J. García, F. Gamero, E. del Rincón, E. Pérez-Pampín, L. Fernandez, R. Miguélez, A.M. Ortíz, E. Vicente, S. Pérez Esteban, E. Tomero, A. Casado, M.J. Arias, E. Cuende, C. Bohorquez, J.M. Rodríguez, A. Aragón, J. García, J. Zubieta, A. Gallego, C. Martínez, I. Mateo, A. de Juanes, E. Enríquez, I. Monteagudo, F.J. López-Longo, E. Pagán, M.J. Rubira, P. Mesa, J. Galvez, E. Saiz, C. Tornero, E. Úcar, C. Rodríguez, B. González Álvarez, N. Rivera, F.X. Arasa, S. Bustabad, E. Delgado, J. Maese and R. Veroz.
Please cite this article as: Jovani V, et al. Variabilidad en el consumo de recursos en pacientes con espondiloartritis en España. Datos descriptivos preliminares del estudio emAR II. Reumatol Clin. 2012;8:114-9.