A large number of complications have been associated with rheumatoid arthritis (RA), those of infectious aetiology being of special relevance. Their high incidence is closely linked to the use of immunosuppressive medication.
The spectrum of agents causing opportunistic infections in patients with RA is very broad; however, there are relatively few cases of Leishmania infection, especially in patients not being treated with biological drugs.
Los pacientes con artritis reumatoide (AR) pueden presentar un número amplio de complicaciones, siendo de especial importancia las de etiología infecciosa. Su elevada incidencia está muy ligada al uso de inmunosupresores.
El espectro de agentes causantes de infecciones oportunistas en pacientes con AR es muy amplio; sin embargo, son relativamente escasos los casos de infección por Leishmania, especialmente en pacientes sin tratamiento con fármacos biológicos.
Leishmaniasis is a protozoal intracellular infection caused by the bite of a dipteral insect. The development of the disease depends on the virulence of the parasite and host risk factors, essentially the state of their immune system. Patients with rheumatoid arthritis (RA) are chronically treated with methotrexate and other immunosuppressants and are therefore at risk of developing infections.1 The spectrum of opportunistic infections is very broad in these patients, however, cases of leishmaniasis are rare, especially in patients treated only with methotrexate.
Clinical caseWe present the case of an 84-year-old male, resident of a southern area of Madrid (an area with a high rabbit population), with a personal history of hypertension, diabetes mellitus, dyslipidaemia, heart failure with atrial fibrillation, with pacemaker implantation due to a third degree atrioventricular heart block, diagnosed 6 years earlier with RA with positive rheumatoid factor, positive anti-cyclic citrullinated peptide antibodies, treated with weekly methotrexate 15mg, with good clinical response. Admitted due to fever, shivering and chills over one week. On physical examination slight bibasalar crackles were observed. No adenopathies, visceromegaly or other data of infectious disease were observed. Analytical tests revealed pancytopenia (haemoglobin 10.9g/dl, 2050 leukocytes with 1310neutrophils/μl and 49,000 platelets/μl), C reactive protein (CPR) 104mg/l and erythrocyte sedimentation rate 110mm/h. Initially medullary toxicity by methotrexate was suspected, with probable bacterial superinfection.
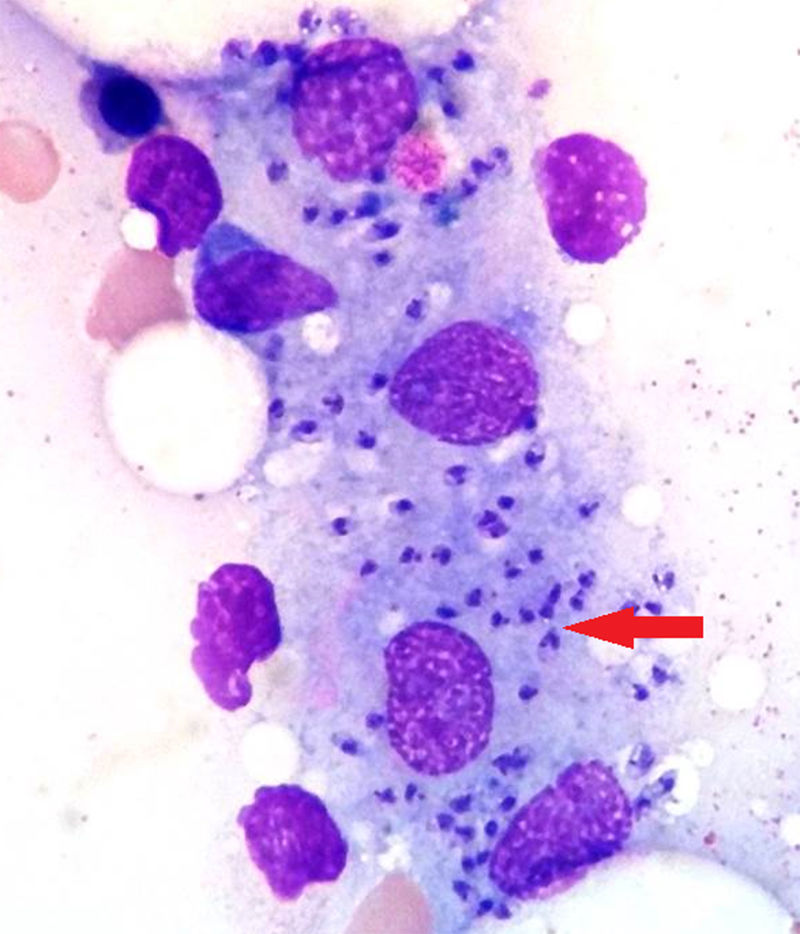
The methotrexate was suspended and several microbiological tests (blood cultures, urine culture, sputum culture, viral and bacterial serologies) and imaging tests (thoracic-abdominal computed tomography, transthoracic and transoesophageal echocardiography) were requested, all of which were not diagnostic of the patient's current condition. Treatment with folic acid and broad-spectrum empirical antibiotics was initiated. Given the persistence of fever and pancytopenia, a bone marrow biopsy was performed to diagnose visceral leishmaniasis (Fig. 1). Serology for Leishmania was positive (titre 1/640) as was polymerase chain reaction (PCR) in the bone marrow biopsy and peripheral blood culture. By contrast, peripheral blood culture was negative. Treatment was started with liposomal amphotericin B 200mg IV initially every 4 days until reaching a cumulative dose of 2400mg. When the treatment was completed, the patient had recovered from the pancytopenia, showed a decrease in antibody titres, and CPR in blood remained negative.
DiscussionLeishmaniasis is a zoonosis caused by more than 20 species of intracellular protozoa of the genus Leishmania. It is transmitted through the bite of an infected female diptera (Phlebotomus and Lutzomya genuses). Mammals act as reservoirs, the most important in our environment being dogs and rodents.
The infection may be asymptomatic, localised or disseminated (mucocutaneous or visceral). According to the World Health Organisation, there are between 900,000 and 1.3 million new cases each year worldwide; of these, between 200,000 and 400,000 have the visceral form. In the Mediterranean basin the infection is due to Leishmania infantum (Leishmania donovani complex), responsible for the visceral form. This is characterised by fever, weight loss, hepatosplenomegaly and pancytopenia. Progression of the disease depends on the aggressiveness of the parasite and on host risk factors such as immunosuppression. The activation of the cell-specific immune response of T helper 1 lymphocytes and the production of macrophage-activating cytokines, such as gamma interferon, interleukin 12 and tumour necrosis factor alpha TNF-α), play an essential role in defence against the disease. Methotrexate inhibits neutrophil chemotaxis and T lymphocyte proliferation, decreasing macrophage activation and response against the parasite.
Diagnosis can be made from tissue samples (skin, spleen, bone marrow or lymph nodes) by direct visualisation of the parasite, culture or quantification of DNA by CRP. CRP and antibody detection by ELISA or indirect immunofluorescence are performed from peripheral blood.1
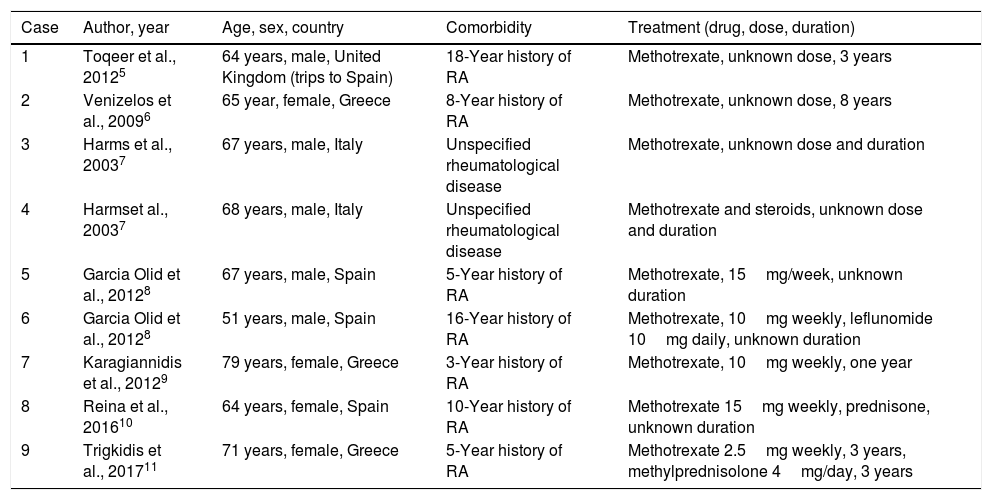
ConclusionsRA affects .5%–1% of the world's population and most patients are treated with methotrexate.2 Multiple cases of visceral leishmaniasis have been described in patients with RA on biological therapy, especially in treatment with anti-TNF, but after a review of the literature we found only 9 cases published on patients treated with methotrexate alone, almost all of them in the Mediterranean area (Table 1) and, given the few cases, it is difficult to establish a subgroup of patients that is more susceptible to the infection.
Cases of visceral leishmaniasis in patients treated with methotrexate described in the literature.
| Case | Author, year | Age, sex, country | Comorbidity | Treatment (drug, dose, duration) |
|---|---|---|---|---|
| 1 | Toqeer et al., 20125 | 64 years, male, United Kingdom (trips to Spain) | 18-Year history of RA | Methotrexate, unknown dose, 3 years |
| 2 | Venizelos et al., 20096 | 65 year, female, Greece | 8-Year history of RA | Methotrexate, unknown dose, 8 years |
| 3 | Harms et al., 20037 | 67 years, male, Italy | Unspecified rheumatological disease | Methotrexate, unknown dose and duration |
| 4 | Harmset al., 20037 | 68 years, male, Italy | Unspecified rheumatological disease | Methotrexate and steroids, unknown dose and duration |
| 5 | Garcia Olid et al., 20128 | 67 years, male, Spain | 5-Year history of RA | Methotrexate, 15mg/week, unknown duration |
| 6 | Garcia Olid et al., 20128 | 51 years, male, Spain | 16-Year history of RA | Methotrexate, 10mg weekly, leflunomide 10mg daily, unknown duration |
| 7 | Karagiannidis et al., 20129 | 79 years, female, Greece | 3-Year history of RA | Methotrexate, 10mg weekly, one year |
| 8 | Reina et al., 201610 | 64 years, female, Spain | 10-Year history of RA | Methotrexate 15mg weekly, prednisone, unknown duration |
| 9 | Trigkidis et al., 201711 | 71 years, female, Greece | 5-Year history of RA | Methotrexate 2.5mg weekly, 3 years, methylprednisolone 4mg/day, 3 years |
Between 2009 and 2012 there was an outbreak of leishmaniasis in the Community of Madrid, affecting 446 people. Of the 160 patients with visceral leishmaniasis, 25 were on immunosuppressive therapy.3,4
In conclusion, the presence of fever and pancytopenia in a patient with cell immunosuppression in an endemic area makes it necessary to rule out leishmaniasis. Exclusive therapy with methotrexate (without biological treatments) in RA may be sufficient to increase the risk of this infection. Bone marrow biopsy enables diagnosis of visceral leishmaniasis, as well as ruling out other causes of pancytopenia.1
Ethical disclosuresProtection of human and animal subjectsThe authors declare that neither human nor animal testing has been carried out under this research.
Confidentiality of dataThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
To the haematology department of the Ramón y Cajal Hospital for their collaboration.
Please cite this article as: Loarce-Martos J, Garrote-Corral S, Gioia F, Bachiller-Corral J. Leishmaniasis visceral en un paciente con artritis reumatoide en tratamiento con metotrexato. Reumatol Clin. 2019;15:e130–e132.