Fluoroquinolones have been associated with increased risk of tendinopathy and Achilles tendon rupture (ATR), especially in patients over 60 years of age.
MethodsA retrospective study was carried out including patients over 60 years of age with ATR attended in our centre over the period 2000–2017.
ResultsWe identified 44 patients with RTA, of whom 18% (8/44) had been previously treated with fluoroquinolones, with a mean age at diagnosis of ATR of 77.37 years and concomitant corticotherapy in 4 of them. In 7 patients, the rupture was spontaneous and all required surgical management. A significantly higher frequency of smoking, concomitant corticotherapy and spontaneous ruptures were found in the group treated with fluoroquinolones.
ConclusionsATR is an adverse event that can occur in patients over 60 years of age treated with fluoroquinolones, so an adequate risk-benefit assessment should be carried out in this population, especially in the presence of associated risk factors.
Las fluoroquinolonas han sido asociadas con aumento del riesgo de tendinopatía y rotura del tendón de Aquiles (RTA), especialmente en pacientes mayores de 60 años.
MétodosSe llevó a cabo un estudio retrospectivo en el que se incluyó a los pacientes mayores de 60 años con RTA atendidos en nuestro centro durante el período 2000-2017.
ResultadosSe identificó a 44 pacientes con RTA, de los cuales 18% 8/44 habían sido tratados previamente con fluoroquinolonas, con una media de edad al diagnóstico de RTA de 77,37 años y corticoterapia concomitante en 4 de ellos. En 7 pacientes la rotura fue espontánea y todas requirieron tratamiento quirúrgico. Se encontró una frecuencia significativamente mayor de tabaquismo, corticoterapia concomitante y roturas espontáneas en el grupo tratado con fluoroquinolonas.
ConclusionesLa RTA es un evento adverso que puede ocurrir en pacientes mayores de 60 años tratados con fluoroquinolonas, por lo que debería realizarse una adecuada evaluación relación riesgo-beneficio en esta población, especialmente en presencia de factores de riesgo asociados.
The Fluoroquinolones (FQ) are a group of broad-spectrum antibiotics, which have come into wider use due to their efficacy and suitable tolerability and safety profile. However, pharmacovigilance studies have associated the use of these drugs with adverse events in connection with alterations in the extracellular matrix collagen. Tendinopathy and tendon rupture have been reported, as well as retinal detachment and aortic aneurisms.1 Although the exact mechanism is unknown, the FQ may cause direct damage to cells in the connective tissue of the tendon, including alterations of fibroblast metabolism and phenomena of necrosis and apoptosis, as well as indirect damage due to the release of metalloproteases, nitric oxide and reactive forms of oxygen.2–4
The Achilles tendon is the most frequent location of tendinopathy associated with FQ, and it is affected in up to 95% of cases. Although the risk of Achilles tendon rupture (ATR) associated with FQ is rare in a healthy young population, it triples in patients older than 60 years old or in the presence of other risk factors.5 The aim of our study is to describe the epidemiological and clinical profile of patients diagnosed ATR after being treated with FQ, seen in a tertiary Madrid hospital.
Patients and methodsA retrospective, observational and transversal study was performed, including patients diagnosed ATR (confirmed by imaging tests or surgical examination) and seen in our hospital in the period from 2000–2017. The clinical histories of the included patients were reviewed, obtaining their demographic data (age, sex, comorbidities and toxic habits) together with information on concomitant medication (glucocorticoids and statins), the mechanism that cause the rupture (spontaneous or traumatic), the type of rupture (partial or total), treatment and evolution of the same. Likewise, those patients who had received treatment with FQ prior to the ATR were identified, registering in these cases the time that transpired from starting to take FQ until the ATR, the type of FQ used, the duration of and the indication for the said treatment.
The demographic and clinical variables were compared between the patients with and without previous treatment with FQ, using the χ2 and Mann–Whitney U tests to obtain the P value. A P value < .05 was considered to indicate statistical significance.
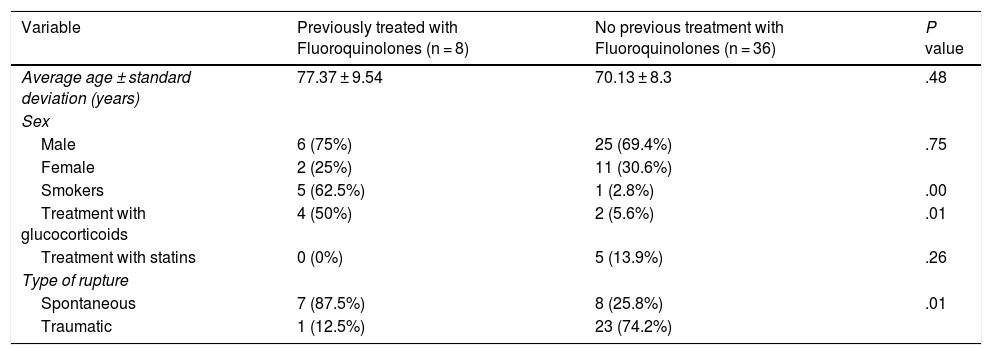
ResultsDuring the period studied a total of 44 patients with ATR were identified (Table 1), of whom 18% (8/44) had been treated previously with FQ. In this latter group the average age at diagnosis of ATR was 77.37 ± 9.54 years old, and 6 of them were men (75%). In 4 cases there was a history of chronic treatment with concomitant glucocorticoids, although none of them had received statins when the ATR occurred. Regarding relevant comorbidities, 3 patients had previously been diagnosed with chronic obstructive pulmonary disease (COPD), one had recently been diagnosed with diffuse interstitial pulmonary disease (DIPD) and another patient had been subjected to renal transplant due to chronic terminal kidney disease secondary to nephroangioesclerosis.
Comparison of the characteristics of patients with ATR, with and without previous treatment with FQ.
| Variable | Previously treated with Fluoroquinolones (n = 8) | No previous treatment with Fluoroquinolones (n = 36) | P value |
|---|---|---|---|
| Average age ± standard deviation (years) | 77.37 ± 9.54 | 70.13 ± 8.3 | .48 |
| Sex | |||
| Male | 6 (75%) | 25 (69.4%) | .75 |
| Female | 2 (25%) | 11 (30.6%) | |
| Smokers | 5 (62.5%) | 1 (2.8%) | .00 |
| Treatment with glucocorticoids | 4 (50%) | 2 (5.6%) | .01 |
| Treatment with statins | 0 (0%) | 5 (13.9%) | .26 |
| Type of rupture | |||
| Spontaneous | 7 (87.5%) | 8 (25.8%) | .01 |
| Traumatic | 1 (12.5%) | 23 (74.2%) | |
Seven patients (87.5%) had been treated with levofloxacin and one with ciprofloxacin, all of them administered orally. In half of the cases the indication for treatment with FQ was acute bronchitis, while in the others it was for infectious exacerbations of their underlying respiratory disease (COPD/DIPD). The average duration of treatment with FQ was 6.16 ± 2.4 days, while the average time from starting to take this drug and the diagnosis of ATR was 19.25 ± 14.83 days. In 7 cases the rupture was spontaneous, while in one patient it was associated with low-intensity traumatism. The ATR was complete in 7 cases, and all of them required surgical repair (including the single case of partial rupture), without any subsequent recurrence.
When the characteristics of the patients with ATR who had been treated with FQ are compared with those who had not, significant differences are found respecting a history of smoking (62.5% vs. 2.8%; P = .00), concomitant treatment with glucocorticoids (50% vs. 5.6%; P = .01) and spontaneous rupture (87.5% vs. 25.8%; P = .01) in the FQ group FQ (Table 1).
Discussion and conclusionsBased on previous population studies, it is estimated that patients under treatment with FQ are at 1.6–1.7 times more risk of tendinopathy than the general population, and the Achilles tendon is the most frequent location (rate of incidence adjusted for ATR 3.14).5,6 In the published cases and series of cases, the time from starting treatment with FQ until the appearance of ATR varies, with a median time of 6 days,7 although it has even been described as occurring from a few hours after starting to take the drug until 6 months after it had been withdrawn.8 The risk of developing ATR is 3 times greater in the first 90 days after starting treatment with FQ.9 In our series, the average time from starting to take the drug until the diagnosis of ATR was 19 days, and this is similar to the 16 day period found in the case-control by Corrao et al. in a Northern Italian population.5
The risk factors that have been associated with developing ATR during treatment with FQ include being older than 60 years old, male, chronic treatment with glucocorticoids, chronic kidney disease and organ transplant (kidney, lung or heart).10 Although the design of our study makes it impossible to establish causal relationships between the use of FQ and other risk factors and the development of ATR, or the possibility that the effect of FQ amplifies other possible risk factors, such as glucocorticoids or smoking, similar associations to those found in previous studies were observed. In our series, there were significantly more men in the group treated with FQ, and up to half of the cases received concomitant glucocorticoid treatment. This percentage is higher than those described in other series, in which the rate of treatment with these drugs ran from 15% to 20%.5,11 This is probably related to our higher number of patients with underlying respiratory disease and chronic inhaled or systemic corticoid therapy. Although organ transplant is a factor clearly associated with FQ connected ATR, only one case in our series had received a kidney transplant, and this type of transplant is the one for which this adverse event has been described the most often (incidence in the population who have received a kidney transplant: 12.2%–15,6%).12 Statins have also been associated with the development of tendinopathy, and it has been argued that their concomitant use with FQ may amplify this risk.13 However, none of the cases in our series had received both drugs simultaneously, and the study of nested cases and controls in a British population by Morales et al. found no correlation between the concomitant use of statins and the development of ATR associated with FQ.6 Other variables associated with the appearance of tendinopathy, the risk of which may increase with the use of FQ but which were not studied in our population are obesity, diabetes mellitus, dyslipidemia, hyperparathyroidism and underlying musculoskeletal disorders.5,12,14 On the other hand, we found a higher number of smokers among the patients who had received FQ, and this datum agrees with previous studies in which being a current smoker (but not an ex-smoker) is associated with an increase in ATR linked to these drugs.6
Although Seeger et al. found no difference in the risk of developing ATR associated with FQ when they compared different drugs in this family in a study of a North American population that included 947 cases of ATR and 18,940 controls,14 other studies, such as those by van der Linden et al.11 and Hori et al.15 found a higher risk of ATR in patients who had taken ofloxacin in comparison with other types of FQ, and that this association was dose-dependent. Nevertheless, in the literature as well as in our series, the majority of cases occurred in patients treated with ciprofloxacin,7 and in more recent publications those treated with levofloxacin.8 This is probably due to the increasingly widespread use of the latter medication.2
FQ are usually prescribed to treat infections that affect the respiratory, genitourinary and gastrointestinal tracts, the first of which was the main cause of the indication for treatment with these drugs in our series. However, other alternative antibiotic treatments exist, and these could be considered for individuals at high risk of ATR, as this condition usually requires surgical treatment. This was evident in our study, in which surgery was necessary in 100% of the cases to repair the rupture, and this may be associated with a high level of morbidity and functional disability. It is therefore advisable to identify the presence of the said risk factors and ensure the early detection of tendinopathy symptoms in these patients.
To conclude, the description of our series supports the emerging concern expressed by pharmacovigilance systems respecting adverse musculoskeletal reaction to the use of FQ, more specifically in terms of tendinopathy and ATR. An appropriate risk-benefit analysis should therefore be performed prior to using these drugs in patients over the age of 60 years old with concomitant risk factors, excluding them for cases of mild or self-limiting infections or when other alternative treatments are available.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Briones-Figueroa A, Sifuentes-Giraldo WA, Morell-Hita JL, Vázquez-Díaz M. Rotura del tendón de Aquiles asociada al uso de fluoroquinolonas en pacientes mayores de 60 años: experiencia de un centro de tercer nivel. Reumatol Clin. 2021;17:141–143.