Patients with RA have a two to four-fold increased risk of developing infections compared to the general population. For this reason, the administration of influenza, pneumococcal and shingles vaccines is recommended for all patients with RA, preferably prior to initiating treatment,
Previous studies have demonstrated the low prevalence of vaccination as well as adherence to current recommendations by rheumatologists in other regions.
ObjectiveTo determine the knowledge and adherence to the current vaccination recommendations for patients with RA by rheumatology members of the Mexican College of Rheumatology (MCR), and to identify barriers to their application in this population.
MethodsA cross-sectional study was conducted through a survey sent to 577 rheumatologists from Mexico in January 2017.
ResultsWe received completed surveys from 122 individuals, representing 21.14% of the 577 rheumatologists in our registry. Fifty percent responded that they recommended immunisation against influenza to 76%–100% of their patients, 36.07% recommended immunisation against pneumococcus to 76%–100% of their patients, and 69.67% of the survey responders did not recommend shingles immunisation routinely to their patients.
ConclusionsThe data collected in this study show there is poor adherence to immunisation schedules recommended for the RA population. This data suggests there is misinformation about the effectiveness, safety and optimal timing of immunisation in patients with RA in Mexico.
Los pacientes con artritis reumatoide (AR) presentan un incremento de dos a cuatro veces del riesgo de infecciones comparado con la población general. Por esta razón, existen recomendaciones sobre la aplicación de vacunas de influenza, neumococo y herpes zóster en todos los pacientes con AR, previo al inicio del tratamiento.
Varios estudios han demostrado la baja prevalencia de vacunación así como la adherencia a las recomendaciones actuales de inmunización por los reumatólogos.
ObjetivoEl objetivo de este estudio fue determinar el conocimiento de las recomendaciones actuales de inmunización en pacientes con AR por los reumatólogos miembros del Colegio Mexicano de Reumatología (CMR), así como identificar las barreras en su aplicación en dicha población.
MétodosSe realizó un estudio transversal por medio de una encuesta a 577 reumatólogos de México en enero 2017.
ResultadosSe obtuvieron 122 respuestas, representando el 21,14% de los 577 reumatólogos.
El 50,82% respondió que recomendaba al 76%–100% de sus pacientes la vacuna de influenza, el 36,07% recomendaba al 76%–100% de sus pacientes la vacuna de neumococo y con respecto a la vacuna del herpes zóster el 69,67% respondió que no la recomendaba rutinariamente a sus pacientes.
ConclusionesDe acuerdo a los datos obtenidos en este estudio, no existe información adecuada acerca de la importancia de la vacunación en pacientes con AR. También muestra que el grado de adherencia a las recomendaciones de vacunación así como el conocimiento sobre seguridad y tiempo óptimo de administración de las vacunas son bajos en México.
Patients with rheumatoid arthritis (RA) are estimated to have from 2 to 4 times the risk of infection compared to the general population.1,2 This may arise due to the immunological dysfunction that the disease involves, associated comorbidities and/or immunosuppressant treatment, and it contributes notably to the morbimortality of these patients.2,3
This is why there are recommendations that patients with RA be actively immunised to prevent infectious diseases.
In general patients with RA are recommended to vaccinate against influenza, pneumococcus and herpes zoster in patients who are above 50 years old, ideally before starting treatment. The recommendations for vaccination against human papilloma are the same as those for the general population, and vaccination against hepatitis B should be given before any treatment if the patient has risk factors for contracting this disease.4–6
In the case of vaccination against herpes zoster, it is important to consider that as it is an attenuated live virus it is contraindicated during strong immunosuppressant treatment,7 so that it should preferentially be administered 4 weeks prior to starting this form of treatment.4,8
Respecting its safety, Zhang et al. conclude in their study that herpes zoster vaccine is not associated with an increase in the risk of infection, and that it reduced the incidence of this over an average of 2 years follow-up.9
ObjectiveTo determine the degree of adherence to current vaccination recommendations in patients with RA by rheumatologists who are members of the Colegio Mexicano de Reumatología (CMR) and to identify the barriers against applying immunisation recommendations.
Material and methodsA transversal study was carried out by means of a survey (Table 1) sent by email to 577 Mexican rheumatologists registered in the CMR database in the month of January 2017. The survey was sent out on 3 occasions. On the first occasion an invitation to respond to the survey using a link to the SurveyMonkey page was sent. The survey was confidential and consisted of 9 multiple choice questions. Two weeks later a reminder was sent out to the doctors who had not answered, and 2 weeks later a third and final invitation to respond to the survey was sent.
Survey.
| 1. Where do you work in the majority of your medical practice? | a) Private sector |
| b) Public sector | |
| c) Mixed | |
| 2. Do you consider that updating vaccination schedules for adult rheumatology patients is the responsibility of: | The family doctor /general practitioner |
| a) The internal medicine doctor | |
| b) The rheumatologist | |
| 3. Do you include vaccination records in clinical files? | a) Yes |
| b) No | |
| 4. Please say why you do not routinely recommend immunisation to your patients: | a) Lack of time when they consult |
| b) I give priority to other aspects when they consult | |
| c) I only do not recommend this when there are contraindications | |
| 5. In what percentage would you routinely recommend vaccination against influenza in your rheumatoid arthritis patients? | a) 0%–25% |
| b) 26%–50% | |
| c) 51%–75% | |
| d) 76%–100% | |
| 6. In what percentage would you routinely recommend vaccination against pneumococcus in your rheumatoid arthritis patients? | a) 0%–25% |
| b) 26%–50% | |
| c) 51%–75% | |
| d) 76%–100% | |
| 7. If you recommend vaccination against influenza or pneumococcus in your patients, when do you indicate or administer this? | a) Before starting treatment with a conventional DMARD |
| b) Only before starting treatment with a biological agent or tofacitinib | |
| c) I recommend it without distinguishing (before or during treatment with a conventional DMARD, a biological agent or tofacitinib) | |
| d) I do not do so routinely | |
| 8. Do you recommend vaccination against herpes zoster to your rheumatoid arthritis patients? | a) Not routinely |
| b) Before or during treatment with a conventional DMARD | |
| c) Only before starting treatment with a biological agent or tofacitinib | |
| 9. What do you think is the main reason why your patients with rheumatoid arthritis do not accept vaccination? | a) Fear of possible adverse effects |
| b) Lack of information in general | |
| c) Cost |
The questions in the survey had the purpose of evaluating adherence to current recommendations for vaccination in RA and the clinical practice of rheumatologists in connection with them.
Inclusion criteriaAll of the rheumatologists registered in the CMR database were included.
Exclusion criteriaDoctors who for any reason did not respond to the survey or could not be contacted by email.
Results122 replies to the survey were obtained from rheumatologists who are members of the CMR of the total of 577 which were sent, representing 21.14% of the sample. 38.2% worked exclusively in the private sector, 19.67% (24/122) stated that they work exclusively in the public sector, and 41.8% (51/122) declared that they work in the public and private sectors.
14.05% (17) respondents stated that updating vaccination schedules in adult rheumatology patients is the responsibility of the family doctor or general practitioner. 4.96% (6) answered that this is the responsibility of the internal medicine specialist, and 80.99% (98) answered that it is the responsibility of the rheumatologist. One respondent did not answer this question.
43.44% (53) stated that they did not include vaccination records in the clinical file and 56.56% (69) replied that they did. Of the 24 doctors who work exclusively in the public sector, 41.66% (10) reported that they did include vaccination history, and in the private sector 48.93% (23) of the 47 doctors who answered said that they did.
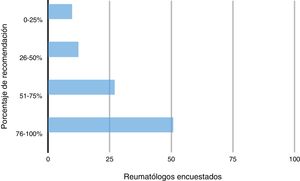
In the case of influenza vaccination in patients with RA in the surgery, 9.84% (12) responded that they had recommended this to 0%–25% of their patients and 12.3% (15) had recommended it to 26%–50% of their patients; 27.05% (33) had recommended it to 51%–75% of their patients and 50.82% (62) had recommended it to 76%–100% of their patients (Fig. 1).
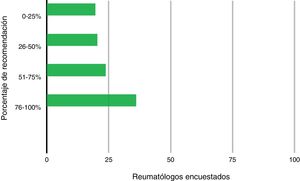
19.67% (24) of the doctors had recommended vaccination against pneumococcus to 0%–25% of their patients, 20.49% (25) had done so to 26%–50%, 23.77% (29) had recommended it to 51%–75% and 36.07%(44) had recommended it to 76%–100% of their patients (Fig. 2).
Regarding when influenza and/or pneumococcus vaccine was administered, 13.11% (16) of the doctors answered that they administered it before commencing treatment with disease modifying drugs (DMARD). 22.13% (27) responded that they only administered these vaccines before starting treatment with biological agents or tofacitinib. 54.1% (66) responded that they administered them without distinguishing, i.e., either before or during treatment with a DMARD, biological agent or tofacitinib, and 10.66% (13) responded that they did not administer these vaccines routinely.
Regarding herpes zoster vaccination, 69.67% (85) doctors answered that they did not usually recommend this to their patients. Only 6.56% (8) responded that they recommended this before or during conventional DMARD treatment, and 23.77% (29) answered that they only recommended it prior to starting treatment with a biological agent or tofacitinib.
Regarding the reasons given by the rheumatologists who did not usually recommend vaccination for this, 75.86% (88) answered that they did not do so only in cases when it was contraindicated, 20.69% (24) stated that they did not do so because they gave priority to other aspects when patients consulted, and 3.45% (4) responded that they did not do so due to lack of time when patients consulted. 4.91% (6) of the respondents did not answer this question.
Lastly, the rheumatologists surveyed were asked what they thought was the main reason why their RA patients did not accept vaccination; 33.33% (40) responded that it was due to fear of possible adverse effects, 52.5% (63) answered that it was because of a lack of information in general, and 14.17% (17) responded that it was because of the cost of the vaccine. Two of the respondents did not answer this question.
DiscussionThe clinical practice guide for the vaccination of immunocompromised patients, issued by the Infectious Diseases Society of America in 2013, states that vaccinating these patients is the responsibility of the specialist in charge of managing them, in this case the rheumatologist, as well as of primary care doctors. They all have to ensure that vaccines are administered appropriately to patients as well as to those who share their household.8
Previous studies in Ireland, the United Kingdom and Germany show that there is a low rate of immunisation and adherence to the recommendations for immunisation.10–12
In an international study (COMORA) in 2014 Dougados et al. evaluated the prevalence of comorbidities and how they were monitored in patients with RA in 17 countries over 5 continents. This study found that 938 (25.3%) of the patients had been vaccinated against influenza, while over the previous 5 years 636 patients had been vaccinated against pneumococcus, i.e., 17.2% of the population analysed. The patients who were up-to-date with both vaccines according to recommendations amounted to only 10.3% of the population.13
In the COMORA study the factors that influenced the vaccination of individuals in the countries with the highest rates of vaccination were advanced age, low disease activity, a high educational level, treatment with biological agents, the absence of treatment with glucocorticoids and the presence of comorbidities.14
In the particular case of herpes zoster vaccination Perry et al. found in an observational study that of 19,326 patients with RA over 50 years old, only 206 (1%) had received the vaccine. On the other hand, in the cohort of Medicare recipients only 3.3% of the patients with RA over 60 years of age were found to have been vaccinated.15
No studies have been undertaken in our country to date which show the current situation in this respect.
Although the majority of doctors were found to accept that the responsibility for updating vaccination schedules corresponds to the rheumatologist, it is important to remark that 53 of the 122 respondents answered that they did not usually include vaccination history in clinical files, making it paradoxical that they accept responsibility for updating vaccination plans.
In our study fewer than 50% of doctors in the public and private sectors include vaccination plans in patient files, so that this would hinder finding the current rate of vaccination by reviewing these files.
20.69% of the rheumatologists stated that they do not recommend vaccination because they consider other aspects to be more important when patients consult, and 3.45% answered that they did not do so because of lack of time. The latter problem is usually associated more with the workload in public institutions, as well as the few doctors who specialise in rheumatology in comparison with the number of rheumatological patients in the country.
Respecting the moment when pneumococcus and influenza vaccines are administered, 54.6% of the respondents stated that the moment when the vaccine is administered is not important. The current recommendation is that vaccines should be administered at least 2 weeks before the start of treatment with DMARD, because methotrexate and the biological agents such as abatacept and rituximab may reduce the humoral response to vaccines, while tofacitinib reduces the response to pneumococcus vaccine.
In our survey 22.13% of respondents answered that they only recommend immunisation against influenza or pneumococcus prior to administering biological agents or tofacitinib. This shows that a high percentage are unaware that vaccination is indicated for all RA patients, or they consider that the risk of suffering one of these infections only increases in the case of starting these types of treatment.
Respecting the safety of vaccine use, 33.33% of the rheumatologists stated that the reason why their patients do not use a vaccine is because they are afraid of possible adverse effects, while more than half (65/122) stated that patients do not use them due to lack of information. It is therefore important for doctors to be well-documented regarding immunisation, so that they are able to confidently recommend vaccines to patients.
These gaps in knowledge could be corrected by applying strategies such as talks on immunisation in rheumatology meetings or congresses, thereby reinforcing rheumatologists’ knowledge of this subject.
Influenza vaccine is recommended more than the one against pneumococcus, and this may be due to the wider availability of influenza vaccine. It is also possible that doctors as well as patients pay more attention to influenza vaccination. These percentages could be improved by the creation of exclusive strategies within the speciality, so that for example it would be necessary in public medicine for patients to be up-to-date with their vaccination schedule prior to the administration of a DMARD or biological agents.
It has to be said that this study does not reflect current patient coverage by vaccination, only the percentage that rheumatologists say they recommend; the actual coverage in Mexican patients is probably even lower.
This study shows that the recommendation to administer herpes zoster vaccine has yet to be accepted, and the rheumatology community is still not fully knowledgeable about it, as there are fears about the adverse effects it may cause because it is a live virus vaccine.
It was impossible in our study to determine the differences between vaccination rates in the public and private sectors with exactitude. Nevertheless, it would be useful to determine whether adherence to recommendations and the vaccination rate were higher in the public sector than is the case in the private sector, as public institutions usually have a vaccination card which allows them a higher level of control, while also offering free vaccinations. However, on the other hand public sector doctors have less time to spend with patients and a greater workload.
Finally, it is striking that 14.7% of the respondents said that patients did not take the vaccine because of its cost. This is important, given that in the private sector we have to be aware that the diagnosis of a chronic disease such as RA involves a major expense for the patient and their family. This means that failure to properly explain the importance of vaccination for the progress of the patient may easily lead to any recommendation for it to be considered by the patient as irrelevant.
An important distortion in this study is that the questions are subjective, and we lack hard data which would show the exact degree of adherence to recommendations for vaccination; for this it would be necessary to interview the patients of these doctors and compare both results, or to have access to clinical files.
ConclusionsAccording to the data obtained in this study we are able to conclude that there is still insufficient information on the importance of vaccination for patients with RA. It also indicates that the degree of compliance with recommendations for vaccination and awareness of the safety and ideal moment for vaccine administration are at a low level in Mexico, particularly in the case of the herpes zoster vaccine.
It is important to underline the need to investigate clinical files to gather data on the immunisation of patients with RA, as well as to implement strategies in the country to increase the awareness of rheumatologists about the vaccination of their patients. The aim is to improve vaccination coverage in patients who are immunocompromised due to RA and to prevent complications because of infections that would increase the morbidity and mortality of the disease.
The education of rheumatologists should be enhanced by talks in national conferences and information in national journals to publicise the current recommendations. Information should also be supplied about the optimum time to commence patient vaccination, as this is also the best way to educate RA patients about the importance of these measures in preventing complications.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Cepeda-Perez AS, Tello Winniczuk N, Diaz-Borjon A. Adherencia a las recomendaciones actuales de inmunización en pacientes con artritis reumatoide en México. Reumatol Clin. 2021;17:155–159.