The history of ankylosing spondylitis (AS) has evolved since the first descriptions (2000 years BC), passing through the Middle Ages and, especially, the second half of the 20th century, with the discovery of HLA B27 (1973). In the fifties of the last century, there were 2 opposing schools of thought: the North American (“lumpers”) and the European (“splitters”), which considered AS to be a variant of rheumatoid arthritis (RA), or as a different entity, respectively. Then evidence arose that was favorable to their separation, grouping AS and other similar diseases as “seronegative arthritides” or “spondyloarthritides” (Moss and Wright, 1976). At the present time, we prefer calling them “spondyloarthritis” (SpA), a name that indicates its inflammatory nature.1
With respect to the diagnosis, classification tools have been appearing, from the criteria of Boland and Present (1945),2 then those of Rome (1961),3 New York (1966)4 and their modification (1984).5 Their major drawback is the limited sensitivity in the initial stages, as they require the radiographic diagnosis of sacroiliitis. To make up for these limitations, in the nineties we had the publication of the criteria of Amor6 and those of the European Spondyloarthropathy Study Group (ESSG),7 which included radiographic sacroiliitis but not as a necessary requirement, extending the diagnostic spectrum to the group of undifferentiated spondyloarthritis. Recently, the criteria of the Assessment of Spondyloarthritis International Society (ASAS) have enabled us to improve its early diagnosis, classifying SpA into 2 groups. One group is comprised of predominantly axial SpA (2009),8 which includes classical AS (radiographic sacroiliitis, meeting the modified New York criteria) and pre-radiographic or non-radiographic axial SpA (with the support of sacroiliac magnetic resonance imaging). The other consists of predominantly peripheral SpA (2011),9 including psoriatic and reactive arthritis and arthritis associated with inflammatory bowel disease and undifferentiated SpA.
Nevertheless, there are patients who cannot be classified using the new ASAS criteria, although their clinical data suggest SpA, as occurs in the following clinical setting: a 40-year-old man with a 1-year history of inflammatory low back pain, HLA B27-negative, normal levels of acute-phase reactants, good response to nonsteroidal anti-inflammatory drugs (NSAID) and 2 earlier episodes of uveitis. First-degree family history of psoriasis. Radiographs showing bilateral sacroiliitis (left, grade 2, and right, grade 1), with no MRI evidence of edema/osteitis in sacroiliac joints.
Within the group of non-radiographic “or pre-radiographic” axial spondyloarthritides (nr axSpA)10 includes those patients with a normal radiography or initial sacroiliitis, that does not meet the modified New York criteria (no AS), have MRI-evidence of edema in sacroiliac joints; however, what would occur if we found patients without edema in MRI and without radiographic damage in the sacroiliac joints? How would they be classified?
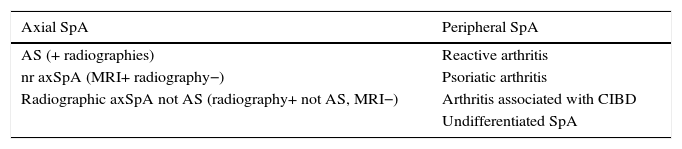
Introducing certain small changes into the nomenclature, we could speak of non-radiographic (or pre-radiographic) axial SpA in those cases in which MRI is positive for sacroiliac involvement, according to ASAS criteria, with normal radiographies or minimal changes in these joints, but do not meet the modified New York criteria. However, on the other hand, radiographic axSpA that is not AS, patients in whom there are initial radiographic changes in the sacroiliac joints (without meeting the modified New York criteria) and whose MRI is negative (Table 1).
Classification of Spondyloarthritis With the Introduction of the Concept We Refer to as Radiographic axSpA That Is not AS.
| Axial SpA | Peripheral SpA |
|---|---|
| AS (+ radiographies) | Reactive arthritis |
| nr axSpA (MRI+ radiography−) | Psoriatic arthritis |
| Radiographic axSpA not AS (radiography+ not AS, MRI−) | Arthritis associated with CIBD |
| Undifferentiated SpA |
AS, ankylosing spondylitis; CIBD, chronic inflammatory bowel disease; MRI, magnetic resonance imaging; nr axSpA, non-radiographic (or pre-radiographic) axial spondyloarthritis; radiographic axSpA no AS, radiographic axial spondyloarthritis no ankylosing spondylitis; SpA, spondyloarthritis;
In any case, studies in which the sensitivity and specificity of these modifications is evaluated are necessary. They could make it easier to achieve a better classification of those patients with incipient radiographic changes during the initial stages who have a negative MRI study.
Please cite this article as: Moreno Ramos MJ, Moreno Martinez MJ, Linares Ferrando LF. Espondiloartritis axiales: ¿se pueden clasificar todas? Reumatol Clin. 2017;13:59–60.