Reports regarding the association between body composition and inflammatory activity in rheumatoid arthritis (RA) have consistently yielded contradictory results.
ObjectiveTo perform a systematic review on the association between overweight/obesity and inflammatory activity in RA.
MethodsFAST approach: Article search (Medline, EBSCO, Cochrane Library), followed by abstract retrieval, full text review and blinded assessment of methodological quality for final inclusion. Because of marked heterogeneity in statistical approach and RA activity assessment method, a meta-analysis could not be done. Results are presented as qualitative synthesis.
ResultsOne hundred and nineteen reports were found, 16 of them qualified for full text review. Eleven studies (8147 patients; n range: 37–5161) approved the methodological quality filter and were finally included. Interobserver agreement for methodological quality score (ICC: 0.93; 95% CI: 0.82–0.98; P<.001) and inclusion/rejection decision (k 1.00, P>.001) was excellent. In all reports body composition was assessed by BMI; however a marked heterogeneity was found in the method used for RA activity assessment. A significant association between BMI and RA activity was found in 6 reports having larger mean sample size: 1274 (range: 140–5161). On the other hand, this association was not found in 5 studies having lower mean sample size: 100 (range: 7–150).
ConclusionsThe modulation of RA clinical status by body fat mass is suggested because a significant association was found between BMI and inflammatory activity in those reports with a trend toward higher statistical power. The relationship between body composition and clinical activity in RA requires be approached with further studies with higher methodological quality.
Los estudios respecto a la asociación entre composición corporal y actividad inflamatoria en artritis reumatoide (AR) muestran resultados contradictorios.
ObjetivoRealizar una revisión sistemática de la literatura sobre la asociación entre sobrepeso/obesidad y nivel de actividad inflamatoria en AR.
MetodologíaEnfoque FAST: búsqueda (Medline, EBSCO, biblioteca Cochrane); revisión de resúmenes, selección para lectura en texto completo y evaluación de la calidad metodológica para inclusión. Debido a la heterogeneidad en el análisis y evaluación de la actividad de la AR, realizamos metaanálisis; los resultados se presentan como síntesis cualitativa.
ResultadosSe identificaron 119 artículos; 16 fueron revisados en texto completo. Se incluyeron 11 artículos (8.147 pacientes; rango n: 37–5.161) que aprobaron la evaluación de calidad metodológica. La concordancia interevaluador para la calidad metodológica (CCI: 0,93; IC 95%:0,82–0,98; p<0,001) y la decisión aceptación/rechazo (k 1,00, p>0,001) fueron excelentes. En todos los estudios la composición corporal se evaluó mediante IMC, pero hubo marcada heterogeneidad en la evaluación de la actividad inflamatoria. Se encontró asociación significativa entre actividad clínica y mayores valores de IMC en 6 estudios de mayor tamaño muestral promedio (1.274; rango: 140–5.161), mientras que en 5 con menor tamaño muestral promedio (100; rango: 37–150) no se encontró asociación entre actividad e IMC.
ConclusionesLa asociación entre actividad de la AR e IMC en los estudios con tendencia a mayor potencia estadística indica que la masa grasa podría modular el estado clínico en AR. El estudio de la relación entre composición corporal y actividad inflamatoria en AR requiere de más estudios y de mayor calidad metodológica.
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease that is probably of autoimmune etiology. It is characterized by inflammation and proliferation of the synovial membrane of the diarthrodial joints and, if it progresses according to its natural history, results in joint destruction, typical deformities, disability and a reduced life expectancy.1
The term “body composition” refers to the quantification of the different structural components of the human body, which can be estimated at the atomic, molecular, cellular, organ-tissue and whole body levels.2 The estimation at the organ-tissue level using variables such as body mass index (BMI), skinfold thickness, waist and hip circumferences,3 and bioelectrical impedance4 enables the assessment of the nutrition status and the determination of the organism's energy reserves and muscle mass. It also provides a valid estimate of the body fat percentage and the health risk derived from excess fat mass.
In recent decades, a series of findings has demonstrated that conditions involving excess fat mass in the body, like overweight and obesity, not only increase the risk of metabolic, neoplastic and cardiovascular diseases,5 but can be considered states of inflammatory activation, since the hypertrophic adipocytes of individuals with body compositions of these types are activated and release a number of soluble mediators known as adipocytokines or adipokines. The most important adipokines in terms of their proinflammatory activity are leptin, visfatin, interleukin 1 and tumor necrosis factor α.6,7 The latter 2 cytokines are relevant in the pathogenesis of RA, as they are crucial for the onset and persistence of the destructive synovitis that characterize this disease.8 These findings explain the interest in studying the effect of the changes in body composition characterized by excess adipose tissue on the modulation of the RA disease activity, as the confirmation of the existence of synergy between overweight or obesity and disease activity9 could justify the routine inclusion of interventions for the control and optimization of body composition as auxiliary measures in the treatment of RA patients.
However, the conclusions of reports that have evaluated the association between changes in body composition in terms of measurements of overweight or obesity and the level of disease activity in RA patients are contradictory.10,11 The reasons for this controversy very probably lie in the heterogeneity or weakness of the evaluation tools used both for body composition and the level of disease activity associated with RA, as well as weaknesses in the design and quality of the sample selection, all of which can be seen in the majority of the reports in which this question has been addressed.
Together, the above considerations indicate that, although the basic sciences provide arguments that suggest that a body composition in the excess adiposity range can modulate the clinical status of RA patients, the conclusions of clinical studies that focus on determining the influence of nutritional status on the disease activity in these patients are contradictory. For these reasons, we decided to conduct the present systematic review to evaluate the association between the presence of overweight and obesity with the level of disease activity in patients with RA.
Material and MethodsMaterialsThe present systematic review was carried out between January and June 2014. The primary data sources were articles dealing with the relationship between type of body composition and the level of disease activity in RA patients. The inclusion criteria were cross-sectional or longitudinal comparative studies involving patients with RA—defined in accordance with the 1987 criteria of the American Rheumatism Association (ARA)12 or the joint criteria of the American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) of 201013—in which an anthropometric method had been used to evaluate body composition. The studies also had to employ a validated clinical method for the determination of the level of RA disease activity, such as swollen joint count, the Ritchie articular index, the disease activity score with 28-Joint Counts (DAS 28), the Simplified Disease Activity Index (SDAI), the Clinical Disease Activity Index (CDAI), Routine Assessment of Patient Index Data (RAPID) or the Rheumatoid Arthritis Disease Activity Index (RADAI).14 Finally, reports had to present the numerical data necessary for the required analyses. We excluded review articles and studies that did not evaluate body composition or the level of disease activity in RA.
MethodsThe present study adhered to the “finding, appraisal, synthesis and transferability” (FAST) methodology,15 applying the following general guidelines:
We used the “participants, interventions, comparisons and outcomes” (PICO) approach to create the research question, which was worded as follows: in patients with RA, is overweight or obesity associated with a higher level of disease activity compared to normal or low weight?
The “finding” stage encompassed the steps involved in the search for the information and application of the selection criteria to the articles encountered in the initial search. The search focused on articles retrievable in Spanish or English from the MEDLINE, EBSCO and the Cochrane Library databases using the keywords “adipose tissue”, “BMI”, “body mass index”, “obesity”, “overweight”, “nutritional status” and “rheumatoid arthritis”. Once the search had been completed, we reviewed all the abstracts of the articles identified in order to eliminate duplicates, those that did not meet the inclusion criteria and those that did meet the exclusion criteria. The remaining articles were read and reviewed in their entirety.
The “appraisal” stage involved a blinded, independent evaluation by 2 researchers, who examined the methodological quality of the studies selected for full-text review, using an expressly designed evaluation tool, based on an adaptation of the STROBE checklist32 for comparative epidemiological studies. It consisted of items that separately assess the quality of the study, according to the design, description of material and methods, definition of the participants, description of the sample selection procedure, quality of the method used to evaluate the level of RA disease activity, and quality of the description and presentation of the results and conclusions. The final tool included 17 items with a maximum score of 14 points. The purpose of this review was to make a final decision on the inclusion only of articles that reached a minimum score for the methodological quality (11 points) and, in addition, possessed the following 4 minimum necessary components of methodological quality: a comparative longitudinal or cross-sectional design, study patients that met the ARA criteria12 or the ACR/EULAR criteria13 for the classification of RA, evaluation of the disease activity of RA using at least a swollen or tender joint count or a validated index such as DAS 28, SDAI, CDAI, RAPID or RADAI,14 and evaluation of body composition by means of some physical anthropometric method, bioelectrical impedance or dual energy X-ray absorptiometry (DXA). Once each article had been reviewed and evaluated separately, the team of reviewers was consulted to compare the methodology scores and the decisions on inclusion or rejection that had been made in the blinded, independent appraisal, in order to reach a consensus on the articles to be included, should there be any disagreement. The level of interobserver agreement in the numerical methodology score was evaluated using the intraclass correlation coefficient and the agreement regarding the decision on inclusion or rejection was determined with Cohen's κ coefficient.
AnalysisIn the “synthesis” stage, we reviewed the statistical procedures employed in the articles finally included. Our purpose was to construct a composite of the effects to establish a measure of overall effect that would enable us to perform a meta-analysis. However, because of the extreme heterogeneity in the statistical analyses and the approach to evaluating the outcome variable (measurement of RA disease activity), we were unable to identify a common effect to subject to meta-analysis. Thus, the study was detained at the level of a simple systematic review, and the findings reported in the form of qualitative synthesis and tabular data.
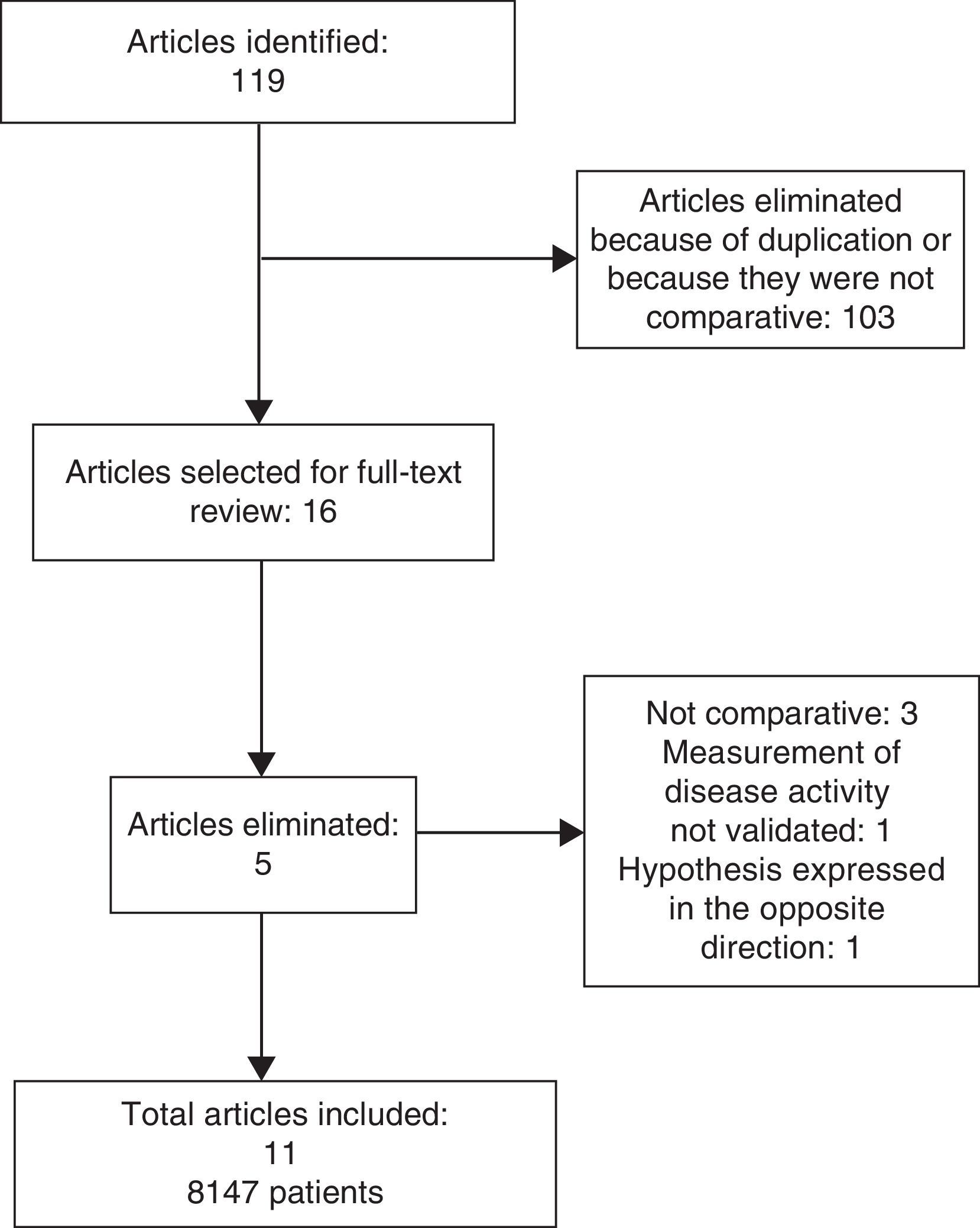
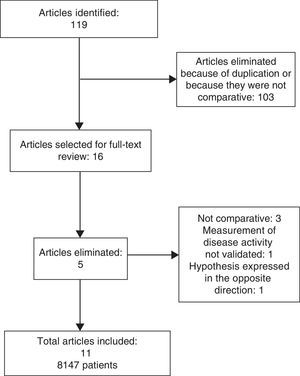
ResultsThe literature search produced 119 articles, 103 of which were eliminated after the review of the abstract, either because they were duplicates or because they had a descriptive design. Thus, we selected 16 studies for the blinded, independent review16–31 of the entire text by 2 researchers to score the methodological quality and eliminate those that did not meet the minimum required.
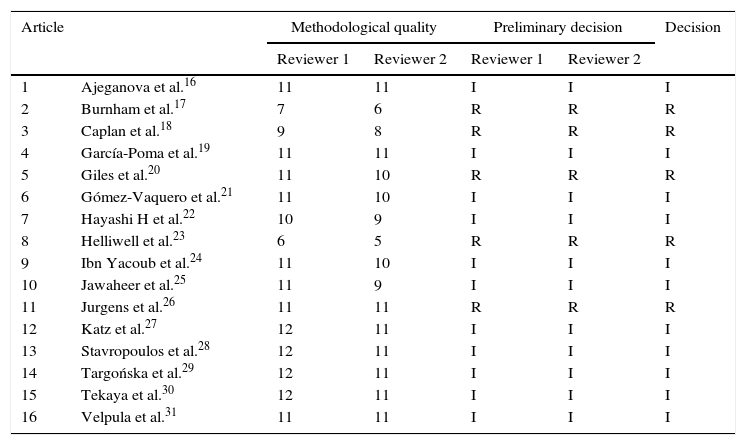
The evaluation of interobserver agreement in terms of the methodology score and the decision on inclusion or rejection is shown in Table 1. Reviewer 1 scored the 16 articles included in this phase of the study with an average of 10.73±1.53 points (range, 6–12), whereas the average score conferred by reviewer 2 was 9.93±1.66 points (range, 5–11). The result was an excellent intraclass correlation coefficient of 0.93 (95% confidence interval [CI]: 0.82–0.93; P<.001). In addition, the interobserver agreement regarding inclusion or rejection was perfect, with a Cohen's κ coefficient of 1.00 (P<.0001). Therefore, there was no need to discuss the articles to be included during this consensus session.
Results of the Scoring Process by Pairs of Researchers and Final Decision on the Inclusion of the 16 Articles Reviewed in Their Entirety.
| Article | Methodological quality | Preliminary decision | Decision | |||
|---|---|---|---|---|---|---|
| Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | |||
| 1 | Ajeganova et al.16 | 11 | 11 | I | I | I |
| 2 | Burnham et al.17 | 7 | 6 | R | R | R |
| 3 | Caplan et al.18 | 9 | 8 | R | R | R |
| 4 | García-Poma et al.19 | 11 | 11 | I | I | I |
| 5 | Giles et al.20 | 11 | 10 | R | R | R |
| 6 | Gómez-Vaquero et al.21 | 11 | 10 | I | I | I |
| 7 | Hayashi H et al.22 | 10 | 9 | I | I | I |
| 8 | Helliwell et al.23 | 6 | 5 | R | R | R |
| 9 | Ibn Yacoub et al.24 | 11 | 10 | I | I | I |
| 10 | Jawaheer et al.25 | 11 | 9 | I | I | I |
| 11 | Jurgens et al.26 | 11 | 11 | R | R | R |
| 12 | Katz et al.27 | 12 | 11 | I | I | I |
| 13 | Stavropoulos et al.28 | 12 | 11 | I | I | I |
| 14 | Targońska et al.29 | 12 | 11 | I | I | I |
| 15 | Tekaya et al.30 | 12 | 11 | I | I | I |
| 16 | Velpula et al.31 | 11 | 11 | I | I | I |
I, Inclusion; R, Rejection.
Following this consensus session concerning the definitive inclusion or rejection, 517,18,20,23,26 of the 16 articles were eliminated after the full-text examination. The main reason for the rejection of these reports was the lack of a comparison between disease activity and body composition,17,18,20 use of nonclinical or invalid indices for the measurement of RA disease activity23 or a hypothesis expressed in the opposite direction; that is, taking the disease activity as a predictor variable in regression analysis.26 Thus, the systematic review involved the remaining 11 articles.16,19,21,22,24,25,27–31 The complete sequence of the search for, analysis of and final inclusion of these publications is shown in Fig. 1.
The 11 articles ultimately included in the systematic review involved a total of 8147 patients from samples of very heterogeneous size, ranging between 37 and 5161 participants. The outcome measures for the evaluation of the level of disease activity in RA were DAS 28 in 9 studies, RADAI in 1 and swollen joint count in 1. The exposure measure for the evaluation of body composition was BMI in all 11, accompanied by skinfold thickness in 2, hip circumference in 2 and arm circumference in 1.
Given that we were unable to find a common unifying effect for the conduction of a meta-analysis, the systematic review was limited to the level of qualitative synthesis. Another aspect that impeded the performance of a meta-analysis was the heterogeneity of the statistical analyses, which involved the comparison of the mean outcome measure in numerical terms in 3 articles (using parametric, nonparametric and multivariate analysis of variance [ANOVA], respectively), whereas the statistical association was evaluated by the calculation of the correlation coefficients (Pearson or Spearman) in 5 and by simple or multiple linear correlation analysis in 3.
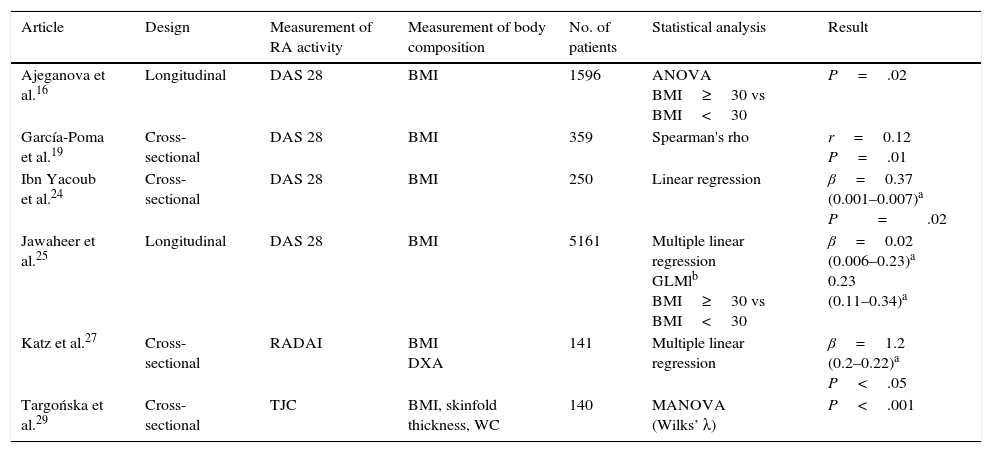
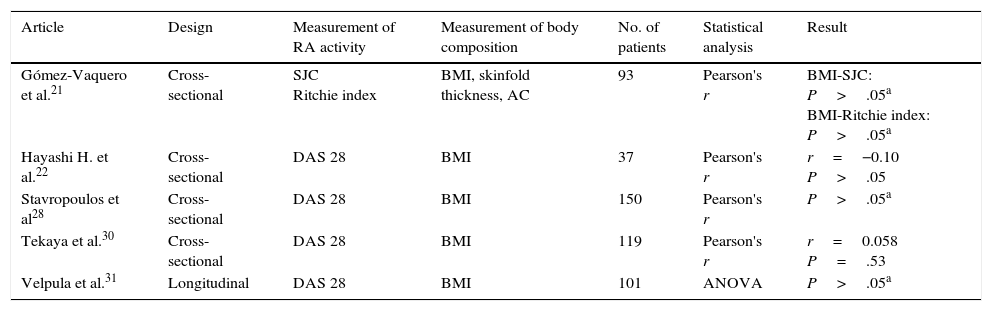
The qualitative analysis of the data revealed a significant association between a higher level of clinical activity in RA and higher BMI in 6 of the 11 studies included16,19,24,25,27,29 (Table 2), whereas, in the remaining 5 (Table 3),21,22,28,30,31 the P value for the comparison between body composition and RA disease activity was not significant. The analysis of Tables 2 and 3 showed that the 6 studies in which a significant relationship was observed between the volume of fat mass and the level of RA inflammatory tended to have larger samples (average n: 1274; range, 140–5161) in comparison with the 5 reports in which the level of significance of the analysis comparing body composition and the level of RA disease activity of did not reach statistical significance (average n: 100; range, 37–150).
Studies That Showed an Association Between Overweight/obesity and Clinical Activity in Rheumatoid Arthritis.
| Article | Design | Measurement of RA activity | Measurement of body composition | No. of patients | Statistical analysis | Result |
|---|---|---|---|---|---|---|
| Ajeganova et al.16 | Longitudinal | DAS 28 | BMI | 1596 | ANOVA BMI≥30 vs BMI<30 | P=.02 |
| García-Poma et al.19 | Cross-sectional | DAS 28 | BMI | 359 | Spearman's rho | r=0.12 P=.01 |
| Ibn Yacoub et al.24 | Cross-sectional | DAS 28 | BMI | 250 | Linear regression | β=0.37 (0.001–0.007)a P=.02 |
| Jawaheer et al.25 | Longitudinal | DAS 28 | BMI | 5161 | Multiple linear regression GLMlb BMI≥30 vs BMI<30 | β=0.02 (0.006–0.23)a 0.23 (0.11–0.34)a |
| Katz et al.27 | Cross-sectional | RADAI | BMI DXA | 141 | Multiple linear regression | β=1.2 (0.2–0.22)a P<.05 |
| Targońska et al.29 | Cross-sectional | TJC | BMI, skinfold thickness, WC | 140 | MANOVA (Wilks’ λ) | P<.001 |
ANOVA, analysis of variance; BMI, body mass index; GLM, general linear model; DAS, disease activity score; DXA, dual-energy X-ray absorptiometry; MANOVA, multivariate analysis of variance; RA, rheumatoid arthritis; RADAI: rheumatoid arthritis disease activity index; TJC, tender joint count; WC, waist circumference.
Studies That Showed no Association Between Overweight/obesity and Clinical Activity in Rheumatoid Arthritis.
| Article | Design | Measurement of RA activity | Measurement of body composition | No. of patients | Statistical analysis | Result |
|---|---|---|---|---|---|---|
| Gómez-Vaquero et al.21 | Cross-sectional | SJC Ritchie index | BMI, skinfold thickness, AC | 93 | Pearson's r | BMI-SJC: P>.05a BMI-Ritchie index: P>.05a |
| Hayashi H. et al.22 | Cross-sectional | DAS 28 | BMI | 37 | Pearson's r | r=−0.10 P>.05 |
| Stavropoulos et al28 | Cross-sectional | DAS 28 | BMI | 150 | Pearson's r | P>.05a |
| Tekaya et al.30 | Cross-sectional | DAS 28 | BMI | 119 | Pearson's r | r=0.058 P=.53 |
| Velpula et al.31 | Longitudinal | DAS 28 | BMI | 101 | ANOVA | P>.05a |
AC, arm circumference; ANOVA, analysis of variance; BMI, body mass index; DAS, disease activity score; RA, rheumatoid arthritis; SJC, swollen joint count.
The establishment of a causal relationship between an increase in the body fat mass and greater RA disease activity is important because it could result in a change in the current care model, as it would justify the inclusion in the evaluation and optimization of the type of body composition in the recommendations for the management of RA.
Previous studies that demonstrated that proinflammatory activity is a functional characteristic of states of excess adiposity,6–8 together with recent evidence showing that obesity reduces the probability of a response to biological therapies or the achievement of clinical remission,9,33 justify the study of the level of association between body fat mass and disease activity in patients with RA, However, although this subject has been dealt with in a number of reports, the conclusions are contradictory.10,11
This systematic review shows that, of the 11 articles devoted to the study of the association between excess adiposity and RA disease activity with sufficient methodological quality to be included,16,19,21,22,24,25,27–31 we found a relationship in the 6 reports that appeared to have sufficient statistical power to be included.16,19,24,25,27,29 On the other hand, we were unable to prove the existence of a statistically significant association between BMI and RA disease activity in 5 of the articles ultimately included in the systematic review.21,22,28,30,31 Our hypothesis is that the inability to detect this association in the latter reports was very probably due to a low statistical power, as their average sample size was smaller than that of the 6 articles in which this association was found to be statistically significant.
In addition to the methodological aspects, such as the design, the heterogeneity—both in the evaluation of RA disease activity and in the type of statistical analysis—and the statistical power of the study, the assessment of the association between body fat mass and the intensity of the disease activity in RA appears to be clouded by deficiencies in the methods for evaluating body composition in all the reports in which this subject is dealt with. In all the studies included in the present systematic review, the standard for the evaluation of body composition was the BMI. However, although because of its practicability and low cost, the BMI has been recommended by the World Health Organization (WHO) as the standard for the categorization of body composition and estimation of health risk on the population level,34 its application for categorizing body composition in RA patients seems to be questioned.
The so-called state of rheumatoid cachexia has an estimated prevalence in RA of between 10% and 67%, and consists of a reduction in muscle mass coinciding with an accumulation of fat tissue and normal weight or slight overweight. It can be explained by sarcopenia secondary to increased levels of proinflammatory cytokines, in addition to muscle atrophy due to disuse.35 On this basis, Stavroupulos-Kalinoglu et al. propose that the BMI may be an inaccurate measure for categorizing body composition in RA patients, at least with the cutoff points for the healthy population recommended by the WHO.10 Taking this into account, the authors suggest subtracting 2 units from the cutoff points of the values recommended by the WHO for a healthy population, if the BMI is to be used as a measure for categorizing the body composition of RA patients. In other words, in RA patients, overweight should correspond to a BMI of 23 or more and obesity, to a BMI of 28 or more. Given that the definition of overweight and obesity in all the articles included in this review was based on the WHO recommendations, it is evident that there is an underestimate of the prevalence of these 2 conditions, in addition to an inaccurate classification in the exposure groups in all the articles that approached the subject using analyses for categorical variables.
We are aware of the fact that the major limitation of the study was our inability to identify a common unifying effect that would enable us to proceed to conduct a meta-analysis. This meant that our findings can serve only for a qualitative synthesis. Moreover, our explanation in support of a possible relationship between excess adiposity and increased disease activity in RA patients is derived from the fact that the studies in which this association was demonstrated tended clearly toward a larger sample size and, thus, a greater statistical power. On the other hand, our hypothesis is that, in the 5 studies in which this association could not be confirmed, the negativity was due to the low statistical power. However, this hypothesis could not be tested either because the data presented in the other studies, with the exception of the report of Ajeganova et al., which had a statistical power of 100%,16 were insufficient for the calculation of their statistical power.
On the other hand, we consider that, given the systematic approach followed up to the point of undertaking qualitative synthesis,15 in addition to the high degree of interobserver agreement in the scoring of and decision to include the articles, the data presented in this systematic review indicate a relationship of dependency between RA disease activity and body fat mass.
In view of the fact that the 6 studies with the highest statistical power in the present systematic review indicate an association between greater fat mass, as evaluated by BMI, and greater disease activity, we conclude that there are data that indicate that the severity of disease activity in patients with RA is positively modulated by the amount of body fat mass. However, in 5 of the studies (probably subject to a type II error) in which this issue was dealt with, said association could not be demonstrated. Moreover, in all the studies, the degree of adiposity was categorized using cutoff values that very probably are not applicable to RA patients. Thus, we consider that there is still no definitive scientific evidence of an association between body fat mass and the clinical status of RA patients. Given that the refutation or corroboration of this association would have a substantial impact on the clinical management of patients with RA, we consider it necessary to stress the need for further study to correct the methodological problems that impede us from closing this important knowledge gap in the clinical care of RA patients.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Alvarez-Nemegyei J, Buenfil-Rello FA, Pacheco-Pantoja EL. Asociación entre composición corporal y actividad inflamatoria en artritis reumatoide. Una revisión sistemática. Reumatol Clin. 2016;12:190–195.