Neurological involvement in Behçet's disease is rare, especially at the onset. It can present in the form of parenchymal changes or as damage to the vascular structures in its nonparenchymal form. The coexistence of both kinds of manifestations in the same patient is exceptional. We report the case of a 32-year-old patient with a history of deep venous thrombosis, who was being treated for holocranial headache, apathy, and oral and genital ulcers. Brain magnetic resonance imaging showed hyperintense lesions in the basal ganglia and white matter, and the vascular study evidenced venous thrombosis of the left transverse sinus. After confirming the diagnosis of Behçet's disease with parenchymal and nonparenchymal cerebral involvement, immunosuppressive and corticosteroid therapy was started, resulting in the remission of the symptoms.
La afectación neurológica en la enfermedad de Behçet es poco frecuente, especialmente como comienzo de la enfermedad. Puede presentarse con alteraciones parenquimatosas o con daño de las estructuras vasculares en su forma extraparenquimatosa. Es excepcional que ambos tipos de manifestaciones coexistan en un mismo paciente. Presentamos el caso de una paciente de 32 años, con antecedentes de trombosis venosa profunda, que acudió a nuestro centro por cuadro de cefalea holocraneal, apatía, aftas orales y genitales. La resonancia magnética cerebral mostró lesiones de hiperseñal en ganglios de la base y sustancia blanca silviana, y el estudio vascular trombosis venosa de seno transverso izquierdo. Tras confirmarse el diagnóstico de enfermedad de Behçet con afectación cerebral intra y extraparenquimatosa, se inició tratamiento inmunosupresor y corticoideo con remisión de la sintomatología.
Behçet's disease (BD) is a chronic recurrent inflammatory syndrome characterized by systemic vasculitis. The clinical manifestations include recurrent genital and oral ulcers, uveitis, skin sores and polyarthralgia. Involvement of the nervous system is observed in approximately 5% of all the cases and can be demonstrated with variable symptoms.
Clinical ObservationThe patient was a 33-year-old woman with a history of iliofemoral deep venous thrombosis of unknown etiology. She came to our hospital with a 4-month history of clinical manifestations of headache involving the entire head and conduct disorder. Over the preceding 3 months, she had developed painful genital and oral ulcers. Physical examination revealed erythematous lesions on the gluteus and the labia minora, both of which were painful. The neurological examination demonstrated psychomotor impairment and bradypsychia, with an excessive indifference toward her disease.
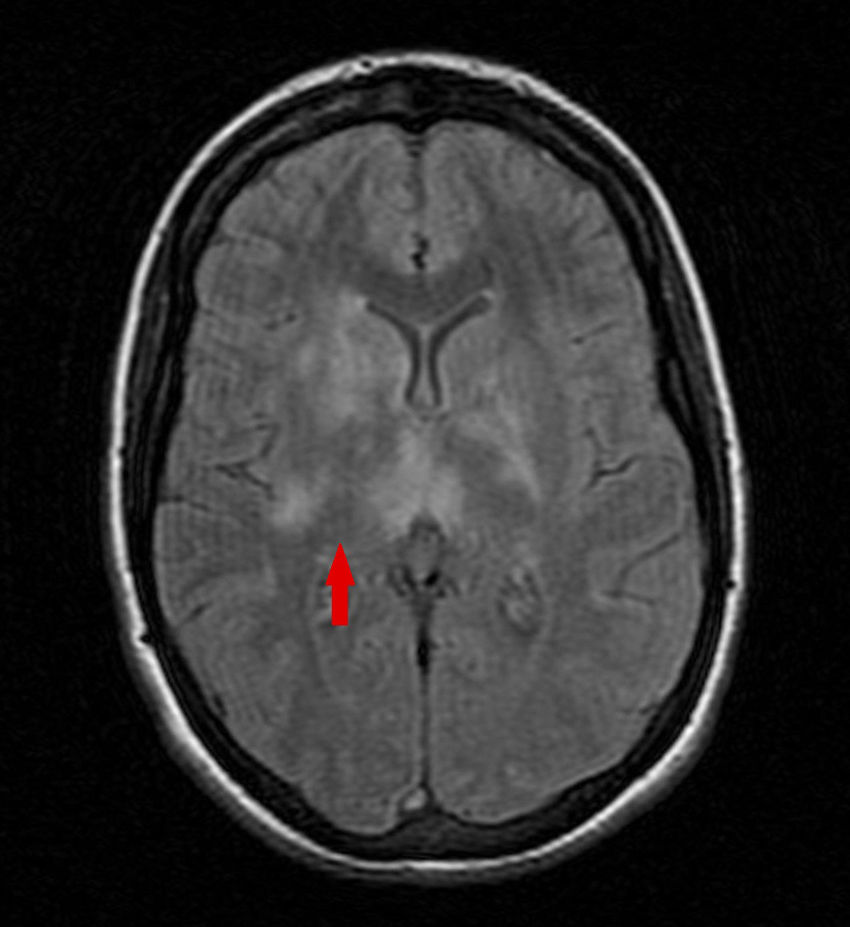
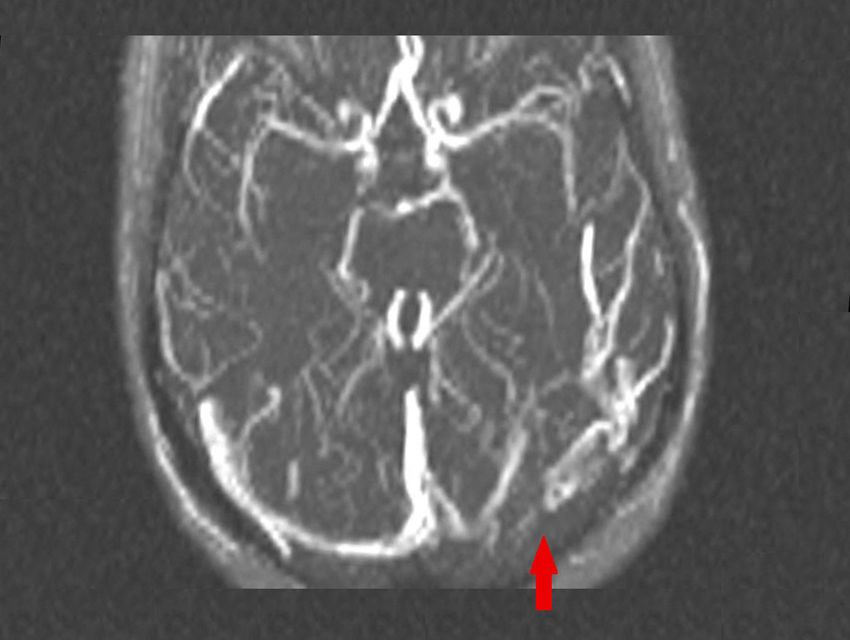
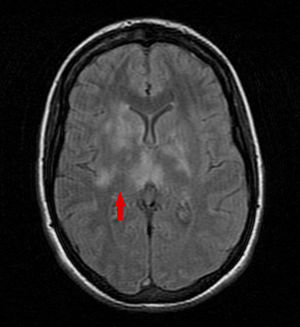
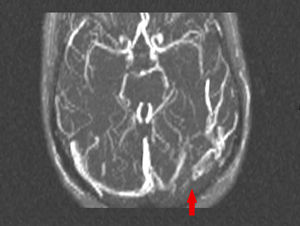
She underwent lumbar puncture which revealed lymphocytic pleocytosis (clear fluid, leukocyte count 102/mm,3 with 90% lymphocytes, glycorrhachia of 51mg/dL and proteins at 30mg/dL), with absence of microorganisms and negative cultures. Brain magnetic resonance imaging (MRI) showed lesions with a hyperintense signal in T2 and fluid-attenuated inversion recovery (FLAIR) sequences in basal ganglia and bilateral white matter (Fig. 1). A vascular study revealed defects in the signal intensity due to venous thrombosis in left transverse sinus and ipsilateral sigmoid sinus (Fig. 2).
After confirmation of the diagnosis of BE (classification criteria of the International Study Group, replaced in 2006 by the International Criteria for Behçet's Disease1) with intra- and extraparenchymal neurological involvement, we proposed treatment with a combination of an intravenous corticosteroid and warfarin (intolerance to acenocoumarol). The progress of the patient was satisfactory, with remission of all of the symptoms. At discharge, we prescribed immunosuppressive therapy with azathioprine. After 1 year of follow-up, she is asymptomatic and has not developed any of the symptoms related to the disease.
DiscussionBehçet's disease is multisystemic and, thus, has variable symptoms. Involvement of the nervous system ranges between 5.3% and 59% of the patients depending on the series,2 and it is usually preceded by other forms of the disease. It is an uncommon complication that is associated with high morbidity and mortality rates. Thus, it is necessary to have an in-depth knowledge of the characteristic symptoms and lesions as portrayed in imaging tests. We have little data on this condition, as studies have been carried out in small series of patients.
The central nervous system (CNS) is the site where the neurological involvement is most likely to be encountered. The peripheral nervous system can also be affected, usually in a subclinical form, which is confirmed by means of electrophysiological studies.3 Depending on the main site of the lesions in the CNS, there are 2 major patterns. The first, with involvement of the cerebral parenchyma, develops in 20%–60% of the cases. It is characterized by small inflammatory lesions in the brain stem and the basal ganglia, which should be considered in the differential diagnosis of diseases like multiple sclerosis (MS). These lesions can provoke symptoms due to cortical involvement, pyramidal syndrome or conduct disorder.4 Sensory symptoms, movement disorders and epilepsy have also been reported.5,6 The acute form is associated with a good response to treatment, but chronicity can provoke brain atrophy and predicts a more aggressive course.7 The spinal cord can also be affected, either due to the proximity of the lesions or in an isolated manner, which constitutes a factor indicating a poor prognosis. The most common type is multifocal transverse myelitis.8 The second pattern is caused by damage to vascular structures, basically by thrombosis of the cerebral venous sinuses, which occurs in 10%–20% of the patients.9 This can affect the entire venous system, with predominance of the superior sagittal and transverse sinuses. It usually presents as a syndrome of intracranial hypotension and, to a lesser extent, with focal symptoms or epileptic seizures.10 Cerebral infarctions are less frequent; they can simultaneously affect small and large arteries,11,12 and the venous and arterial systems.
Concerning the clinical manifestations of the disease, headache is the most common neurological symptom; it is observed in 50%–80% of the cases and is due to direct neurological involvement in only 10%.13 The impact of BD on cognitive functions is frequently reported, and may be associated with the site of the lesions. The presence of bipolar disorder or paranoid symptoms and, occasionally, indifference and apathy with respect to the disease.14 Anxiety and depression are more frequent psychiatric symptoms, with an incidence of up to 86% in some studies, and a higher prevalence than in other autoimmune disorders.
Behçet's disease is a clinical condition in which the diagnostic criteria are well established and defined. However, there are no validated criteria for neurological involvement.1 Usually, the clinical presentation, neuroimaging findings and changes in the cerebrospinal fluid (CSF) are sufficient to confirm the diagnosis. Brain MRI has a major role in the diagnosis and constitutes the gold standard, as it enables the differential diagnosis for MS, systemic lupus erythematosus and other autoimmune diseases. The components of CSF are changed in 60%–80% of the patients, with hypercellularity, normal glucose levels and a slight increase in proteins.
ConclusionsBehçet's disease is an inflammatory, chronic and recurrent syndrome, characterized by systemic vasculitis. The involvement of the nervous system in this condition is infrequent. The most common form of neuro-Behçet's disease is due to the involvement of the cerebral parenchyma and, to a lesser extent, vascular damage. The simultaneous development of both patterns, as in the case we report, has been observed in less than 1% of the series.15 Headache is the main neurological symptom, although, in most cases, the headache is primary. The involvement of higher functions is common and is manifested with a number of psychiatric symptoms. In the case we present, we point out the coexistence of the intra- and extraparenchymal forms, and the initial clinical presentation with tension headache and conduct disorder.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: López Bravo A, Parra Soto C, Bellosta Diago E, Cecilio Irazola Á, Santos-Lasaosa S. Manifestaciones neurológicas de la enfermedad de Behçet: descripción de un caso y revisión de la literatura. Reumatol Clin. 2019;15:e36–e38.