We present the case of a woman of 69 years of age with dermatomyositis complicated with interstitial lung disease for the past 7 years, azathioprine and corticosteroids at an initial dose of 60mg/day of prednisone for 6 weeks, with subsequent progressive decrease at 5mg each week until 20mg/day, decreasing 2.5mg every 2 weeks until a maintenance dose of 5–10mg/day was reached. Osteoporosis was diagnosed 3 years earlier, with a bone densitometry: lumbar spine 0.752g/cm2, T −3.0 SD; femoral neck 0.531g/cm2, T −2.9 SD, treated with alendronate 70mg weekly, 1000mg/day of calcium and 400U/day of vitamin D.
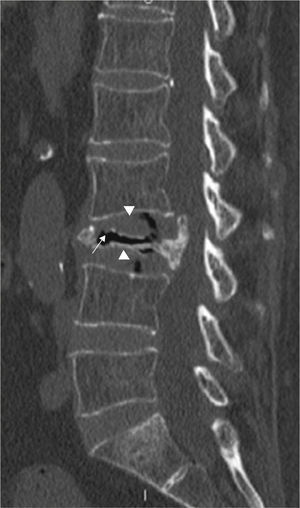
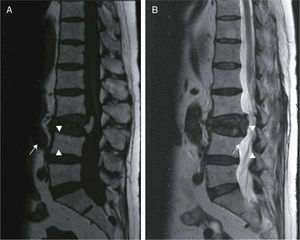
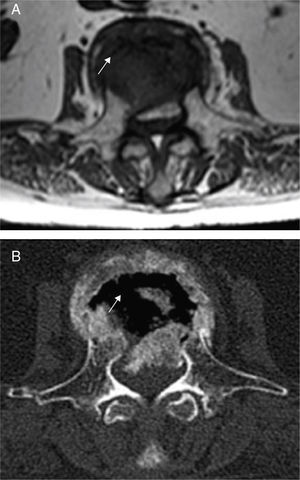
She consulted for low inflammatory back pain lasting 4 weeks, with no history of trauma, fever or constitutional symptoms. The lateral lumbar spine X-ray showed a fracture of L3 due to collapse with intravertebral vacuum phenomenon (IVVF), suggesting vertebral osteonecrosis (ON). Computed tomography (CT) and magnetic resonance imaging (MRI) confirmed this diagnosis (Figs. 1–3). Surgical fixation was performed of the area. The study showed histological signs of bone avascular necrosis: trabecular bone tissue with extensive areas of necrosis, medullary space with proliferation of granulation tissue, few hematopoietic elements, necrosis and cellular debris.
ON is a rare entity characterized by vertebral collapse and the presence of IVVF.1,2 The most common location is the thoraco-lumbar junction. It usually occurs in older patients and/or pre-osteoporosis. In fact, today there are still discrepancies on whether it is a case of vertebral osteonecrosis that subsequently collapses, or a vertebral fracture due to osteoporosis, which leads to a certain amount of local bone ischemia (the fracture produces a compaction of the spongy bone and difficult blood flow). Other factors related to the appearance of this entity are alcohol abuse, mild trauma, radiation or prolonged treatment with steroids.1 Although there is a greater involvement of the anterior part of the vertebra (which coincides with the most affected area of vascularization) and in some cases neurological, complications can occur by displacement of the rear wall conditioning spinal canal stenosis.
IVVF, although not pathognomonic, is the most characteristic radiographic sign of this entity and often suggests the diagnsis.3,4 This sign reflects the presence of gas within the bone (mainly nitrogen) and in adjacent tissues. IVVF can be seen in radiographs, a linear or crescent-shaped radiolucent image usually located adjacent to the superior endplate, which appears or is enhanced by the extension, and decrease or even disappears with flexion of the spine. Sometimes it can be detected by CT or MRI because of its greater sensitivity.
In conclusion, the presence of IVVF, along with the appropriate clinical context, enables the diagnosis of ON. In general terms, this sign does not usually occur in neoplasia where these fractures and the vertebral body is filled with tumor cells (although there is a case described in multiple myeloma).3 Infection by anaerobic microorganisms may form gas in the intervertebral disc and adjacent bone, but is very infrequent.3,4
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence is in possession of this document.
Please cite this article as: Martín-Esteve I, et al. Osteonecrosis vertebral como complicación del tratamiento con glucocorticoides: el fenómeno del vacío intravertebral. Reumatol Clin. 2012;8:375–7.