To study the differences between rheumatoid arthritis (RA)-interstitial lung disease (ILD) patients and RA patients without ILD in severity markers and disease activity and to identify factors associated with the presence of ILD in RA patients.
Patients and methodsPatients: RA-ILD patients selected from a multicentre cohort in Andalusia, Spain. Controls: RA-patients without ILD paired by sex, age and disease duration. Protocol: RA patients are reviewed every 3–6 months in rheumatology consultation. All patients are reviewed according to a predetermined protocol with systematic data collection. Outcomes: description of ILD type, differences in severity markers and disease activity in both groups. Other variables: ILD type by imaging technique (HRCT): nonspecific interstitial pneumonia (NSIP)/usual interstitial pneumonia (UIP). Lung function by PTF. Activity and severity markers of arthritis by DAS28-ESR, HAQ, RF, ACPA and erosions. Treatment with DMARD. Statistical analysis: descriptive and paired T-test or Chi-square test followed by binary logistic regression (DV: ILD in patients with RA).
ResultsEighty-two patients were included, 41 RA-ILD and 41 RA controls. RF and ACPA positivity, serositis and osteoporosis were more frequent in RA-ILD patients. No significant differences in DAS28 were observed (P=.145) between RA-ILD and RA control patients. RA-ILD patients presented worse HAQ scores (P=.006). All patients were treated with disease modifying antirheumatic drugs (DMARDs). The risk of developing ILD in RA patients is tripled by a history of smoking or the presence of erosive arthritis (R2=.36).
ConclusionsThe results of our study support the higher frequency of UIP and NSIP in RA patients. DLCO is the most sensitive parameter to detect ILD in RA patients. Our study showed that ILD in RA patients was associated with RA severity (presence of erosions and ACPA) and with a history of smoking.
Estudiar las diferencias en pacientes con artritis reumatoide (AR) y enfermedad pulmonar intersticial (EPID) y pacientes con AR sin EPID, e identificar factores asociados con la EPID en pacientes con AR.
Pacientes y métodosEstudio observacional de casos y controles. Pacientes: se seleccionaron pacientes de una cohorte con AR y EPID de diferentes centros de Andalucía. Controles: pacientes con AR sin EPID pareados por edad, género y tiempo de evolución. Protocolo: los pacientes con AR se revisan cada 3-6 meses en consulta. Todos los pacientes son revisados de acuerdo con un protocolo predeterminado con recogida de datos sistemática. Desenlaces: descripción del tipo radiológico de EPID, diferencias en los marcadores de gravedad en casos y controles y en la actividad de la enfermedad. Otras variables: descripción del tipo de EPID por TACAR: neumonía intersticial usual (NIU), neumonía intersticial no específica (NINE) y de la función pulmonar por PFR; marcadores de actividad y gravedad de artritis: DAS28, HAQ, FR, ACPA, erosiones. Tratamiento con FAME. Análisis: descriptivo, χ2 o t de Student, seguida de regresión logística binaria (Vd:EPID en pacientes con AR).
ResultadosSe incluyeron 82 pacientes: 41 con AR y EPID y 41 controles AR sin EPID. Los pacientes con EPID presentaron un mayor porcentaje de pacientes con FR y ACPA positivos y una mayor frecuencia de serositis y osteoporosis. No hubo diferencias significativas en DAS28 en casos y controles(p=0,145), pero los pacientes de AR con EPID presentaron peor HAQ (p=0,006). Todos los pacientes estaban en tratamiento con FAME. El análisis multivariante mostró que los pacientes con AR exfumadores y con artritis erosiva triplicaron el riesgo de presentar EPID (R2=0,36).
ConclusionesLos resultados de nuestro estudio apoyan la mayor frecuencia de NIU y NINE en pacientes con AR, así como la alteración de DLCO como el parámetro más importante. Los pacientes con AR y EPID se asociaron con una enfermedad más grave (erosiones y ACPA) y con el tabaco.
Rheumatoid arthritis (RA) is an immune-mediated inflammatory disease of unknown cause and chronic course. It primarily affects the joints, but extra-articular clinical manifestations are common. The lung is one of the most frequently affected organs and causes significant morbidity and mortality.1,2 Interstitial lung disease (ILD) is the most common non-plural lung manifestation in RA. Between 8% and 10% of patients develop clinically significant ILD, while subclinical ILD, detected by systematic screening, occurs in 22%–33% of patients with established RA.3 This condition has been associated with a poor prognosis,4 and therefore greater knowledge of its characteristics (e.g., histopathological type) and the discovery of risk factors associated with its development are of great importance in its diagnosis and treatment.5
Variables associated with RA with ILD include male sex,6 elevated levels of rheumatoid factor (RF), erythrocyte sedimentation rate (ESR) and smoking. The most recent studies also involve anticitrullinated peptide antibodies (ACPA).7 Because of the connection between tobacco smoke and the development of ACPA, it is believed that this toxic substance may influence both the pathogenesis of RA and its complications.8 Therefore, smoking may be a preventable risk factor for susceptibility to RA, RA-associated ILD and idiopathic pulmonary fibrosis.9,10
Synthetic (sDMARD) and biological (bDMARD) disease modifying drugs are the primary treatment for RA, although glucocorticoids, non-steroidal anti-inflammatory drugs (NSAIDs) and analgesics are also used as symptomatic treatment.11 Studies in RA and ILD patients treated with DMARDs are few and contradictory. In addition, these patients are usually excluded from clinical trials due to the condition. All this has led to a restriction of their use and remains a challenge for clinicians. Therefore, there is a need to better understand the characteristics of patients treated with DMARDs in routine clinical practice.12,13 The objectives of this study are: (1) to describe the clinical, radiological, respiratory functional and echocardiographic characteristics of a prospective cohort of RA and clinical ILD patients treated with DMARDs in routine clinical practice and (2) to study the possible association of severity factors (e.g., ACPA positivity, erosions) with RA-associated lung disease.
Patients and methodsStudy designMulticentre cross-sectional study conducted in a cohort of RA and ILD patients from different hospitals in Andalusia, Spain, and a control group of RA subjects without IDL, matched by sex and age. The recruitment period was from January 2015 to January 2017. The study was approved by the medical ethics committee, and all subjects provided written their informed consent prior to enrolment.
SubjectsPatientsAll the patients with RA and ILD treated with DMARDs were recruited consecutively from rheumatology clinics of different centres in Andalusia: Hospital Regional Universitario de Málaga, Hospital Virgen de la Victoria de Málaga, Hospital de Valme de Sevilla and Hospital Virgen de las Nieves de Granada. The inclusion criteria were age ≥16 years, diagnosis of RA according to the classification criteria of the American College of Rheumatology/European League Against Rheumatism 2010 (ACR/EULAR criteria 2010), ILD (American Thoracic Society/European Respiratory Criteria) and treated with DMARDs at the last visit. The exclusion criteria were the presence of any inflammatory or rheumatic disease other than RA (except secondary Sjögren's syndrome) and pregnancy.
ControlsPatients with RA without ILD were selected consecutively from a prospective cohort at the Hospital Regional Universitario de Málaga. Controls were paired by sex, age and time of disease progression. The inclusion criteria were age ≥16 years, diagnosis of RA according to the classification criteria of the American College of Rheumatology/European League Against Rheumatism 2010 (ACR/EULAR 2010 criteria) and treated at the last visit with DMARDs.
ProtocolPatients with RA and ILD who attended rheumatology consultations from January 2015 to December 2017 and met the selection criteria were treated according to a pre-established protocol for data collection. The date of this visit was used as the index date, and this visit was marked as V0. High resolution computed tomography (HRCT), respiratory functional tests (PFTs) and echocardiography were requested for all patients who had not undergone these tests in the past year. The controls were also treated using a pre-established protocol for data collection.
Variables and operational variablesPrincipal variableThe main variables analysed were: (1) description of the radiological type of ILD in RA patients and (2) difference in markers of disease severity and activity in cases and controls at the date of inclusion.
Other variablesILD variables included description of radiological type by high resolution computerised tomography (nonspecific interstitial pneumonia [NSIP], usual interstitial pneumonia [UIP]) and lung function by RFT (DLCO, FEV1, FV, FEV1/CVF); presence of pulmonary hypertension (PHT) by echocardiogram, and presence and degree of dyspnoea. HRCT was performed in the baseline assessment with a 1.5 axial section or 2mm thickness taken at intervals of 1cm along the chest and reconstructed using a high spatial frequency algorithm, taking 20–25 slices for each patient. The CT scans were evaluated by two chest radiology experts blinded to the clinical data. They were graded according to the Kazerooni score on the fibrotic component and the extent of ground glass opacities.8,9 ILD patterns were classified according to the criteria of the American Thoracic Society/European Respiratory Criteria.
The variables of RA included the duration of symptoms, extra-articular manifestations and history of smoking: current or past. In addition, the following parameters were collected at the date of inclusion: count of painful and inflamed joints, visual analogue scale of 0–10cm; disease activity measured by DAS28 (Disease Activity Score)13 and physical function by a health assessment questionnaire (HAQ).14 Severity variables were also collected at the date of inclusion: RF, measured in U/ml, was considered high when the titres were above the upper cut-off point used in our laboratory (>20U/ml) and high titre (>60U/ml); presence of ACPA, measured in U/ml: were considered positive with titres above 10U/ml, and high titre (>340U/ml); as well as the presence of radiological erosion. Treatments: sDMARD, bDMARD, other immunosuppressants or glucocorticoids that the patient was taking at the date of inclusion.
Statistical analysisFirst, a descriptive analysis of the characteristics in both groups of patients was performed. The qualitative variables were expressed as absolute numbers and their percentages; the quantitative variables, as mean and standard deviation when their distribution was normal, and as median and interquartile range when not normal. The goodness of fit of the continuous variables was confirmed with the Kolmogorov–Smirnov test. The χ2 or Fisher's test was performed as appropriate, and for quantitative variables, the Student's t-test for independent samples or Mann–Whitney in cases of non-normality. Finally, a binary logistic regression analysis was performed in patients with RA and ILD (DV: ILD) to check which variables were independently associated with the presence of ILD. The sample size was calculated assuming an alpha risk of .10 and a beta risk of .2 in a bilateral contrast, and 40 subjects in each group were required to detect the difference between two proportions as statistically significant, which for group 1 was expected to be .53 and for group 2 .26.1 The analysis was performed using the Rcomander statistical programme.
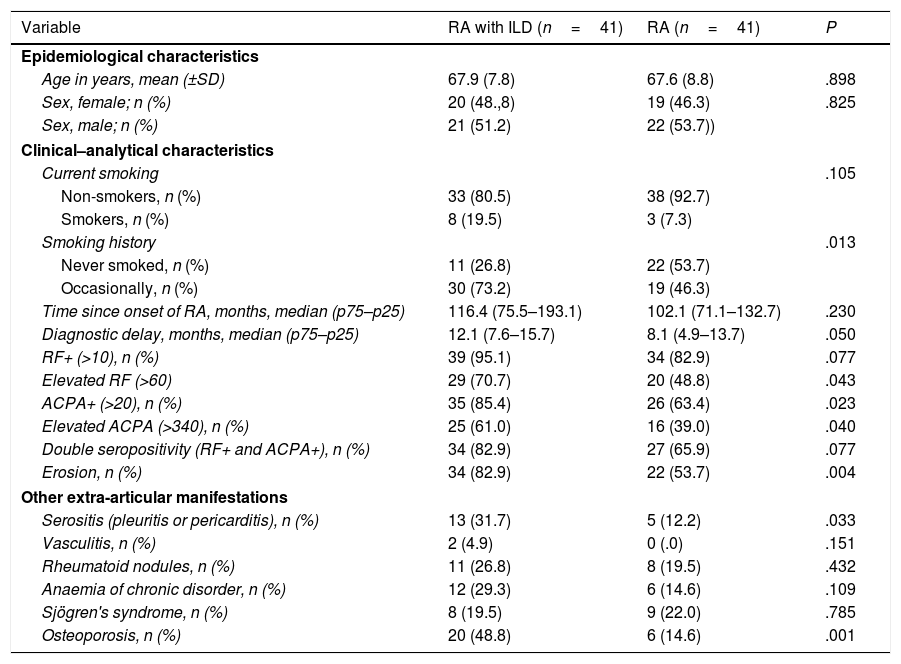
ResultBaseline characteristicsThe study population comprised 82 RA patients: 41 RA patients with ILD and 41 RA patients without ILD. All the patient with IDL had been previously diagnosed by CT. The baseline characteristics of both patient groups are shown in Table 1. Although there were no differences between either group in most clinical and epidemiological parameters, a higher percentage of patients with ILD were ex-smokers (P=.013), with erosive disease (P=.004) and double or single seropositive. The group of patients with ILD had a higher percentage of RF-positive (P=.077), ACPA-positive (P=.023), and RF- and high-titre ACPA-positive (P=.040) patients. The patients with RA and ILD also had a higher frequency of serositis (P=.033) and osteoporosis (P=.001).
Baseline characteristics of the study population.
| Variable | RA with ILD (n=41) | RA (n=41) | P |
|---|---|---|---|
| Epidemiological characteristics | |||
| Age in years, mean (±SD) | 67.9 (7.8) | 67.6 (8.8) | .898 |
| Sex, female; n (%) | 20 (48.,8) | 19 (46.3) | .825 |
| Sex, male; n (%) | 21 (51.2) | 22 (53.7)) | |
| Clinical–analytical characteristics | |||
| Current smoking | .105 | ||
| Non-smokers, n (%) | 33 (80.5) | 38 (92.7) | |
| Smokers, n (%) | 8 (19.5) | 3 (7.3) | |
| Smoking history | .013 | ||
| Never smoked, n (%) | 11 (26.8) | 22 (53.7) | |
| Occasionally, n (%) | 30 (73.2) | 19 (46.3) | |
| Time since onset of RA, months, median (p75–p25) | 116.4 (75.5–193.1) | 102.1 (71.1–132.7) | .230 |
| Diagnostic delay, months, median (p75–p25) | 12.1 (7.6–15.7) | 8.1 (4.9–13.7) | .050 |
| RF+ (>10), n (%) | 39 (95.1) | 34 (82.9) | .077 |
| Elevated RF (>60) | 29 (70.7) | 20 (48.8) | .043 |
| ACPA+ (>20), n (%) | 35 (85.4) | 26 (63.4) | .023 |
| Elevated ACPA (>340), n (%) | 25 (61.0) | 16 (39.0) | .040 |
| Double seropositivity (RF+ and ACPA+), n (%) | 34 (82.9) | 27 (65.9) | .077 |
| Erosion, n (%) | 34 (82.9) | 22 (53.7) | .004 |
| Other extra-articular manifestations | |||
| Serositis (pleuritis or pericarditis), n (%) | 13 (31.7) | 5 (12.2) | .033 |
| Vasculitis, n (%) | 2 (4.9) | 0 (.0) | .151 |
| Rheumatoid nodules, n (%) | 11 (26.8) | 8 (19.5) | .432 |
| Anaemia of chronic disorder, n (%) | 12 (29.3) | 6 (14.6) | .109 |
| Sjögren's syndrome, n (%) | 8 (19.5) | 9 (22.0) | .785 |
| Osteoporosis, n (%) | 20 (48.8) | 6 (14.6) | .001 |
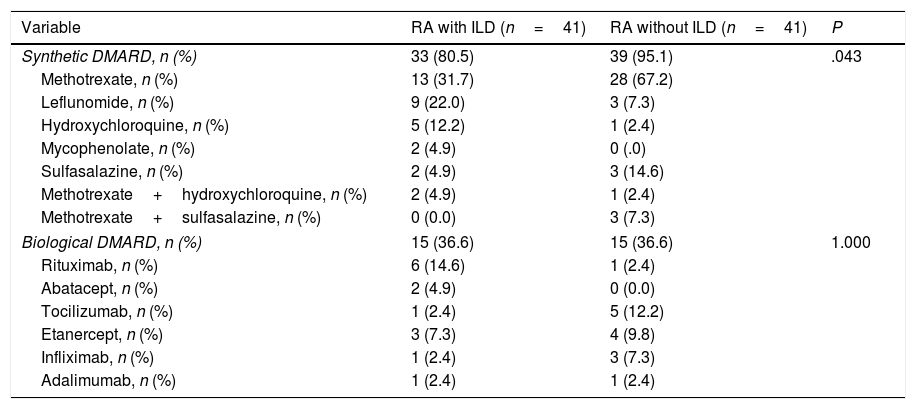
All the patients were under treatment with DMARDs. Among the patients with RA and ILD: 9 (21.9%) were taking a bDMARD with an sDMARD, the most common combination being DMARD +RTX (12.1%); 25 patients (60.9%) were receiving sDMARDs in monotherapy, most commonly methotrexate (MTX) (48%), and 7 (17.0) monotherapy with a bDMARD (Table 2). Among the RA patients without ILD, bDMARD monotherapy was also the most frequent in 26 patients (63.4%), with MTX also the most frequent, followed by combination therapy in 13 patients (31.7%); only 2 patients were on bDMARD monotherapy (4.8%).
DMARD treatment.
| Variable | RA with ILD (n=41) | RA without ILD (n=41) | P |
|---|---|---|---|
| Synthetic DMARD, n (%) | 33 (80.5) | 39 (95.1) | .043 |
| Methotrexate, n (%) | 13 (31.7) | 28 (67.2) | |
| Leflunomide, n (%) | 9 (22.0) | 3 (7.3) | |
| Hydroxychloroquine, n (%) | 5 (12.2) | 1 (2.4) | |
| Mycophenolate, n (%) | 2 (4.9) | 0 (.0) | |
| Sulfasalazine, n (%) | 2 (4.9) | 3 (14.6) | |
| Methotrexate+hydroxychloroquine, n (%) | 2 (4.9) | 1 (2.4) | |
| Methotrexate+sulfasalazine, n (%) | 0 (0.0) | 3 (7.3) | |
| Biological DMARD, n (%) | 15 (36.6) | 15 (36.6) | 1.000 |
| Rituximab, n (%) | 6 (14.6) | 1 (2.4) | |
| Abatacept, n (%) | 2 (4.9) | 0 (0.0) | |
| Tocilizumab, n (%) | 1 (2.4) | 5 (12.2) | |
| Etanercept, n (%) | 3 (7.3) | 4 (9.8) | |
| Infliximab, n (%) | 1 (2.4) | 3 (7.3) | |
| Adalimumab, n (%) | 1 (2.4) | 1 (2.4) | |
With regard to disease activity parameters, no differences in the median were observed in either of the patient groups (p75–p25) in TJC (P=.590), NIA (P=.834), CRP (P=.338), ESR (P=.320) or DAS28 (2.7 [2.3–3.3] vs. 2.29 [1.9–3.2]; P=.145). Quality of life was shown to be worse in the patients with ILD measured by HAQ (1.20 [.5–1.7] vs. .75 [.0–.0]; P=.006).
Lung characteristics of the patients with rheumatoid arthritis and interstitial lung diseaseWith regard to the patients’ respiratory symptoms, at the assessment date most described moderate effort dyspnoea (25; 61.0%), 14 patients (34.1%) has no dyspnoea and only 2 patients (4.9%) had minimal effort dyspnoea with home oxygen therapy. The patients without dyspnoea had better mean (SD) O2Sat than the patients with moderate and minimal effort dyspnoea (97.15 [2.5] vs. 95.12 [2.2] vs. 95.0 [.7]).
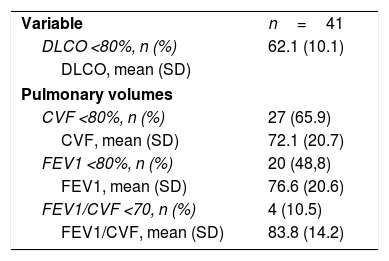
The PFT alterations included a reduction in DLCO diffusing capacity in most of the patients. Forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1) were below 80 in slightly more than half the patients, but the FEV1/FVC ratio was mostly normal (Table 3). DLCO <70 was associated with erosions (<.001), elevated RF (.038) and positive ACPA (.039). Four patients (9.8%) had PHT on the echocardiogram.
Respiratory function tests in patients with RA with ILD.
| Variable | n=41 |
| DLCO <80%, n (%) | 62.1 (10.1) |
| DLCO, mean (SD) | |
| Pulmonary volumes | |
| CVF <80%, n (%) | 27 (65.9) |
| CVF, mean (SD) | 72.1 (20.7) |
| FEV1 <80%, n (%) | 20 (48,8) |
| FEV1, mean (SD) | 76.6 (20.6) |
| FEV1/CVF <70, n (%) | 4 (10.5) |
| FEV1/CVF, mean (SD) | 83.8 (14.2) |
The most common histopathological types described by HRCT were usual interstitial pneumonia in 27 patients (65.9%) and nonspecific interstitial pneumonia in 13 (31.7%). Only one patient (2.3%) had an organising pneumonia. Three patients had a combination of NSIP and UIP, but eventually described as dominant type.
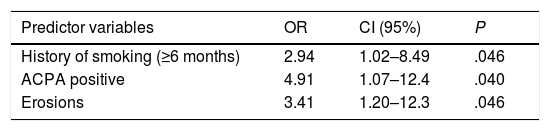
Factors associated with interstitial lung diseaseThe multivariate analysis showed that patients with a history of smoking of at least 6 months and erosive arthritis tripled the risk of ILD. The variable most independently associated with ILD was the presence of ACPA (OR=4.91) (Table 4). This model would explain 36% of the variability of the presence of ILD (R2=.36).
Binary multivariate logistic regression using the presence of ILD as a dependent variable.
| Predictor variables | OR | CI (95%) | P |
|---|---|---|---|
| History of smoking (≥6 months) | 2.94 | 1.02–8.49 | .046 |
| ACPA positive | 4.91 | 1.07–12.4 | .040 |
| Erosions | 3.41 | 1.20–12.3 | .046 |
Nagelkerke's R2=.371.
Predictor variables: sex, age, history of smoking (≥6 months), erosions, ACPA positive, disease duration, DAS28, HAQ.
The RA patients treated with DMARDs and ILD in our cohort show a predominant histopathological pattern on HRCT of UIP (65.9%) or NSIP (31.7%), similar percentages to those described in the literature.14,15 We should also highlight that almost 90% of our patients had a reduced DLCO. These figures coincide with other studies, such as that of Zhang et al.,16 who found a reduced DLCO in 92% of patients with RA and ILD and describe it as the most common and sensitive physiopathological change in ILD. This is of diagnostic interest and could also be a result of screening from the onset of the disease. In fact, a recent study of RA patients highlights DLCO as a good method for preclinically identifying patients with ILD and RA.17 The latter study also describes an inverse correlation between DLCO levels and ACPA titre (−.45; P=.004).17 In our cohort the patients with ILD with a DLCO<80 were associated with erosion (<.001), elevated RF (.038) and positive ACPA (.039).
The patients with RA and ILD in our cohort had more severe disease in the form of greater association with erosive disease and presence of ACPA. We also identified more patients with a history of smoking in the patients with ILD. The higher prevalence of ACPA detected in our RA-ILD patients compared to the RA patients without ILD is in line with most studies,5,18–20 although there are some in whom this association was not seen.21,22 These differences could be explained by the type of population, the definition of the disease or the methodology for detecting clinical parameters. The varying sensitivity and specificity of the methods for detecting ACPA may also affect their value when assessing the association with ILD. The significantly higher positivity in the patients with RA and ILD could indicate that the presence of ACPA could be a good biomarker for diagnosing ILD in patients with RA. It is believed that lung injury from smoking and other stimuli could contribute to protein citrullination modification, which later creates new epitopes and subsequent autoimmune responses.20 In this regard, a previous history of smoking (for at least 6 months) is associated with ILD in RA, and multiple studies have demonstrated this association.23,24
In terms of the treatment used, the patients with RA and ILD took more sDMARDs than those without ILD, mainly at the expense of MTX; this could be due to the contradictory data described with this DMARD: a meta-analysis of randomised controlled trials describing an increased risk of pneumonitis associated with MTX (RR: 7.81, 95% CI: 1.76–34.72).25 Subsequently a group of experts expressed their disagreement with this, among other reasons because of the non-specific definition of the term pneumonitis.26 They described the course of lung function in a cohort of patients with RA and ILD and observed improved lung function tests after treatment with corticosteroids plus DMARDs (MTX, LFN or AZA).27 With regard to treatment with bDMARDs, in these patients the evidence is even more uncertain. The few studies carried out describe abatacept and rituximab as drugs that could be effective and safe in the treatment of RA with IDL, both at joint level and in stabilisation, even with improvement in respiratory parameters.28,29 In line with the data described, the distribution of the use of biological therapy in our patients was consistent: higher use of rituximab and abatacept in patients with ILD versus anti-TNF and tocilizumab in the group without ILD. The fact that both patient groups are under treatment could explain why there was no difference in inflammatory activity measured by DAS28 and APR (CRP and ESR) in both groups of patients. The study by Restrepo et al.,10 like ours, also presents a lower percentage of patients treated with MTX due to contradictory data regarding its pulmonary toxicity. However, they associate this under-treatment with a higher DAS28 in these patients. This might be due to the fact that the patients with ILD in their study were older and had a longer disease duration than those without ILD, which was not the case in our study, because we matched them by sex, age and time since onset.
Among this study's limitations, since it was performed in routine clinical practice, were that no PFT or HRCT were performed in the group of RA patients without a diagnosis of ILD because they had no associated symptoms and unaltered chest X-rays. Although according to various studies17 there could already be alterations in PFT and on HRCT in the preclinical phase, in these routine practice patients these tests were requested due to suspected pulmonary involvement. This study is an observational analysis of a cohort of patients with RA and ILD, in whom we prospectively analyse the parameters of respiratory function over time, and a cohort of patients with RA without clinical respiratory symptoms. The study was conducted under routine clinical practice conditions and its results could be extrapolated to situations in this field, although longitudinal studies with a larger number of patients would be necessary to confirm the findings of our study and to establish causality.
To conclude, the results of our study support the higher frequency of the NIU and NINE histopathological patterns in patients with RA and ILD, as well as impaired DLCO as the most important parameter. Patients with RA and ILD are associated with more severe disease (erosions and presence of ACPA) as well as the smoking exposure factor. Treatment with DMARDs in both patient groups controls inflammatory activity, with increased use of the synthetic DMARDS HQC and leflunomide, and the bDMARDs rituximab and abatacept, in patients with ILD. We need to wait for the prospective assessment of these patients to see any association of the treatment with the course of the lung disease.
FundingAndalusian Public Foundation for Health and Biomedicine Research in Málaga (FIMABIS). Spanish Rheumatology Foundation (FER).
Conflict of interestsNatalia Mena-Vázquez: talks for MSD, UCB and Roche.
Lorena Pérez-Albaladejo: no conflict of interest.
Sara Manrique-Arija: talks/presentations for Abbvie, Pzifer and MSD.
Carmen María Romero-Barco: talks/speeches for Abbvie.
Carmen Gómez Cano: no conflict of interest to declare.
Inmaculada Ureña-Garnica: no conflict of interest to declare.
Antonio Fernández-Nebro: talks/presentations for Roche, MSD and BMS.
For the translation, to the Spanish Society of Rheumatology. Spanish Rheumatology Foundation (FER).
Please cite this article as: Mena-Vázquez N, Pérez Albaladejo L, Manrique-Arija S, Romero Barco CM, Gómez Cano C, Ureña Garnica I, et al. Análisis de las características clínico-analíticas de pacientes con artritis reumatoide y enfermedad pulmonar intersticial: casos y controles. Reumatol Clin. 2021;17:197–202.