The giant cell tumor (GCT) is a benign primary bone neoplasm that has a locally aggressive behavior, and is rarely found in the cervical spine, where it potentially may be serious due to the risk of neurological involvement.1 Some of the affected patients may initially be evaluated by the rheumatologist due to cervical pain, the motive that brought about this clinical case.
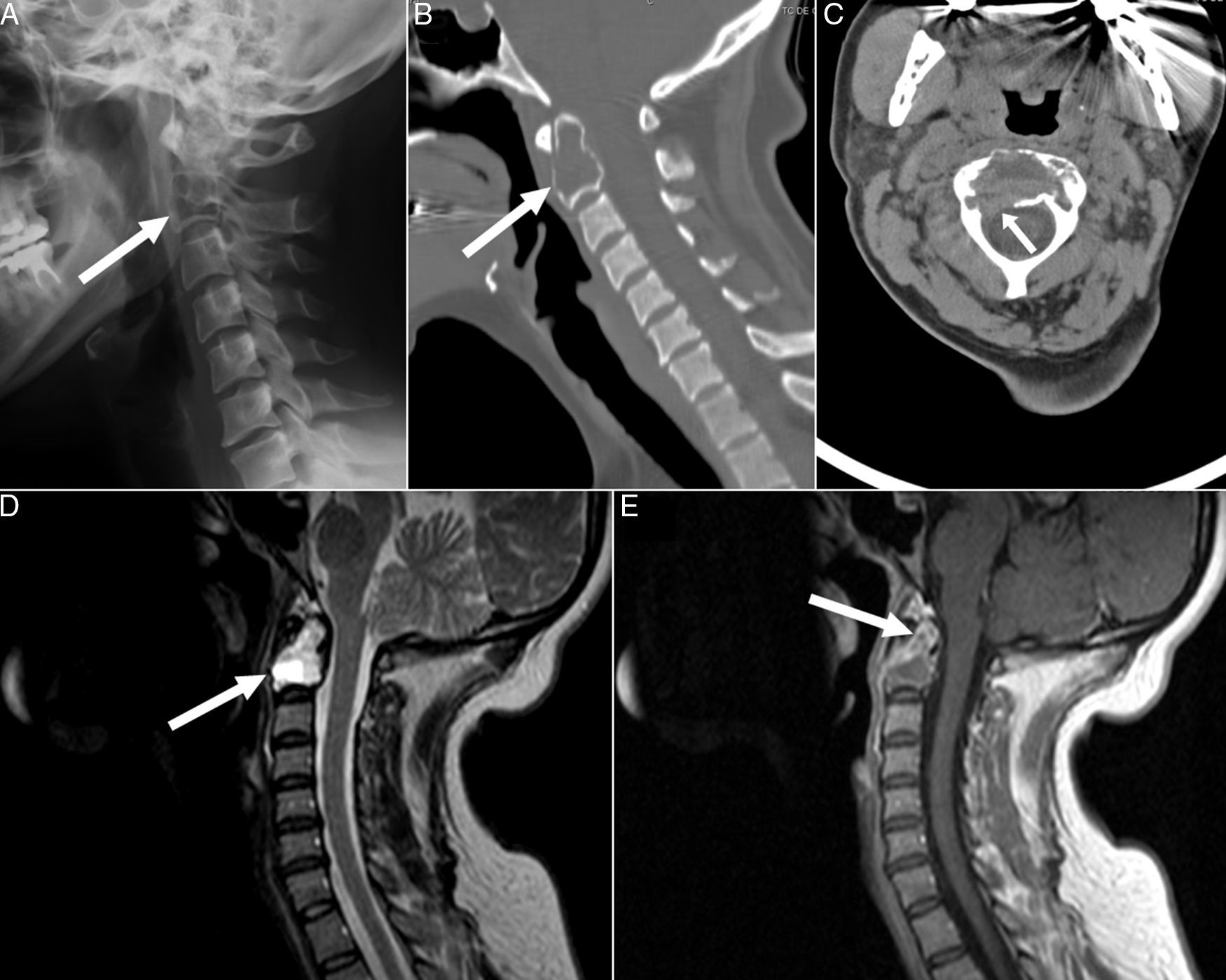
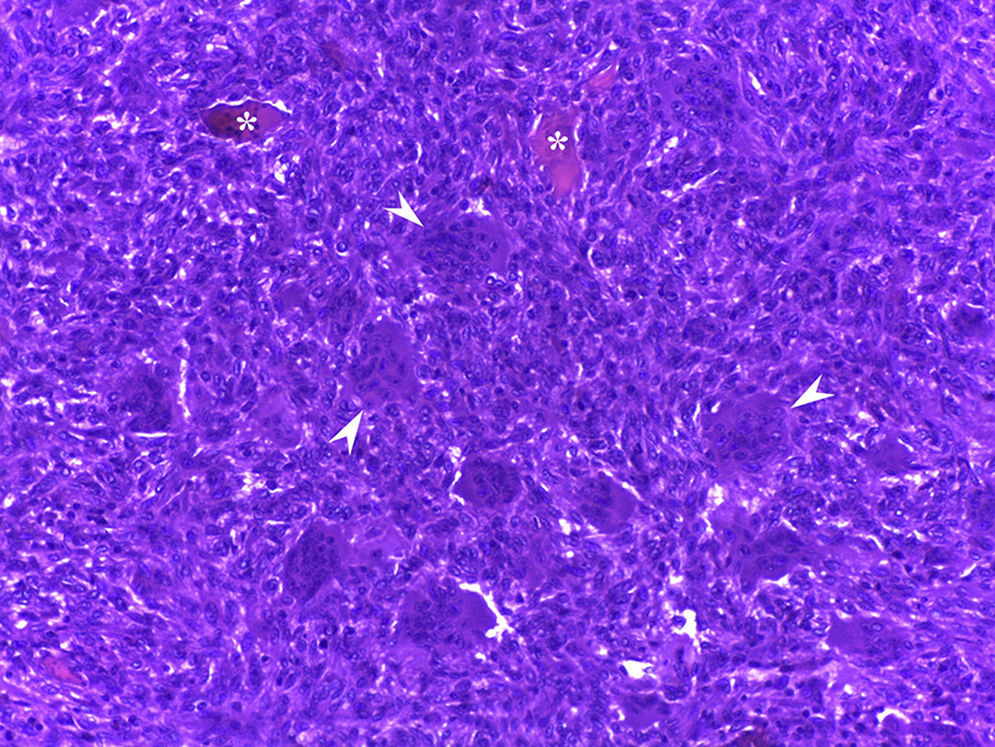
A 43-year-old, previously healthy woman presented with a sharp pain in the occipital and cervical regions with associated paresthesias in suboccipital and left retroauricular region (C2-C3 dermatomes). It had begun 9 months earlier. She was treated with analgesics, muscle relaxants and transcutaneous electrostimulation, but had noticed no improvement. Physical examination found an overall limitation to her cervical mobility and hypoesthesia in left C2-C3 dermatomes. The laboratory tests, including a complete blood count, biochemistry, acute-phase reactants (erythrocyte sedimentation rate [ESR] was 12mm/h, her C-reactive protein [CRP] 3.78mg/L), bone metabolism (Ca 8.7mg/dL, P 3.2mg/dL, 25 OH-vitamin D 39ng/mL and parathyroid hormone 44pg/mL) were normal. Lateral radiograph of the cervical spine (Fig. 1A) revealed the presence of an expansile lytic lesion occupying the C2 vertebral body. Computed tomography (CT) confirmed that the lesion totally replaced the bone marrow and interrupted the cortical (Fig. 1B and C). The lesion was hyperintense, the T2-weighted sequence of magnetic resonance imaging (MRI) reduced the caliber of the 2 holes linking C2-C3, showing areas of necrosis, fluid-fluid levels and peripheral enhancement (Fig. 1D and E). The patient was subjected to C1-C2-C3 arthrodesis due to the cervical instability caused by the lesion, which was removed using a transpharyngeal route and the defect was filled with demineralized bone matrix. The histopathological study showed a proliferation of mono- and multinucleated cells with no nuclear atypia, frequent cavities full of red cells and foci of bone neoformation and osteoid deposition. These findings were consistent with GCT or an aneurysmal bone cyst (ABC). The pain and paresthesias improved after the procedure, but these symptoms became worse 8 months later. Radiograph and CT showed recurrence of the lesion, this time with associated retropharyngeal mass. Surgery was repeated to remove the C2 using a translabiomandibular approach and occipitocervical fusion. Histopathology confirmed that the lesion was a GCT with extensions to neighboring soft tissue (Fig. 2). The patient recovered satisfactorily after the procedure, and has had no recurrences or complications after a follow-up period of 21 months.
Lateral radiograph of the cervical spine (A) showing an expansile osteolytic lesion in the vertebral body of C2 with cortical insufflation (arrow). Sagittal (B) and axial (C) planes in cervical spinal computed tomography showing that the lesion totally replaced the bone marrow (arrow) and interrupted the cortical at the right posterolateral surface of the vertebral body (arrow). Sagittal view in T2-weighted sequences (D) and in T1 after gadolinium enhancement (E) in magnetic resonance imaging of the cervical spine, which showed a cystic area, necrosis and trabeculation. The lesion was markedly hyperintense in T2 and hypointense in T1, showing peripheral enhancement after the administration of gadolinium (arrows).
Histopathology of the lesion in C2 vertebral body showing that the bone marrow has been replaced by a proliferation of round or fusiform mononuclear cells and osteoclastic-type multinucleated giant cells (arrow head). A few residual bone trabeculae can be observed among the tumor cells (asterisks) (hematoxylin and eosin, original magnification 20×).
The GCT is a benign neoplasm, characterized by the presence of osteoclastic-type multinucleated giant cells expressing CD68, that represents 4%–5% of all primary bone tumors.2 Although it can be locally aggressive, it rarely undergoes malignant transformation (approximately 2%) and it generally metastasizes to lung.3 It occurs most frequently between 20 and 40 years of age, slightly more among women and it has a predilection for the metaphyseal/epiphyseal region of the long bones.4 It affects the spine in 2.7%–6.5% of cases, but it is rarely located in the cervical spine.1,5 The most common symptoms are pain and the limited mobility, although neurological involvement is also common and occurs in up to 70% of the cases.1,5 The differential diagnosis includes other giant cell bone tumors such as ABC, simple bone cyst, chondroblastoma, osteoid osteoma, osteoblastoma, osteosarcoma, giant cell reparative granuloma and brown tumor of hyperparathyroidism.4,6 In this case, the presence of hyperparathyroidism had been ruled out, as the association between GCT and that disorder has been reported, including cases in which the cervical spine is involved.7 Up to 14% of GCT exhibit cystic components consistent with secondary ABC, but this occurs with less frequency in the cervical spine.8 The presence of osteolysis and trabeculations in imaging studies are suggestive of GCT, but the definitive diagnosis requires histopathology.7 Magnetic resonance imaging has the best sensitivity for detecting cystic components and fluid-fluid levels.7,9 The treatment is mainly surgical, in the attempt to resect the entire lesion whenever possible, especially if there may be neurological involvement.1,5,10 However, the recurrence rates are high (26%–50%).10 A number of adjuvant therapies have been utilized in the case of recurrence or inoperable lesions, including radiotherapy, selective arterial embolization, cryotherapy, argon plasma coagulation, bisphosphonates, interferon α-2b and denosumab.5,10
In conclusion, although the GCT in cervical spine is rare, it should be taken into account in the differential diagnosis of patients with neck pain and lytic lesions in vertebrae, especially when there are associated neurological signs.
Please cite this article as: Maldonado-Romero LV, Sifuentes-Giraldo WA, Martínez-Rodrigo MA, de La Puente-Bujidos C. Tumor de células gigantes vertebral: una causa rara de cervicalgia. Reumatol Clin. 2017;13:58–59.