Granulomatosis with polyangiitis (GP) is the most frequent ANCA-associated vasculitis, with an annual incidence of 5–14 cases per million inhabitants.1 It predominates in Caucasian adults aged between 45 and 60 and affects both sexes equally.2,3 It is characterised by otorhinolaryngological, pulmonary and renal involvement, positive ANCA findings and confirmation diagnosis through biopsy of the affected organ. We present a case where confirmation diagnosis was made through biopsy of bone marrow.
Clinical ObservationA female aged 51 was admitted to hospital in August 2016 with a respiratory condition, with 3 months onset of fever, cough, changes in chest CT scan (soft tissue density sleeve surrounding the lobar bronchi and proximal segments, millimetric pulmonary nodules), with no microbiological isolation in bronchoalveolar lavage. The patient received 2 cycles of antibiotics with no response to which corticoids were subsequently added and which resulted in improved clinical symptoms. Serous otitis media also presented in the left ear.
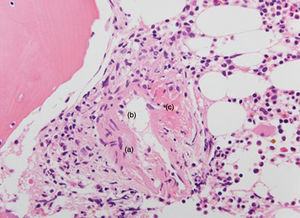
Several days after discharge the patient was readmitted due to fever, non-productive cough, otalgia, deafness, tinnitus in the left ear and dysphonia. On arrival the patient was hypotense, suffered from tachycardia, was eupneic and had a fever of 38.7°C. Cardiopulmonary, abdominal, joint and pulse examinations tested normal. Nasofibroscopy was performed which revealed a mild oedema of the left torus tubarius. Lab analysis showed PCR of 23.76mg/dl, normal procalcitonin, neutrophilia, normocytic anaemia, thrombocytosis up to 1,500,000/μl, 65% prothrombin activity, autoimmunity with negative ANA and ENA, normal complement and c-ANCA 1/20 with antiproteinase-3 antibodies of 32IU/ml (normal values: 0–3IU/ml). Microbiological findings (blood and urine cultures, pharyngeal culture, serology studies, Mantoux) were negative. PET-CT scans showed mucosa enlargement of the nasopharynx, laterocervical and mediastinal adenopathies, a peribronchial soft tissue sleeve and multiple, millimetric pulmonary nodules, a pathological increase of the uptake in medial cortical of the upper pole of the left kidney, all metabolically pathological and suggestive of inflammatory aetiology. The renal study was completed where proteinuria of up to 1.8g/24h was detected, in addition to microhaematuria, dysmophic red blood cells, normal creatine and an abdominal MRI was performed with the renal lesion being suggestive of an inflammatory condition. Due to suspected vasculitis the following biopsies were performed: (a) cervical adenopathy with reactive lymphoid hyperplasia without vasculitis or lymphoproliferative syndrome; (b) nasal mucosa and nasopharynx with chronic inflammation without vasculitis; and (c) biopsy of bone marrow. The bone marrow biopsy showed a lymphoid infiltrate in small vessels, mainly of T lymphocytes (CD3 positive), with images of formation of granulomas with an angiocentric disposition with areas of fibrinoid necrosis. All of the above was compatible with histological diagnosis of granulomatous vasculitis (Fig. 1).
Once we had obtained the histological samples 3500mg boluses of methylprednisone were administered, followed by corticoids at 1mg/kg with improved clinical symptom and the patient was afebrile, with lowering of inflammatory markers.
Following diagnosis of GP with pulmonary, renal and otorhinolaryngological involvement, treatment was initiated with monthly cyclophosphamide. The patient became asymptomatic, with improved laboratory studies and significant reduction of the peribronchial sleeve and pulmonary nodules.
DiscussionGP is a multisystemic disease characterised by otorhinolaryngological symptoms, nodules or pulmonary opacities, glomerulonephritis and other cutaneous, ophthalmological and nervous system symptoms. It is associated in 82%–94% of cases with antiproteinase-3 positivity in c-ANCA patients, although 20% of cases may present with anti-myeloperoxidase.4
In the case which we present a differential diagnosis was performed with the following entities: lympthoproliterative syndrome (ruled out by biopsy), granulomatous infections such as tuberculosis (they present with positive microbacterial cultures), sarcoidosis (the ECA was normal, the ANCA were negative and the biopsy would show non-caseating granulomas), microscopic polyangiitis (usually ANCA-associated positive anti-myeloperoxidase and does not present with granulomas in the biopsy), eosinophilic granulomatosis with polyangiitis (rare in the absence of asthma, eosinophilia or eosinophil infiltrate in the biopsy) and anti-glomerular baseline membrane disease (does not usually present with systemic symptoms nor involvement outside the kidney and lung).
Once all studies had been completed, our patient was diagnosed with GP on meeting the following 1990 ACR classification criteria: inflammation in nasal mucosa, changes in urine sedimentation with microhaematuria and biopsy with proof of granulomatous inflammation.
The suspicion of GP in a patient with compatible clinical symptoms and positive ANCA must be confirmed when possible with biopsy, although when the situation is severe treatment should not be delayed. The most favourable biopsy location for diagnosis is the kidney although cuteaneous, pulmonary or nasal biopsies may also be useful. Nasal biopsies, however, may result in a high rate of false negatives.
Other locations where biopsy has confirmed diagnosis of GP are less common. Infrequent cases have been described which began in a similar manner to gastric ulcer or gastric cancer but in which necrotising granulomas were detected suggestive of GP.5–8 Granulomatous vasculitis has also been detected in biopsies of the breast in patients with an initial suspicion of neoplasia,9 and in biopsies of ulcers in foreskin and glans.10,11 With reference to bone marrow, samples have been reported in GP with haemophagocytosis12 or lymphoproliferative syndrome,13 but to our knowledge the detection of granulomatous vasculitis in bone marrow has not been previously described. It is probable that the presence of macrophages and the extended vascularisation of the bone marrow confirm the presence of granulomatous vasculitis in this location.
ConclusionAs GP is a systemic vasculitis, involvement may occur in any organ and infrequent locations for GP have been described in which biopsy has revealed granulomatous vasculitis. Notwithstanding, its detection in bone marrow up until now has not been reported.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of InterestsThe authors declare they have not received any financing and there are no conflicts of interests.
Please cite this article as: de la Cámara Fernández I, Lozano Morillo F, Morillas López L, Martínez López M. Comunicación de un caso de granulomatosis con poliangitis con detección de granulomas en médula ósea. Reumatol Clin. 2019;15:e60–e61.