Antiphospholipid syndrome is characterised by abortions or thrombotic phenomena associated with specific antibodies. Anticoagulant therapy is based on vitamin K antagonists. We present two cases in which the use of rivaroxaban achieved control of the disease after the failure of acenocoumarol.
El síndrome antifosfolipídico se caracteriza por abortos o fenómenos trombóticos asociado a anticuerpos específicos. El tratamiento se basa en la anticoagulación con los antagonistas de la vitamina K. Presentamos 2 casos en los que el empleo del rivaroxabán ha logrado controlar la enfermedad tras su fracaso con acenocumarol.
Antiphospholipid syndrome (APS) is an autoimmune disease characterised by thrombosis or foetal loss associated with the presence of specific persistent antibodies (lupus anticoagulant, anticardiolipin and/or anti-beta2-glycoprotein). The standard treatment for patients with a history of venous thromboembolic disease (VTED) in the acute phase is unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH) followed by a vitamin K antagonist (VKA). If VKA fails, the therapeutic range can be increased, prescribing an LMWH and/or combining acetylsalicylic acid (especially if there is associated arterial thrombosis).1 We present 2 clinical cases of VTED in the context of APS where rivaroxaban was used after failing to achieve adequate control with VKA.
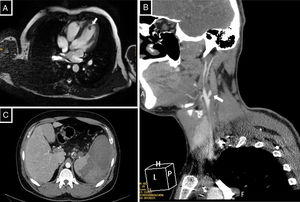
Clinical ObservationClinical Case 1A 30-year-old male patient, with a diagnosis of primary APS due to lupus anticoagulant, with no other history of interest, who started manifestations of recurring and chronic VTED in the lower limbs at the age of 17. Treatment with acenocoumarol was started, and the patient had a labile international normalised ratio (INR), despite exhaustive controls. The patient required supplementary LMWH when he did not achieve the therapeutic range. At the age of 25, after study of a transient ischaemic attack, an intracardiac thrombus that was refractory to intravenous sodium heparin was found, for which the patient was operated (Fig. 1A). Treatment was intensified with acenocoumarol with an INR of between 2.5 and 3.5, combined with 100mg aspirin every 24h. A year later, the patient had a stroke of the middle right cerebral artery secondary to thrombosis of the right internal carotid artery (days earlier his INR was near 7, and therefore his regimen was changed; he had an INR of 1.3 on arrival at the hospital). He underwent intravenous fibrinolysis which was not successful (Fig. 1B). The time in therapeutic range (TTR), according to the Rosendaal method, of the acenocoumarol over the year before the ischaemic attack was 46%. Subsequently, having failed to achieve optimal control with acenocoumarol, the patient was changed to warfarin and continued to have highly fluctuating INR levels, therefore treatment was started with rivaroxaban 20mg every 24h as compassionate use. After 3 years of follow-up of the rivaroxaban treatment, the patient had had no further thrombotic events, and had maintained enzyme-linked immunosorbent assay d-Dimer levels within the normal range.
(A) Cardiac magnetic resonance with gradient-echo images of 4 chambers. Intracavitary polypoid lesion 12×9mm dependent on the endocardium in the apical region of the left ventricle, isointense with no significant contrast enhancement. (B) CT angiography of supra-aortic trunks with axial slice image. A thrombus can be observed in the right carotid system adhering to the right internal carotid artery from its origin, reducing its calibre and resulting in occlusion of the artery. (C) Abdominal CT showing thrombosis of the splenic vein of the porta hepatis with an extensive are of splenic infarction.
A 26-year-old male, with APS due to lupus anticoagulant associated with systemic lupus erythematous (SLE) that had started 10 years earlier with joint, skin and kidney involvement (diffuse proliferative glomerulonephritis with nephrotic syndrome). Under maintenance treatment with mycophenolate mofetil 1000mg/12h, prednisone 2.5mg, aspirin 100mg, losartan 50mg and hydroxychloroquine 200mg every 24h, with stability of the SLE and no signs of kidney involvement. The patient had an episode of pulmonary thromboembolism at the age of 19 and started treatment with acenocoumarol. Three years later, he had an episode of VTED in the lower left limb, which was not in the therapeutic range (INR 1.2). Subsequently he maintained more exhaustive controls of VKA and supplementary LMWH, if it was necessary. At the age of 24, he suffered a splenic infarction secondary to thrombosis of the splenoportal axis (Fig. 1C), with an INR of 3.4 and TTR of 71% over the year before the event. In the acute phase he received treatment with LMWH at therapeutic doses (enoxaparin mg/kg/12h), and after clinical and radiological stability was achieved continued with rivaroxaban 20mg/24h as compassionate use. Since then no further VTED event over a follow-up period of 2 years has been observed on X-rays, checkups and lab tests.
DiscussionWe present 2 clinical cases of thromboembolic disease for which treatment with rivaroxaban managed to stabilise APS after failure with antivitamin K. Traditionally UFH or LMWH have been used in the acute phase, sequenced to AVK. For refractory cases, in maintenance therapy with, AVK the INR range of the AVK agents has been increased or LMWH used, combined with anticoagulants depending on the case.1 Prolonged used of low molecular weight heparin is harmful to the patient because it is administered subcutaneously, it causes discomfort, especially locally at the puncture site, and there is the possibility of adverse effects, such as reduced bone mineral density, thrombocytopenia and hypertransaminasaemia.
The therapeutic target of the new oral anticoagulants (NOAC), such as rivaroxaban (anti-Xa), have a similar mechanism of action to that of LMWH. Because this is a drug with a predictable action and low drug interaction rate, it has a promising future for patients who have been poorly controlled with the classical anticoagulant therapy. Furthermore, rivaroxaban, according to recent research, might have the additional benefit of limiting complement activation,2 and in results of the RAPS study (phase II) is not inferior to warfarin for APS.3 NOACs have been used for APS, usually with favourable results.4–7 The series published by Malec et al. is worthy of note, with 56 patients (49 treated with rivaroxaban) with a mean follow-up of 22 months, and 5.8% recurrence of VTED per year.5 In the research studies by Haladyj and Olesinska on 23 patients and Son et al. on 12 patients treated with rivaroxaban, 1 and 2 cases recurred, respectively.4,7 Development of thrombotic events should also be mentioned after replacing warfarin with a NOAC, as in the study published by Schaefer et al. with a series of 3 patients (one with dabigatran and 2 with rivaroxaban8), and one case of catastrophic APS after changing warfarin for rivaroxaban.9 Clinical trials are currently being developed to determine the role of the NACOs in APS.3,10
In both clinical cases (one due to poor control of anticoagulation with fluctuating INR levels, and the other with thrombosis phenomena despite appropriate oral anticoagulation with AVK), treatment with rivaroxaban was proposed with check-up, lab test and imaging follow-up, without revealing any new thrombotic phenomena, and showing good control of APS.
ConclusionsTreatment with rivaroxaban could be considered a therapeutic alternative for patients with APS not controlled with AVK. New research studies will establish the role of the NACOs in APS.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that neither human nor animal testing has been carried out under this research.
Data confidentialityThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of InterestsThe authors have no conflict of interest to declare.
Please cite this article as: Mateos Rodríguez JJ, Bellido D, Castro D, Portillo Sánchez J, Vanegas R, Núñez García A. Rivaroxabán en síndrome antifosfolipídico tras fracaso con acenocumarol: a propósito de 2 casos. Reumatol Clin. 2019;15:e33–e35.