Historically, nutritional therapy for rheumatoid arthritis (RA) has been very appreciated by the medical community. Moreover it has always been a topic of great interest to patients. It follows from this that medical practitioners need information on how best to respond the patients’ questions about what they should be eating in an attempt to control RA.
RA and musculoskeletal disorders are among the most common medical disorders. This disease is characterized by a chronic inflammation of the synovial tissue leading to cartilage and bone damage. Several environmental factors have been recognized as increasing the risk of developing RA and emerging scientific evidence supports the relationship between nutrition and RA. For instance, a consistent prospective, double-blind, and randomized trial found that olive oil supplementation was associated with lower risk of RA.1 Besides, well-designed and meta-analysis studies suggest that patients with RA should consume 3–6g of omega 3 fatty acids (n-3) daily throughout ≥12 weeks. After taking n-3 supplements for this period, patients have reported reduction in joint pain intensity and in non-steroidal anti-inflammatory drugs dose.2,3 Recently, Dawczynski et al4 in a randomized, double-blind, placebo-controlled and cross-over study showed that the effects of dairy products moderately supplemented with n-3 have not improved the RA activity. However, the long-term consumption of dairy products acts against the cartilage and bone destruction in RA.
Concerning other nutrients, a population-based prospective study revealed that the daily intake of one glass of orange juice (containing β-cryptoxanthin, a potent anti-inflammatory component of the diet) is associated with lower risk of developing RA.5 In line with this, other prospective cohort study with more than 29,000 women showed that the high intake of β-cryptoxanthin, zinc supplements and diets rich in fruits and cruciferous vegetables may also be protective against RA.6
Broadly speaking, McCann7 summarized that the nutritional therapy for RA should include anti-inflammatory nutrients (minimum amount of meat and plenty of fish, whole grains, fruits, and vegetables). However, in the same year, Benito-Garcia et al8 in a prospective cohort study with 82,063 women in the Nurses’ Health Study reported that it is still uncertain to confirm that the red meat, poultry, fish, and iron consumption is associated with RA risk. Additionally, Rathore et al9 proposed that Indian herbal medicines, e.g. gingerol—Zinziber officinalis, chirayita—Swertia chirayita, bromelin—Ananas comosus and turmeric—Curcuma longa could act as potent therapeutics agents for RA. Moreover, Kim et al10 demonstrated that other anti-inflammatory components of the diet, particularly polyphenol compounds from green tea—Camellia sinensis including epicatechin, epigallocatechin, epicatechin-3-O-gallate, and epigallocatechin-3-O-gallate,10 have anti-inflammatory properties via the suppression of the pro-inflammatory cytokine IL-17 and of the antibodies to Bhsp65 (a mycobacterial heat shock protein of 65kDa that has been invoked in the pathogenesis of RA) and the increase of the anti-inflammatory cytokine IL-10.
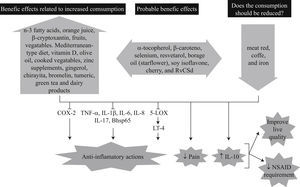
Additionally, further foods, nutrients and nutritional components such as resveratrol, α-tocopherol, β-carotene, selenium, zinc, phosphatidylcholine, Mediterranean-type diet, borage oil (starflower), soy isoflavones, cherry (Prunus avium L), and an oriental herbal mixture called RvCSd (Rv: Rhus verniciflua Stokes, C: Cinnamomum cassia, Sd: Saposhnikovia divaricata) are being studied and may offer possible new targets to prevent and/or treat RA. Fig. 1 summarizes the up-to-date data regarding nutrients and the prevention or treatment of RA, as well as its possible anti-inflammatory mechanisms.
The possible effects of some components of the diet on the prevention and treatment of rheumatoid arthritis. RvCSd: an oriental herbal mixture (Rv: Rhus verniciflua Stokes, C: Cinnamomum cassia, Sd: Saposhnikovia divaricata), LT: leucotriene, PG: prostaglandin, IL: interleukin, TXB: thromboxane, COX: cyclooxygenase, TNF: tumor necrosis factor, LOX: lipoxygenase, NSAID: non-steroidal anti-inflammatory drug.
At the same time we experience the growing knowledge about nutrition and RA, it was not possible for health care providers to acquire all aspects of the combination of the different components of the diet cited above. There is no “RA diet,” for example, the way there are diets for diabetes and cardiovascular diseases. The continuous discoveries represent a challenge for medical providers and scientific investigators, and also contentment for patients who are vulnerable to the misinformation that exists regarding diet and RA. Otherwise, health care providers are in the position of having to simplify much of the information provided by the scientific investigations, not disregarding that dietary supplement should not replace the diet, i.e. the standard nutritional therapy.
FundingThe authors receive a fellowship from the National Council of Technological and Scientific Development (CNPq, Brazil).