Systemic sclerosis is a rare disease that predominantly affects women. The Medsger severity scale has been used to assess the severity, but it requires expensive and poorly accessible studies and it does not include complications such acrosteolysis, calcinosis, pericardial disease or hypothyroidism that occur on a relatively frequent basis in this disease. There is no study that considers if comorbidities, such as primary biliary cirrhosis, are related to gravity.
ObjectivesTo determine the correlation between severity and the presence of such complications.
Methods40 patients with systemic sclerosis, dividing them into tertiles according to severity were studied. Dichotomous variables were described using percentages, while dimensional by averages+SD. Statistical inference was performed using chi square test or Kruskal–Wallis test with Dunn post-test, as appropriate. A significance at P<.05 was set.
ResultsOf all the complications studied there were only differences in severity with acrosteolysis. Within comorbidities, primary biliary cirrhosis is not associated with gravity.
La esclerosis sistémica es una patología rara que afecta predominantemente a las mujeres. Se utiliza la escala de Medsger para evaluar la severidad, pero precisa de estudios caros y de difícil acceso y no incluye complicaciones tales como acrosteólisis, calcinosis, enfermedades pericárdicas o hipotiroidismo, que se presentan con relativa frecuencia en esta enfermedad. No existen estudios que tengan en cuenta si las comorbilidades, como la cirrosis biliar primaria, se asocian a la gravedad.
ObjetivosEstablecer la correlación entre la gravedad y la presencia de complicaciones asociadas.
MétodosSe estudió a 40 pacientes con esclerosis sistémica, divididos entre terciles conforme a su gravedad. Se describen las variables dicotómicas con porcentajes, mientras que las variables dimensionales se describen con medias+DE. La interferencia estadística se llevó a cabo con la prueba de la χ2 y de Kruskal–Wallis con la prueba de Dunn después del test, según procediera. Se estableció la significación estadística en p<0,05.
ResultadosDe todas las complicaciones analizadas, solo había diferencias en el caso de la acrosteólisis. Entre las comorbilidades, la cirrosis biliar primaria no se asocia a la gravedad.
Systemic sclerosis (SS) is an uncommon disease (the worldwide prevalence is 10–34.1 per 100,000 population), of unknown etiology, with a clear female predominance. The systemic forms are divided into 2 large groups, limited (LSS) and diffuse (DSS). The factors that interact in the pathogenesis are autoimmunity, inflammation and functional and structural changes in the small vessels, as well as interstitial and vascular fibrosis of the skin and internal organs, and collagen deposition in the extracellular matrix. The prognosis varies depending on the extent of the skin compromise, the degree of involvement of internal organs and the comorbidities.1
To date, it has been very difficult to build a consensus with regard to a practical and economical way to evaluate the extent of the damage in an individual in the outpatient setting. One of the tools most widely validated and employed in some clinical studies is the Medsger Disease Severity Scale (MDSS).2 This scale does not take into consideration some of the complications of SS, such as acro-osteolysis.
Acro-osteolysis is the erosion of the distal phalanges, affecting those of the hands in 22% of the patients.3 It starts at the tip and, in the most severe cases, produces the destruction of a large portion of the distal phalanx, giving the finger a conical aspect.4 Its clinical importance, according to some authors,5 is its association with digital ulcers, severe Raynaud's phenomenon and calcinosis.
Main ObjectiveWe propose to determine whether acro-osteolysis is related to the severity of SS in accordance with the MDSS.
Material and MethodsStudy DesignA cross-sectional, observational, quasi-experimental analysis was performed.
Description of the Study PopulationInclusion CriteriaWe considered eligible any patient over 18 years of age who met the updated criteria of the American College of Rheumatology for SS, was being followed during the current year in the Department of Rheumatology of the Mexican National Institute of Cardiology, had a complete record for the determination of the MDSS, and had undergone capillaroscopy within the past year. This required:
- 1.
At least one indirect immunofluorescence assay, at the time of diagnosis, for antinuclear antibodies (ANA), as well as ANA specificities determined by enzyme-linked immunosorbent assay (ELISA): anti-centromere and anti-topoisomerase I.
- 2.
At least 2 clinical evaluations within the last year.
- 3.
Examination within the preceding 2 years including: body weight and/or hematocrit; the presence of Raynaud's phenomenon and its severity; the presence of digital ulcers or digital gangrene; measurement of the finger-to-palm distance; evaluation of the presence or absence of muscle weakness and its degree, and the presence or absence of symptoms of esophageal or bowel dysfunction and the consequences; spirometry with determination of the diffusing capacity of the lungs for carbon monoxide (DLCO) and measurement of the forced vital capacity (FVC); evaluation of the presence or absence of pulmonary infiltrates on radiographs, and the presence or absence of pulmonary hypertension (PH) and, if present, its severity or whether or not continuous oxygen is required; electrocardiogram evaluated by an expert (cardiologist) to establish the presence or absence of arrhythmias, ventricular enlargement or heart failure; at least 1 transthoracic echocardiogram (TTE) to corroborate structural anomalies and left ventricular ejection fraction (LVEF), as well as calculated pulmonary artery systolic pressure (PASP); and creatinine determination and measurement of proteinuria, if detected.
In addition to the analysis of these data, a radiological examination was performed to determine the presence or absence of acro-osteolysis.
Exclusion CriteriaWe excluded patients in whom the diagnosis was not clearly established, who had any syndromes that overlapped or mixed connective tissue disease that had the features of SS, who had been lost to follow-up in the past year, or for whom the data (referring to any of the abovementioned variables) were not complete.
Definition of the VariablesAll of the patients who had been diagnosed with PH had at least 2 of 3 studies that, while not confirmatory, created a high degree of suspicion as they indicated the presence of the disease: (a) a radiograph with thickening of the pulmonary artery associated with “pruning” of peripheral blood vessels (present in 90% of those affected, according to the literature) and/or (b) a TTE performed within the preceding 2 years showing tricuspid regurgitation with a pressure gradient >40mmHg (tricuspid regurgitation velocity >3.2m/s), with an assumed right atrial pressure of 10mmHg (thus equivalent to a pulmonary artery systolic pressure > 50mmHg),6 and/or complete spirometry that included FVC and DLCO; the latter is usually between 40% and 80% of the predicted value in affected patients.7
We took into account all the variables proposed by Medsger for the evaluation of severity, in accordance with the definitions he and his collaborators had previously established, which were revised by the same group in 2003.8 However, we wish to make the following points.
To determine the distance from pulp to palm in flexion, we took into account the worst score obtained in the most severely affected hand, in the absence of burns, Dupuytren's contracture or any other condition of the palm that could jeopardize this parameter.
With respect to the gastrointestinal evaluation, a change was considered to be present only if there was an imaging study that supported the clinical suspicion (upper gastrointestinal series in the case of esophageal or duodenal disease and/or endoscopy, tomography in the case of intestinal involvement or evidence of blind loop syndrome observed in special coprological examinations).
In the section on lung, to achieve the final score, we considered the worse parameter evaluated, given that DLCO, FVC, PASP and radiographic changes are grouped together in each section. The identification of interstitial lung disease (ILD) was based not only on changes in those parameters, but on the presence of characteristic pulmonary infiltrates on high-resolution tomography with or without the presence of fine crepitant rales on auscultation. The same was carried out in the section on the heart, in which the final score was defined by the worst parameter (changes on the electrocardiogram or TTE showing an abnormal LVEF).
Any change in the pericardium reported in TTE was considered to be a pericardial disease, once it had been evaluated by an expert in echocardiography. Pericardial effusion was classified according to Maisch et al.9
Although the MDSS was not designed to sum up the points in the section corresponding to each organ, we performed this addition to facilitate the statistical analysis.
Statistical StudyThe dichotomous variables were expressed as percentages, whereas the dimensional variables were expressed as mean±standard deviation (SD).
Statistical inference was based on chi-square tests, with adjustment for trends when possible, or the Kruskal–Wallis test with Dunn's post hoc test, as appropriate.
The results were divided into tertiles to improve the statistical calculation.
All of the analyses were two-tailed and significance was set at P<.05.
The statistical software package used was GraphPad Prism (version 4.02) (GraphPad Inc., San Diego, United States).
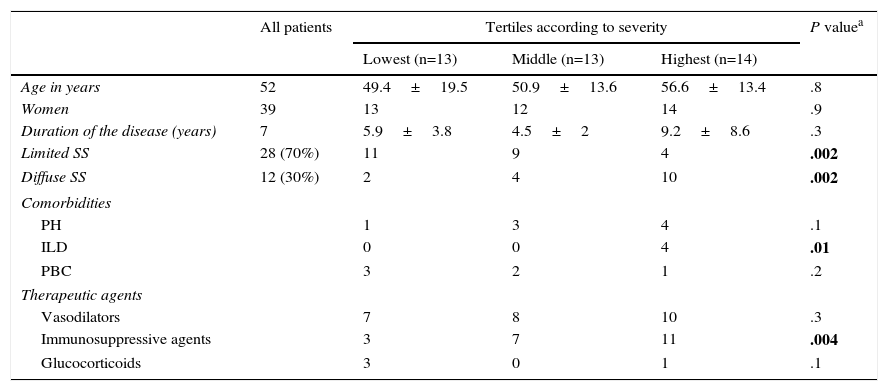
ResultsWe studied a total of 40 patients who met the inclusion criteria. The mean age of the study population was 52 years, with a range of 13–77 years.
Regarding the duration of the disease course, the count began from the first year of diagnosis, even if this had not taken place in the institute, and continued once the patient had been enrolled in the study, in the department of rheumatology. As was to be expected, the patients with the longest history of disease had LSS, although there was not much difference with respect to DSS.
The immense majority of the patients (39) were women and of the total group, 27 (70%) had LSS.
In all, 18.6% of the patients with LSS had been diagnosed with PH (without specifying the group), the same incidence as pericardial effusion. Less common was ILD, with a prevalence of 3.7%. In DSS, the most common comorbidity was PH (29%), followed by ILD. Of all these conditions, only ILD had a statistically significant influence on the disease severity (see Table 1).
Demographic and Clinical Data Related to the Medsger Disease Severity Scale.
| All patients | Tertiles according to severity | P valuea | |||
|---|---|---|---|---|---|
| Lowest (n=13) | Middle (n=13) | Highest (n=14) | |||
| Age in years | 52 | 49.4±19.5 | 50.9±13.6 | 56.6±13.4 | .8 |
| Women | 39 | 13 | 12 | 14 | .9 |
| Duration of the disease (years) | 7 | 5.9±3.8 | 4.5±2 | 9.2±8.6 | .3 |
| Limited SS | 28 (70%) | 11 | 9 | 4 | .002 |
| Diffuse SS | 12 (30%) | 2 | 4 | 10 | .002 |
| Comorbidities | |||||
| PH | 1 | 3 | 4 | .1 | |
| ILD | 0 | 0 | 4 | .01 | |
| PBC | 3 | 2 | 1 | .2 | |
| Therapeutic agents | |||||
| Vasodilators | 7 | 8 | 10 | .3 | |
| Immunosuppressive agents | 3 | 7 | 11 | .004 | |
| Glucocorticoids | 3 | 0 | 1 | .1 | |
ILD, interstitial lung disease; PBC, primary biliary cirrhosis; PH, pulmonary hypertension.
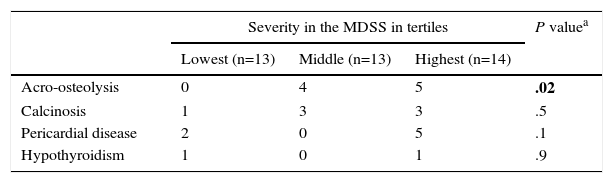
Acro-osteolysis also showed a statistically significant difference in relation to severity (see Table 2).
Selected Clinical Manifestations not Considered in the Medsger Disease Severity Scale (MDSS).
| Severity in the MDSS in tertiles | P valuea | |||
|---|---|---|---|---|
| Lowest (n=13) | Middle (n=13) | Highest (n=14) | ||
| Acro-osteolysis | 0 | 4 | 5 | .02 |
| Calcinosis | 1 | 3 | 3 | .5 |
| Pericardial disease | 2 | 0 | 5 | .1 |
| Hypothyroidism | 1 | 0 | 1 | .9 |
By far, a large part of the literature on SS is based on the observations of physicians from other countries in which Caucasians usually predominate and, to a lesser degree, Afro-Americans. The most widely known groups studying this disease are from the United Kingdom, The Netherlands, Italy and, to a lesser extent, North America. In contrast, it has been studied very little in Latin American countries, where there is a predominance of mestizos and, to a lesser extent, indigenous populations. A recent study published in Science shows how important the differences in the Mexican population can be with respect to the behavior of different diseases.10
With regard to the prevalence of ILD in SS, most of the literature reports a rate of 8%–12%, although it is usually milder in the diffuse forms, especially if it is associated with anti-centromere B.10,11 In the present study, we found it in only 3.7% of the patients. It was not very different in the patients with DSS, in whom a prevalence of 50%–80% has been reported in referral centers,12 whereas in this analysis, the prevalence scarcely reached 20% in that group of patients. However, these results should be taken with caution, given that many patients without respiratory symptoms may have been overlooked because they had not undergone high-resolution tomography.
In a cohort of patients studied for ILD, with the usual type of interstitial pneumonia, Fischer et al.13 found that SS was the underlying disease in 8.7% of the overall cohort. In an observational study of the treatment of ILD in SS, the most extensive published to date, Iudici et al.14 found it to be much more common in DSS, and especially those patients who were positive for Scl were less likely to respond to treatment with cyclophosphamide and more likely to have more severe pulmonary compromise.
With respect to PH, there are many discrepancies in the literature, having to do with the year of publication and the changes that have taken place in the diagnostic criteria. It is known that, in general, it is more widespread among patients with LSS, in whom it can come to be highly aggressive, and it usually belongs to group 1 of the Dana Point 2008 classification (true pulmonary arterial hypertension). The literature mentions an estimated prevalence in asymptomatic patients of 8%–14%,12,15,16 whereas in the population of the Mexican National Institute of Cardiology, it was slightly more common (18.5%) in the limited forms, being even more frequent in the diffuse forms (29%). In these patients, a lower prevalence has characteristically been reported, and they usually develop this complication as a consequence of left heart disease (group 2) or secondary to restrictive lung disease (group 3).17,18 In this respect, it is important to take into consideration the fact that several patients had not undergone right cardiac catheterization to confirm the diagnosis, which was based only on the TTE findings and clinical signs.
While the literature indicates that acro-osteolysis is associated with a greater number of vascular complications, its association with disease severity is not clearly established. In our study, we confirm that there is a difference between the patients with mild and severe forms in terms of its frequency.5
ConclusionsSystemic sclerosis is an uncommon disease, of unknown etiology, about which we still have much to learn. It is still necessary to devise methods of evaluation much more widely available in clinical practice, that enable us to establish the severity of the disease with much simpler resources and, thus, to perform a proper stratification for patient follow-up. Acro-osteolysis is a clinical complication that is not considered in the MDSS, but is directly related to the severity. Should this be corroborated in future studies, this parameter could replace other complications that require complex and expensive measures for their evaluation.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Arana-Ruiz JC, Amezcua-Guerra LM. La acrosteólisis como indicador de gravedad en los pacientes con esclerosis sistémica. Reumatol Clin. 2016;12:263–266.