Gout is an inflammatory disease characterized by deposition of monosodium urate (MSU) crystals in joints and tissues in the presence of hyperuricemia.1 The definitive diagnosis is based on the patient's history, typical symptoms and subsequent microscopy verification of crystals.2 Different imaging techniques can be helpful in the diagnosis, especially in those whom joint aspiration is not successful.3 Ultrasound (US) is a simple imaging technique that has gained interest in the assessment of individuals with gout due to its ability to identify inflammation and joint damage, as well as crystal deposition. The most characteristic gout US findings are the presence of intra-articular aggregates and the double contour (DC) signal, included in the 2015 ACR/EULAR classification criteria.4
We conducted a cross-sectional study including 57 gout patients and 32 individuals with normal uricemia, matched by age and gender. Sociodemographic, clinical and analytical data were collected. Bilateral US grey scale evaluation of the 1st metatarsophalangeal joint (MTP1), 2nd metacarpophalangeal (MCP2) and knee was performed in all participants by a single rheumatologist experienced in musculoskeletal US, using a 6–15MHz linear probe of a LOGIQ S8 equipment. The findings assessed were intra-articular effusion, synovial hypertrophy, bone erosion, DC signal and intra-articular MSU aggregates, taking in account the OMERACT definitions.5,6 Parametric and non-parametric tests were used to comparative analysis and the level of significance was defined as p<0.05.
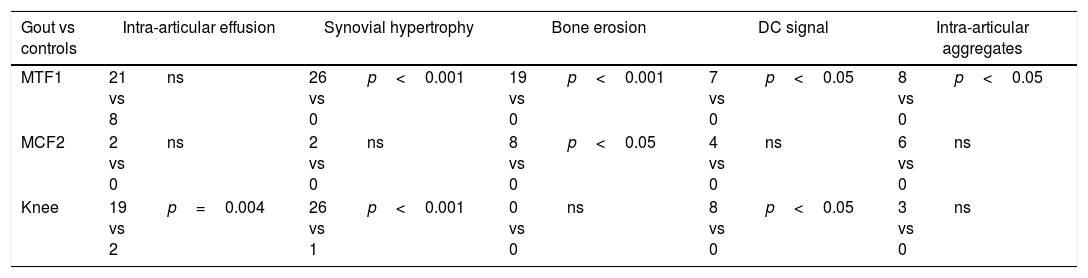
The mean age of gout patients was 63.3±12.6 years. The majority of the gout patients were male; 77.2% had previous history of podagra and 26.3% had tophi. Mean disease duration was 4.3 years. Mean uricemia was 6.7±2.0mg/dl in gout patients and 4.9±0.9mg/dl in the control group. At the time of the study, 73.7% of patients were on urate lowering therapy. As shown in Table 1, in the MTP1, patients with gout presented more frequently with synovial hypertrophy (p<0.001), bone erosion (p<0.001), DC signal (p<0.05) and intra-articular aggregates (p<0.05). At the knee, patients showed more often effusion (p<0.001), synovial hypertrophy (p<0.001) and DC signal (p<0.05). At the MCP2, only the presence of erosion was significantly more common in the gout group (p<0.05). DC signal was found in 17 (30%) patients and in none of the healthy subjects (p<0.001); this finding was more frequently observed at the knee. There was an association between previous gout crisis in the MTP1 and the presence of erosion in this joint (p=0.04). Another association was found between the presence of tophi and erosion (p<0.001), DC signal (p<0.05) and intra-articular aggregates (p=0.006). There was no association between uricemia levels, disease duration and US findings.
Comparison between US findings in gout patients and healthy subjects.
| Gout vs controls | Intra-articular effusion | Synovial hypertrophy | Bone erosion | DC signal | Intra-articular aggregates | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| MTF1 | 21 vs 8 | ns | 26 vs 0 | p<0.001 | 19 vs 0 | p<0.001 | 7 vs 0 | p<0.05 | 8 vs 0 | p<0.05 |
| MCF2 | 2 vs 0 | ns | 2 vs 0 | ns | 8 vs 0 | p<0.05 | 4 vs 0 | ns | 6 vs 0 | ns |
| Knee | 19 vs 2 | p=0.004 | 26 vs 1 | p<0.001 | 0 vs 0 | ns | 8 vs 0 | p<0.05 | 3 vs 0 | ns |
In our study, the presence of synovial hypertrophy, erosions, DC signal and intra-articular aggregates were the most frequent US findings in patients with gout. Moreover, we found that the DC signal was significantly more frequent in those with gout, which is in agreement with previous studies.1,7–10 Das et al.10 in 62 patients with gout and 30 control subjects and Stewart et al.1 in 23 patients and 34 normouricaemic subjects concluded that the DC signal was only present in gout patients and in none of the controls. Although we evaluated three joints bilaterally, the knee and the MTP1 seem to be the joints where gout US features are more evident.
Our study has some limitations namely the small size of the sample and the assessments performed by a single observer. Nonetheless, our findings reveal that US seems to be useful in gout to demonstrate evocative signs of crystal accumulation, inflammation or joint damage, even in the absence of flare. Larger studies are needed to confirm our findings.
Conflict of interestThe authors declare that they have no conflicts of interest.