To determine the annual number and trend of prostheses implanted in patients with rheumatoid arthritis (RA) at our hospital during the past decade.
Materials and methodsRetrospective observational study. Patients were collected through an extensive search of the database of the Clinical Documentation Service between 1998 and 2007. The data were extracted from medical records using a predesigned questionnaire. Statistical analysis of longitudinal prostheses was made using Cochrane's Q test and the Kaplan–Meier method.
ResultsSixty-one RA patients were operated on with 78 prostheses as a direct result of their disease at our hospital between 1998 and 2007. Most were women (80%) with positive rheumatoid factor (84%). The mean age was 58 years, and the average time since onset of RA was 13 years. All but one had previously received antirheumatic drugs (88% methotrexate), but only 11% had biological therapy. No changes were observed in the number of arthroplasties as a whole over a decade, although there was a trend toward reduction in the number of patients that required a knee replacement for the first time (Cochrane Q, P=.05).
ConclusionWe observed no significant changes in trends in the number of new joint replacement procedures as a whole in the past decade at our hospital, although the number of patients who required knee replacement for the first time as a direct result of their underlying disease seems to have declined in the last decade.
Conocer el número anual y la tendencia de las prótesis implantadas en nuestro hospital a los pacientes con artritis reumatoide (AR) durante la última década.
Material y métodosEstudio observacional retrospectivo. Los pacientes fueron localizados mediante búsqueda exhaustiva en la base de datos del servicio de documentación clínica entre 1998 y 2007. Los datos se extrajeron de las historias clínicas siguiendo un cuestionario prediseñado. El análisis estadístico longitudinal de las prótesis colocadas se efectuó mediante la Q de Cochrane y las curvas de Kaplan–Meier.
ResultadoSesenta y un pacientes con AR fueron intervenidos con 78 prótesis como consecuencia directa de su enfermedad en nuestro hospital entre 1998 y 2007. La mayoría eran mujeres (80%) con factor reumatoide positivo (84%). La media de edad fue de 58 años y el tiempo de evolución medio de la AR fue de 13 años. Todos excepto uno habían recibido previamente fármacos antirreumáticos (88% metotrexato), pero sólo el 11% había accedido a una terapia biológica. No se observaron cambios en el número de artroplastias a lo largo de toda la década, aunque sí hubo una tendencia a la reducción en el número de pacientes que precisaron por primera vez una prótesis de rodilla (Q Cochrane; p=0,05).
ConclusiónNo hemos observado cambios significativos en la colocación de prótesis articulares en su conjunto en la última década en nuestro hospital, aunque podría estar produciéndose un descenso del número de pacientes que acceden por primera vez a una prótesis de rodilla.
Rheumatoid arthritis (RA) is an autoimmune systemic disease, characterized by chronic inflammation and polyarticular destruction.1,2 It leads to deformity and stiffness of joints, and is associated with marked disability and reduced quality of life. Because joint damage is progressive and irreversible, severe deterioration of physical function is only partially recoverable by joint substitution.3,4
The therapeutic approach to a patient with RA requires a multidisciplinary team. The main goals of treatment are to reduce symptoms of inflammation and prevent joint destruction and limitation.5 To achieve these objectives, the use of physical therapy and rehabilitation as well as drug treatment should be considered as a whole. According to current recommendations, early and intense onset of therapy with disease-modifying antirheumatic drugs (DMARDs) is indicated. The use of DMARDs at an early stage in the course of the disease has been shown to slow the development of short-term joint damage and has a positive impact on the need for joint replacement surgery.5–7 Although these drugs reduce joint damage, they do so only moderately, so in most patients they only reduce the impact of the disease but do not entirely avoid its consequences. Several recently published studies suggest that after 1985 there has been a reduction in the need for orthopedic surgery in patients with AR through an earlier treatment of the disease and the use of more effective drugs most.8–10
Biological therapies are available in our country since 1998 and have demonstrated greater potency to inhibit joint damage than traditional DMARDs. It is therefore expected that they will play a role in helping patients avoid disability, improve their quality of life and reduce the surgical needs associated with RA in a more effective manner.11–14 However, the impact of these therapies on the indications for prosthetic surgery has not yet been evaluated in RA.
The objective of this study was to describe the tendency for prosthetic interventions in patients with RA from 1998 to 2007 in our center.
Materials and MethodsThis is a descriptive study based on the review of medical records of patients undergoing hip and knee arthroplasty in the Regional University Hospital (RUH) Carlos Haya. The study included patients with RA classified according to ACR criteria of 1987,15 with at least 14 years of age who had undergon a total knee or hip between January 1, 1998 and December 31, 2007 for the first time. We excluded patients with RA who had previously undergone surgery for hip and/or knee for any reason, and also those treated for problems such as fractures, prosthetic replacement, avascular necrosis, and so on.
Medical records of patients undergoing knee replacement and/or hip in the HRU Carlos Haya in Malaga from January 1, 1998 until December 31, 2007 were located through the clinical documentation.
A specific questionnaire was prepared for the systematic collection of the following variables: gender, age, indication of arthroplasty, the diagnosis related group (DRG), date of surgery, hospital stay, rheumatoid factor, systemic manifestations, total number and order of insertion of prostheses and treatment carried out since the beginning of RA, including biological therapies.
Statistical AnalysisAn analysis of frequencies of arthroplasties placed per each of the years of study was performed. Quantitative variables were presented as mean±standard deviation (SD). Qualitative variables were compared using the chi-square test (or Fisher exact test, as appropriate) and by quantitative t-test for unrelated samples for normally distributed variables (age, number of prostheses, the number of DMARDs and time since onset) or the Mann–Whitney U test for non-normal distributions (number of replacements). The normal setting was checked by Kolmogorov. Longitudinal statistical analysis of arthroplasties over the decade was carried out by Cochrane's Q and the Kaplan–Meier tests.
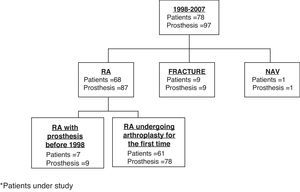
ResultsBetween January 1, 1998 and December 31, 2007, 7828 interventions of total knee arthroplasty and hip were performed in our hospital. Only 78 patients had been diagnosed with RA, of whom 17 had undergone surgery for reasons other than their underlying disease or were already carrying a total knee and/or hip replacement from before 1998. Finally, we included 61 patients with RA who underwent surgery for the first time and 78 total hip or knee replacements performed in the last decade in our hospital as a direct result of their illness. Fig. 1 shows the flow of surgical interventions and indications of all patients with RA.
Baseline clinical characteristics of patients with RA who underwent hip and/or knee as a direct result of their illness for the first time between 1998 and 2007, are shown in Table 1. As shown, 80% were women, mean age 58 years and with a long-standing disease at the time that they were given the first prosthesis. The proportion of patients with positive RF was also quite high, and 2 patients had amyloidosis. The frequency, however, of rheumatoid nodules, sicca syndrome, pulmonary fibrosis and atlantoaxial subluxation was low.
Baseline Characteristics of Patients Undergoing a First Time Knee and/or Hip Arthroplasty due to RA.
| Variables | n/No. (%)/Mean±SD (Range) |
| No. patients | 61 |
| Female | 49/61 (80%) |
| Age, years | 58±13 (20–76) |
| Time from onset of RA to first PRT, years | 13±7 (2–33) |
| Positive rheumatoid factor | 51/61 (84%) |
| Anti-cyclic citrullinated peptide | 22/54 (41%) |
| Positive ANA | 25/55 (46%) |
| Early erosions (first 6 months) | 4/35 (11%) |
| Rheumatoid nodules | 13/48 (27%) |
| Sicca syndrome | 13/48 (27%) |
| Pulmonary fibrosis | 4/48 (8%) |
| Atloaxoid subluxation | 5/43 (12%) |
| Amyloidosis | 2/48 (4% |
| Elevated ESR at onset | 32/46 (70%) |
| Elevated CRP at onset | 36/40 (90%) |
SD: standard deviation; CRP: C reactive protein; PRT: prosthesis; ESR: erythrocyte sedimentation rate.
As shown in Table 2, the majority of patients had been treated previously with at least one DMARD, mostly with methotrexate, leflunomide and sulfasalazine. Only 7 patients (11.5%) had received biological therapy prior to arthroplasty, but this proportion increased to 36% over the last decade.
Antirheumatic Treatment Employed up Until the Moment of the First Prosthesis and Localization and Total Number of Arthroplasties.
| Variables | n/No. (%)/Mean±SD (Range) |
| No. previous DMARD | 2.6±1.5 (0–6) |
| 0 | 1/40 (2.5%) |
| 1 | 8/40 (20%) |
| 2 | 14/40 (35%) |
| ≥3 | 17/40 (42.5%) |
| DMARD employed | 2.6±1.5 (0–6) |
| Methotrexate | 35/40 (88%) |
| Leflunomide | 20/40 (50%) |
| Sulfasalazine | 14/40 (35%) |
| Biologic therapy | 23/61 (38%) |
| Before the first arthroplasty | 7/61 (11.5%) |
| Mean time of use, years | 1.2±0.73 (0.4–2.6) |
| After the first arthroplasty | 16/61 (26.2%) |
| Mean time of wait, years | 3.7±2.6 (0.5–8.1) |
| Biologic therapy used as a first option | |
| Etanercept | 17/23 (74%) |
| Adalimumab | 1/23 (4%) |
| Infliximab | 5/23 (22%) |
| Localization of total arthroplaties in RA | |
| Knee | 44/61 (72%) |
| Hip | 17/61 (28%) |
| Total no. of prosthesis per patient | |
| 1 | 46/61 (75%) |
| 2 | 14/61 (23%) |
| 3 | 1/61 (2%) |
RA: rheumatoid arthritis; DMARD: disease modifying anti-rheumatic drugs.
Patients receiving biologic therapy also took a greater number of DMARDs (mean±SD: 3.6±1.7 vs 2.0±0.9, t-test, P=.001).
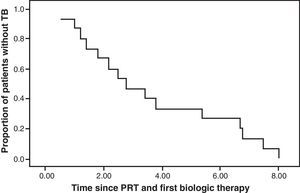
The rate of these patients’ access to the first biological therapy since the first prosthesis was placed was sequential and one third of them took more than 4 years to receive it (Fig. 2). The most widely used biologic therapy as a first option was etanercept, followed by infliximab.
Total Prosthesis PlacedTable 2 describes the location and number of replacements made. As can be seen, almost three times more knee replacements than hip were placed and three-quarters of patients only underwent arthroplasty during the study period. The time each patient remained hospitalized was variable depending on the complications suffered, but the average was 16 days.
Patients who had received biologic therapy prior to the first prosthesis tended to have lower average stays (mean±DE: 11.1±2.5 vs 16.4±7.0, t-test, P=.053).
Progression of the ProsthesisThere was no change in the total number of prosthetic interventions in our hospital per year in this decade (Cochrane Q, P=.437), nor in the number of hip replacements (Cochrane Q, P=.395). However, we did observe a downward trend in the placement of knee prosthesis as a direct result of RA in patients who were operated for the first time between 1998 and 2007 (Cochrane Q, P=.05).
There were no differences in the frequency and rate at which the prostheses were placed by gender or prior access to biological therapy.
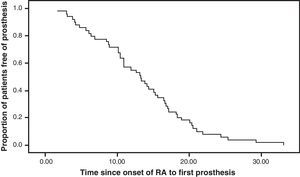
Fig. 3 shows the time from the onset of RA to the placement of the artificial joint.
DiscussionRA is a major public health problem in terms of prevalence, disability, reduction in life expectancy and quality of life. Once the damage has been established in a joint, the only treatment able to restore functionality is arthroplasty. The current antirheumatic therapies attempt to alleviate the pain and delay or prevent the deterioration of the joint. Biological therapies have been proven to inhibit joint damage with a power far superior to conventional therapies. Therefore, this should translate into a progressive reduction of the needs that patients with RA have for orthopedic surgery.
This study has been designed to analyze the frequency of surgery for hip and knee prostheses in patients with RA in our hospital during the last decade. However, our results do not suggest that there has been a significant reduction in the number of total hip placed in the last decade as a direct result of RA. We have only found a trend in reduction in the number of patients who have undergone, for the first time, total knee arthroplasty. This turnaround appears to have started in the past 5 years.
The fact that there has been a sharper reversal in arthroplasties at our institution, as might be expected, may be due to various reasons. On the one hand, most of our patients are currently being treated with methotrexate, and this treatment may be responsible for a reduction in the need for interventions since 1985, when its use was completely integrated into clinical practice. Da Silva et al.12 found this general trend toward a reduction in joint surgery in patients with RA since 1985.
Another additional reason could be that there were still a proportion of patients who agreed to replacement rather than antirheumatic therapy or were undertreated before surgery.
After 1999, the new therapeutic milestone event has been the emergence of biological therapies. Biological therapies are available in our country since then, so perhaps, given its recent introduction, we will need to spend even more time before we encounter a significant impact in reducing joint replacements, which appears to have started in 2004. However, due to the high cost of these therapies and the risks associated with their use in certain subgroups of patients, access to these drugs is not even close to that of methotrexate, so maybe its impact on the needs of orthopedic surgery in RA patients will be delayed even longer. In our study we found that patients receiving biologic therapy prior to receiving a prostheses were only seven (11.5%), and those treated after the first prosthesis 16 (26.2%), which seems a small percentage of patients taking into account the fact that they had more severe disease.
Another aspect might have influenced the methodology we have used. In our study, medical records were located through the clinical documentation service using a search strategy based on the DRG discharge reports. This approach's main weakness is that it depends on the coding being correct. However, we found no cases miscoded during the review of medical records. But even assuming that the encoding and the diagnosis has been correct in all cases, it allows us to really know the progression of prosthetic surgery rates in our patients with RA, as currently there is significant overlap in the patients treated in different hospital sectors of our province, so that a considerable number of our patients are operated on at other public or private institution and having the free choice of doctor and hospital, and the existence of coincidences between the different entities to reduce waiting lists by health administration. Alternative approaches to try to avoid these weaknesses have attempted to retrospectively or prospectively review all medical records of our patients with RA. This methodology has been used in studies like the one from Rochester, Minnesota,12 which reviewed all cases of RA between 1955 and 1995, and from there they collected every joint interventions that was made. Other studies are based on populations of patients with RA and use national registries of patients with RA.13 However, the period investigated in these studies does not include the use of biological therapies.
Another limitation of our study is its retrospective nature, as information was obtained from secondary sources, as have been the medical records of our hospital, with the limitation regarding sometimes patients and missing data having been collected by different observers, and disparity criteria in the medical records. Other studies16 where data collection was done prospectively have advantages in collecting data because it is obtained by the researcher during the observation time. This makes the data more reliable.
Finally, we highlight other aspects that may influence our results, as are the epidemiological characteristics typical of our sample. Factors such as gender seem to influence the severity of the disease. 80% of the patients in our cohort who underwent hip or knee arthroplasty were women. However, in other studies referred to above, this ratio was lower and ranged between 63% and 75%.12–14 However, these studies showed that joint surgery was more common in women, including prosthetic surgery.
The RF is another factor that decisively influences the severity of RA and 84% of our patients were RF positive. This percentage was also lower in the study by Da silva,12 who observed 56% of RF positivity, but was similar to that of Kapetanovic et al.16
The most common type of implant placed in patients who underwent a prosthesis for the first time between 1998 and 2007 was the knee prosthesis, with 44 knee prosthesis placed compared with 27 hip prosthesis, as shown by Massardo's et al.17 study, where among all arthroplasties performed as a direct result of RA, the knee was the most frequently operated on (of 146 joint arthroplasties performed, 54 were knee replacements and 31 hip replacements, who were in second place).
In conclusion, we observed no significant changes in the trend of performing total hip replacement as a whole between 1998 and 2007 in our center. The frequency of hip prosthesis has not changed, but the frequency of the number of patients requiring first time knee replacement as a direct cause of their illness may be experiencing a decline since 2004.
Please cite this article as: Manrique Arija S, et al. Tendencia anual de las artroplastias de rodilla y cadera en artritis reumatoide entre 1998–2007. Reumatol Clin. 2011;7(6):380–4.