The diagnosis of nail deformities may not be simple. Even with nail psoriasis being one of the most common onychodystrophies, it is important to recognize other common causes, such as nail biting, self-induced or traumatic causes.1
Clinical CaseThe patient is a 48-year-old woman, smoker of 20 packs/year, with a family history of psoriasis (mother and brother). She had carpal arthritis which had lasted for 9 months, with no history of inflammatory back pain, along with major onychodystrophy of the hands and a normal skin examination (Fig. 1). Analytical studies were normal or negative, including acute phase reactants, rheumatoid factor, anti-CCP and antinuclear antibodies and HLAB27. Radiographs of hands and pelvis showed no abnormalities. Treatment was started with methotrexate and a dermatologist was consulted for suspected psoriasis with nail involvement in psoriatic arthropathy. The diagnosis was “traumatic dystrophy due to onychophagia”. The patient stopped biting her nail for 6 months (Fig. 2). The response to methotrexate has been good and she has not presented arthritis. After 4 years of follow-up, the case remains an undifferentiated arthritis, with negative CASPAR criteria for psoriatic arthropathy.
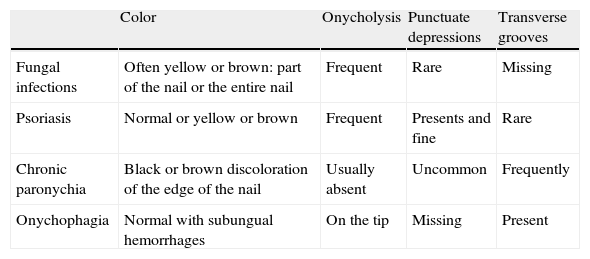
In all, 12% of patients with psoriasis have nail involvement, although the reported prevalence varies, being greater if there is joint involvement.2 The manifestations of nail psoriasis are multiple.3 The most common form is subungual hyperkeratosis, and nail pitting is the characteristic sign, although not pathognomonic, but oil spots under the nail bed can be considered very specific.4 It may be clinically indistinguishable from onychomycosis and differential diagnosis must also be made with other processes, including self-induced nail dystrophy (Table 1).
Differential Diagnosis Between the 4 most Common Diseases of the Nails.
| Color | Onycholysis | Punctuate depressions | Transverse grooves | |
| Fungal infections | Often yellow or brown: part of the nail or the entire nail | Frequent | Rare | Missing |
| Psoriasis | Normal or yellow or brown | Frequent | Presents and fine | Rare |
| Chronic paronychia | Black or brown discoloration of the edge of the nail | Usually absent | Uncommon | Frequently |
| Onychophagia | Normal with subungual hemorrhages | On the tip | Missing | Present |
Onychophagia can be explained as a compulsive habit that causes the destruction of the nails. It is a common behavior among children and young adults, although underestimated, which has received little attention in the psychiatric and dermatologic literature, but can be related to obsessive-compulsive disorders.5 Complications include superinfection, paronychia and dental problems, and phalanx osteomyelitis may occur exceptionally.6 Most patients admit onychophagia, so in nail deformities it should be one of the first direct questions we ask to exclude the diagnosis.
In our patient, because of the arthropathy, it was very important to diagnose the cause of onychopathy. If the source had been psoriasis, she would have been diagnosed with psoriatic arthropathy based on the CASPAR7 criteria. However, we showed that with willpower she could stop nail-biting for 6 months. This confirms once again the importance of the history and multidisciplinary collaboration.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that no experiments have been performed on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors declare no conflicts of interest.
Please cite this article as: Pantoja Zarza L, Díez Morrondo C, Manjón Haces JA. Artritis y onicofagia: un factor de confusión. Reumatol Clin. 2014;10:260–261.