To explore barriers to exercise of patients with spondyloarthritis (SpA) and to propose facilitators.
MethodsAnalysis of the speech of focus groups. It included the identification the elements that shape the studied reality, description of the relationship between them and synthesis through: (1) thematic segmentation, (2) categorization according to situations, relationships, opinions, feelings or others, (3) coding of the various categories and (4) interpretation of results.
ResultsTwo focus groups of 1h each with 11 patients recruited from associations and social networks in Madrid and surrounding provinces took place (64% men, 72% between 40 and 60 years, 57% with disease duration longer than 10 years, 80% performed some type of exercise or physical activity). The following were identified: (1) barriers to exercise, among which the following pointed out: disinformation, fear, pain, distrust, and prior negative experiences with exercise; (2) facilitators to exercise: the complementary to barriers plus regularity and social and professional support; (3) items that could influence in either way, negative or positively; and (4) four phases of coping with exercise or physical activity in SpA.
ConclusionApart from recognizing the existence of some modifiable personal factors, patients generally demand: more knowledge and education on exercise, including the pros and cons in the context of their disease, and coherence of messages received, together with better monitors that accompany them in their coping with disease and exercise.
Explorar las barreras que los pacientes con espondiloartritis (EsA) tienen ante el ejercicio y proponer facilitadores.
MétodosAnálisis cualitativo del discurso en grupos focales para identificar los elementos que configuran la realidad estudiada, describir las relaciones entre ellos y sintetizar el resultado mediante: 1) segmentación según criterios temáticos; 2) categorización en función de situaciones, relaciones, opiniones, sentimientos u otras; 3) codificación de las diversas categorías, y 4) interpretación de los resultados.
ResultadosSe realizaron 2 grupos focales de una hora de duración cada uno con 11 pacientes con EsA reclutados a partir de asociaciones y redes sociales en Madrid y provincias colindantes (64% hombres, 72% entre 40 y 60años y 57% con enfermedad de más de 10años; el 80% realizaba algún tipo de ejercicio o actividad física). Se identificaron: 1) barreras al ejercicio, entre las que destacaron: desinformación, miedo, dolor, desconfianza y experiencias previas negativas; 2) aspectos que facilitan la realización de ejercicio: los complementarios a las barreras más regularidad y apoyo profesional y social; 3) ítems que pueden influir tanto positiva como negativamente, y 4) cuatro fases del afrontamiento del ejercicio o actividad física en la EsA.
ConclusiónAparte de reconocer la existencia de factores personales poco modificables, en general los pacientes reclaman mayor conocimiento y educación sobre el ejercicio y sobre los pros y contras en el contexto de su enfermedad, coherencia de mensajes recibidos y mejores monitores que les acompañen en su afrontamiento frente a la enfermedad y al ejercicio.
Physical exercise is a fundamental pillar of therapy for spondyloarthritis (SpA).1,2 A review on the effects of physical activity on patients with SpA found evidence that exercise, whether supervised or at home, is better than not exercising, in order to relieve pain and improve spinal mobility, and overall evaluation on the part of the patient, although the outcome is better when it is supervised.3 The effects of exercising, supervised or done at home without supervision, are moderate but positive for function, activity, pain and mobility,4 and also improve physical condition, chest expansion and activity in SpA.5 Together with the improvement in the cardiovascular risk profile offered by physical exercise, there is a perception of increased self-care ability, a variable that is gaining in relevance in the medical treatment.6–8 There is evidence that exercise activates anti-inflammatory profiles of cytokines9 and anti-tumor necrosis factor agents increase long-term adherence to exercise in SpA patients10; this is related to the general well-being that they produce and an improvement in fatigue.11
On the other hand, teams of professionals who are responsible for the treatment of SpA patients rarely include those trained in physical activity and sports, leaving the prescription of exercise in hands of the rheumatologists.12 A survey distributed to 106 rheumatologists on the role of exercise in SpA, and in other rheumatic diseases, found that more than 86% of those specialists consider that their patients with SpA need to exercise, and that a similar number recommend it. They feel that they fail to prescribe it properly, and that one of the reasons is that they consider that they need more training for the prescription of specific exercises. They recognize that exercise should be prescribed in accordance with the underlying disease, and most agree that the intensity should be decreased during disease flares. However, when it comes time to prescribe exercise, their confidence is low.12
As occurs with medication, there is a dose–response relationship in the effect of exercise on the patient,13,14 and the prescription and follow-up of exercise should be as specific and precise as they are for drug therapy.15 Moreover, adherence is critical, and is always evaluated in clinical trials involving physical activity as a measurement of the effectiveness of this approach.
Knowledge of the possible barriers to and facilitators of exercising on the part of SpA patients is essential for the design of successful specific programs. Thus, the purpose of this study was to explore the barriers to exercise encountered by SpA patients and to propose facilitators.
MethodsWe employed a qualitative methodology for this study. The protocol was approved by the research ethics committee of Hospital Universitario Fundación Alcorcón, in the city of Alcorcón, 13km south of Madrid.
Design and Procedure for Establishing the Focus GroupsGiven the exploratory and multidimensional nature of the objective of the study, we considered the formation of focus groups to be the most appropriate technique. A typological framework was prepared to identify the profiles of the participants that would ensure a diversity of views. It included sex (a larger proportion of men than women), disease duration (at least 2 patients less than 5 years), age (at least 2 under 40 years) and a variety of occupations (active, retired, pensioners and persons who had never worked). To recruit the participants, we contacted the Spanish spondylitis coordinator (Coordinadora Española de Asociaciones de Espondiloartritis [CEADE]) and the Spanish League Against Rheumatism (Liga Reumatológica Española [LIRE]). The latter, in turn, contacted with local spondylitis associations, who ultimately got the volunteers in touch with the team. Prior to the formation of discussion groups, the patients signed a standard confidentiality document that explained that the conversation would be taped and that the data would, in addition, be published.
Each of the focus groups had a minimum duration of 1h, which could be prolonged to up to 2h if necessary, depending on the discourse. They were held for 2 consecutive days, in rooms that provided the usual requirements for groups of this type, with a neutral setting in terms of structural and symbolic matters. The interviewers were trained in qualitative methodology and followed an outline that reproduced the terms of the argument map. The gathering of information was over when the discourse had become saturated, that is, any further comments were redundant and offered nothing new. The discourse was taped and was later analyzed in terms of semiology with the aid of the Mind Manager© program.
Discussion ScriptThe group discussion outline was prepared on the basis of a systematic review of factors that improve adherence to exercise in patients with rheumatic diseases (manuscript in preparation), and the survey for rheumatologists dealing with the role of exercise in SpA and in other rheumatic diseases.11 The review revealed controversy concerning demographic factors related to adherence and, consistently, to the importance of intrinsic and motivation factors.
While the groups were being configured, information was being gathered on the following aspects: (a) typology of exercises performed by the participants and what they understand to be physical activity, exercise and sport; (b) phases of coping with exercise or physical activity in SpA; (c) aspects that facilitate exercising; and (d) potential barriers.
Data AnalysisThe data were analyzed thematically with the help of the Mind Manager© program. The analysis consisted in identifying the elements that constituted the reality being studied, describing the relationships among them and summarizing the outcome by means of: (1) segmentation according to thematic criteria; (2) categorization depending on situations, relationships, opinions, feelings or some other grouping; (3) coding of the different categories, including (a) barriers, (b) facilitators and (c) other differing factors; and (4) interpretation of the results.
ResultsHere we provide the outcome of the discourse analysis. The verbatim comments of the participants were included as supplementary material, as examples, and are identified in the text by V and successively numbered. In this case, as there are few patients, we preferred not to identify them by using initials or with descriptors.
Participant ProfilesWe recruited 11 patients among the 2 groups with the following profiles: 7 (64%) men, with ages between 30 and 70 years; 6 of them (57%) had a history of SpA of over 10 years. In all, 80% did some type of exercise or physical activity: either sports (swimming and biking), some type of gymnastics (yoga, Pilates, stretching, circuit training at home, etc.) and/or physical activity (brisk walking, jogging, running, dancing, biking, walking the dog).
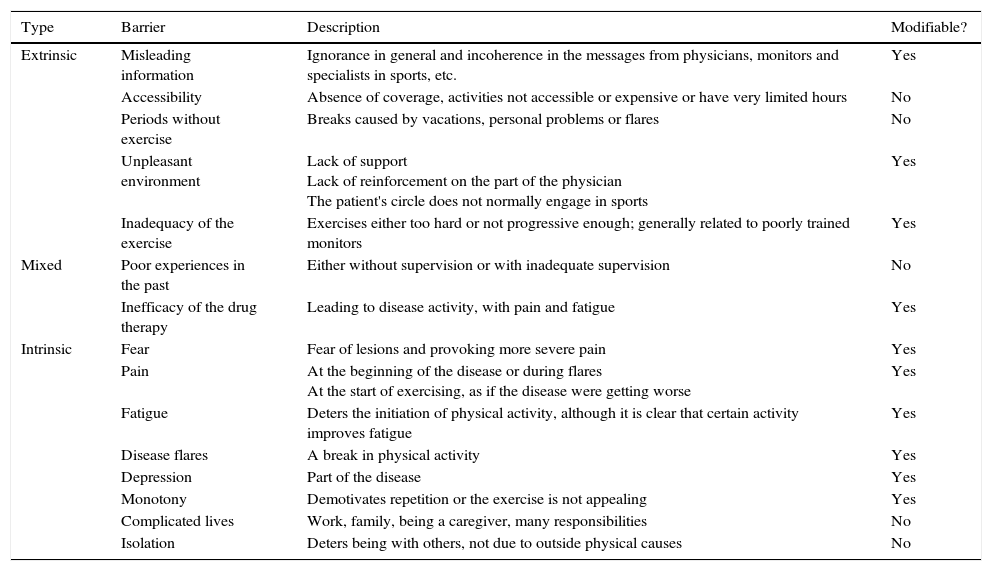
Barriers to Physical ExerciseThe barriers included intrinsic and extrinsic barriers; each was assessed a posteriori to determine whether or not it could be modified from the outside (Table 1).
Barriers to Exercising in Spondyloarthritis.
| Type | Barrier | Description | Modifiable? |
|---|---|---|---|
| Extrinsic | Misleading information | Ignorance in general and incoherence in the messages from physicians, monitors and specialists in sports, etc. | Yes |
| Accessibility | Absence of coverage, activities not accessible or expensive or have very limited hours | No | |
| Periods without exercise | Breaks caused by vacations, personal problems or flares | No | |
| Unpleasant environment | Lack of support Lack of reinforcement on the part of the physician The patient's circle does not normally engage in sports | Yes | |
| Inadequacy of the exercise | Exercises either too hard or not progressive enough; generally related to poorly trained monitors | Yes | |
| Mixed | Poor experiences in the past | Either without supervision or with inadequate supervision | No |
| Inefficacy of the drug therapy | Leading to disease activity, with pain and fatigue | Yes | |
| Intrinsic | Fear | Fear of lesions and provoking more severe pain | Yes |
| Pain | At the beginning of the disease or during flares At the start of exercising, as if the disease were getting worse | Yes | |
| Fatigue | Deters the initiation of physical activity, although it is clear that certain activity improves fatigue | Yes | |
| Disease flares | A break in physical activity | Yes | |
| Depression | Part of the disease | Yes | |
| Monotony | Demotivates repetition or the exercise is not appealing | Yes | |
| Complicated lives | Work, family, being a caregiver, many responsibilities | No | |
| Isolation | Deters being with others, not due to outside physical causes | No |
Fear of injury and of provoking more severe pain was repeatedly identified as one of the major intrinsic obstacles for performing physical exercise encountered by the patients. Pain comes to be a factor that affects them in their activities of daily living and, thus, exercising is not one of their priorities.
In general, disease activity, either as flares, fatigue or even depression, is identified as an intrinsic barrier. In fact, the inefficacy of drug therapy was seen per se as a barrier that led to the above events, although, in this case, it was considered an extrinsic barrier.
Previous negative experiences involving exercise are also an inconvenience for attempting it again. In most cases, these incidents included exercising or playing sports without supervision. This resulted in the patients being injured due to their lack of knowledge of the exercises that were most suitable for them; on some occasions, the negative experiences were associated with undertaking exercise routines that were not dosed in accordance with the individual's capacities (VI).
Within the extrinsic barriers, we point out the lack of coverage (accessibility) with interventions appropriate for the changing physical condition of the patients, or the unawareness of the existence of this circumstance. Some allude to the need to engage a good monitor to design an exercise plan in accordance with the situation and the preferences of each patient, and that ensures that the patient will not be hurt (V2).
On the other hand, the inclusion of exercise in the daily routine is complicated, and even more so, in the case of patients who feel alone and are often in a setting that is not favorable for exercising. This can occur because of the extrinsic barriers mentioned above, or because the people in the patient's circle do not regularly get involved in physical activity or sports. Those periods in which exercise is left “on hold”, either because of a disease flare, personal problems or vacations, make it difficult to maintain a routine, and motivation is discouraged. In this case, the cause would be a combination, or mixture, of extrinsic and intrinsic factors (V3).
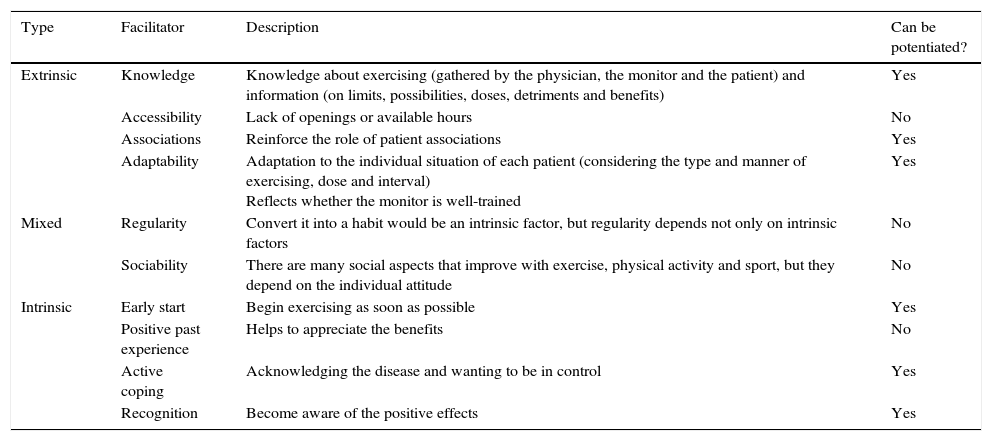
Facilitators of Physical ExerciseWe identified several facilitators of physical exercise, again classifiable as extrinsic and intrinsic (Table 2). On the one hand, extrinsic aspects were mentioned repeatedly in patient input. Knowledge, on the part of both the professional physician who provides guidelines for exercise, and that of the monitor who designs the work plan, seems to be a positive factor when it comes to this approach. Having a good monitor who adapts the exercises to the characteristics of each patient appears to be essential (V4).
Facilitators for Exercising in Spondyloarthritis.
| Type | Facilitator | Description | Can be potentiated? |
|---|---|---|---|
| Extrinsic | Knowledge | Knowledge about exercising (gathered by the physician, the monitor and the patient) and information (on limits, possibilities, doses, detriments and benefits) | Yes |
| Accessibility | Lack of openings or available hours | No | |
| Associations | Reinforce the role of patient associations | Yes | |
| Adaptability | Adaptation to the individual situation of each patient (considering the type and manner of exercising, dose and interval) Reflects whether the monitor is well-trained | Yes | |
| Mixed | Regularity | Convert it into a habit would be an intrinsic factor, but regularity depends not only on intrinsic factors | No |
| Sociability | There are many social aspects that improve with exercise, physical activity and sport, but they depend on the individual attitude | No | |
| Intrinsic | Early start | Begin exercising as soon as possible | Yes |
| Positive past experience | Helps to appreciate the benefits | No | |
| Active coping | Acknowledging the disease and wanting to be in control | Yes | |
| Recognition | Become aware of the positive effects | Yes |
Regarding knowledge, information has been identified as a key aspect. In general, patients considered that their physicians were not well-informed about exercise and the sports they could or could not participate in. Therefore, the latter did not inform the patients, or were unable to respond to their doubts.
On the other hand, patients showed that, to achieve good adherence, the crucial aspects were accessibility in terms of proximity, hours compatible with their workday and the quality of sports facilities (V5).
Regularity is an intrinsic–extrinsic factor (depending on the arguments employed) that is clearly identified as a facilitator (V6).
Finally, the social aspects of exercise were pointed out, as a way of forgetting about their disease and as a diversion (V7).
Concerning the intrinsic factors, the patients stated that active coping with the disease was a key facilitator for engaging in physical exercise (V8).
Starting to exercise right after receiving the diagnosis of SpA is also a facilitator. It makes it easier to include it in the daily routine and, above all, maintain it over the long term (V9).
Another factor that was pointed out was a good experience with exercising in the past. Those patients who had participated in some type of sport prior to the diagnosis found it easier to continue to do so, as they themselves knew the benefits of it (V10).
The Role of AssociationsOne of the groups identified an unexpected facilitator, that actually encompasses many of the facilitators, reinforcing the role of associations in facilitating exercise (V11).
One of the groups pointed out that, aside from providing companionship and the experience of others in the same situation, the associations can serve as a vehicle for a great deal of information. This information should deal with limits to exercising, especially in the initial phases of the disease, as well as the most appropriate types of exercise, the amounts, and the accompanying benefits and problems. On the other hand, associations can improve the access of patients to exercise and potentiate or facilitate regular exercising. The training of specialized monitors was even proposed to make use of the experience of the associations of patients in the design and adaptation of exercise programs (V12).
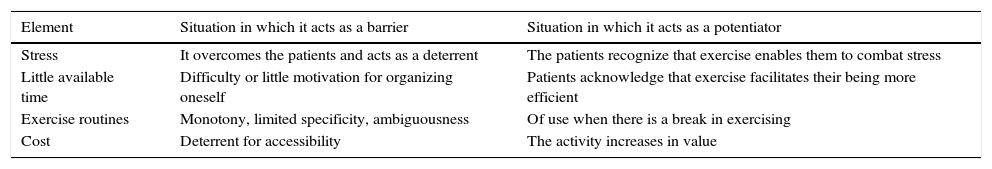
Conflicting ElementsFinally, there were certain elements that aroused contrasting opinions among the individuals participating in the focus groups (Table 3).
Conflicting Elements That Can Be a Barrier or a Facilitator Depending on the Individual.
| Element | Situation in which it acts as a barrier | Situation in which it acts as a potentiator |
|---|---|---|
| Stress | It overcomes the patients and acts as a deterrent | The patients recognize that exercise enables them to combat stress |
| Little available time | Difficulty or little motivation for organizing oneself | Patients acknowledge that exercise facilitates their being more efficient |
| Exercise routines | Monotony, limited specificity, ambiguousness | Of use when there is a break in exercising |
| Cost | Deterrent for accessibility | The activity increases in value |
Certain patients are overcome by the stress created by the situation and end up abandoning exercise, while others see it as a mode of getting away and increase the intensity (V13).
Finding the time is also a conflicting element. Regular physical exercise is difficult to reconcile with the vicissitudes of daily living for some patients. However, others acknowledge that the time utilized in exercising is gained through efficiency in other duties. The motivations of each individual and past experiences with exercise come in to play here (V14).
On occasion, health professionals prescribe exercise routines. Aspects like monotony, limited specificity or ambiguousness of the tables were comments from the participants and, in terms of their utility, if they are good, they can serve for moments when exercise is “on hold” (V15).
The cost of the activities can potentiate and, at times, is a restraint, provided we are talking about reasonable prices. Greater quality in exercising will always be accompanied by higher costs (V16).
Phases of Coping With Exercise or Physical Activity in SpondyloarthritisFour phases of coping with exercise or physical activity have been identified in patients with SpA. In the first phase, at the commencement of the disease, patients are fearful after the medical diagnosis, probably due to the enormous amount of information they receive. We found 2 attitudes in the patients: those who refuse to exercise (V17) and those who decide to start participating in physical activity on their own. During this phase, patients are receptive and can understand that exercise has positive effects if things are explained well. That is the time to incorporate beneficial routines and, thus, information and support on the part of the person prescribing exercise will be critical elements to get patients involved in their own care (V18).
In a second phase, there can be 2 profiles: patients who, in general, see few results of the treatment, or those who see that, in them, the disease does not appear to be so severe, or who receive little reinforcement on the part of their attending physician, and stop exercising “You become over-confident and start loafing”; and those who continue to look on their own, or in patient associations, on how best to progress or adapt exercise to their disease.
In a third phase, which we can call the expert patient. These persons know what exercise implies, both in terms of its effect and in logistics. Again, there are 2 postures: that of relaxation and giving up, and that of active coping (V19). In this phase, health care professionals have little to say.
Finally, the fourth phase involves disease flares, although, in reality, they can develop at any time. Flares act like a trigger, or an opportunity, for engaging in exercise; patients mention that they become totally conscious of the utility of maintaining themselves active (V20).
DiscussionThis study recalls the discussion between SpA patients concerning the evaluation of their opinion on physical exercise and their suggestions on how to improve adherence to it. The main objective of qualitative methodology is not to empirically demonstrate the facts, but to analyze and interpret the thinking, motivation and behaviors linked to those facts. This exploratory exercise has enabled us to propose several elements that we should take into account when prescribing exercise to patients with SpA. However, it is important to make it clear that, although we have identified both barriers and facilitating elements, we have not measured the individual importance of each.
In general, the elements identified coincide with those indicated in previous studies. Above all, it is noteworthy that psychological factors are more evident than physical or objectified aspects; they include the levels of motivation and self-efficacy, time or its scarcity, our limited familiarity with exercise and the little social and cultural support.16,17
Moreover, we see that, although they are psychological, many are perfectly modifiable. For example, we demonstrated the importance of information, of confidence in oneself and in the specialists, and of fear. It could be that the intervention should be done, but rather than in patients, in rheumatologists, who will ultimately prescribe the patients’ regimens and perform the follow-up. If rheumatologists feel comfortable with what they prescribe because they are familiar with it, it is more probable that they devote more time to the patients during their visits and carry out the follow-up.12 Rheumatologists should be able to explain, or refer patients to where they will find a good explanation, of the benefits of exercise, banishing fears (their own and those of the patients) and responding to doubts about which exercises to perform, how to proceed and how to adapt them to the needs of patients.
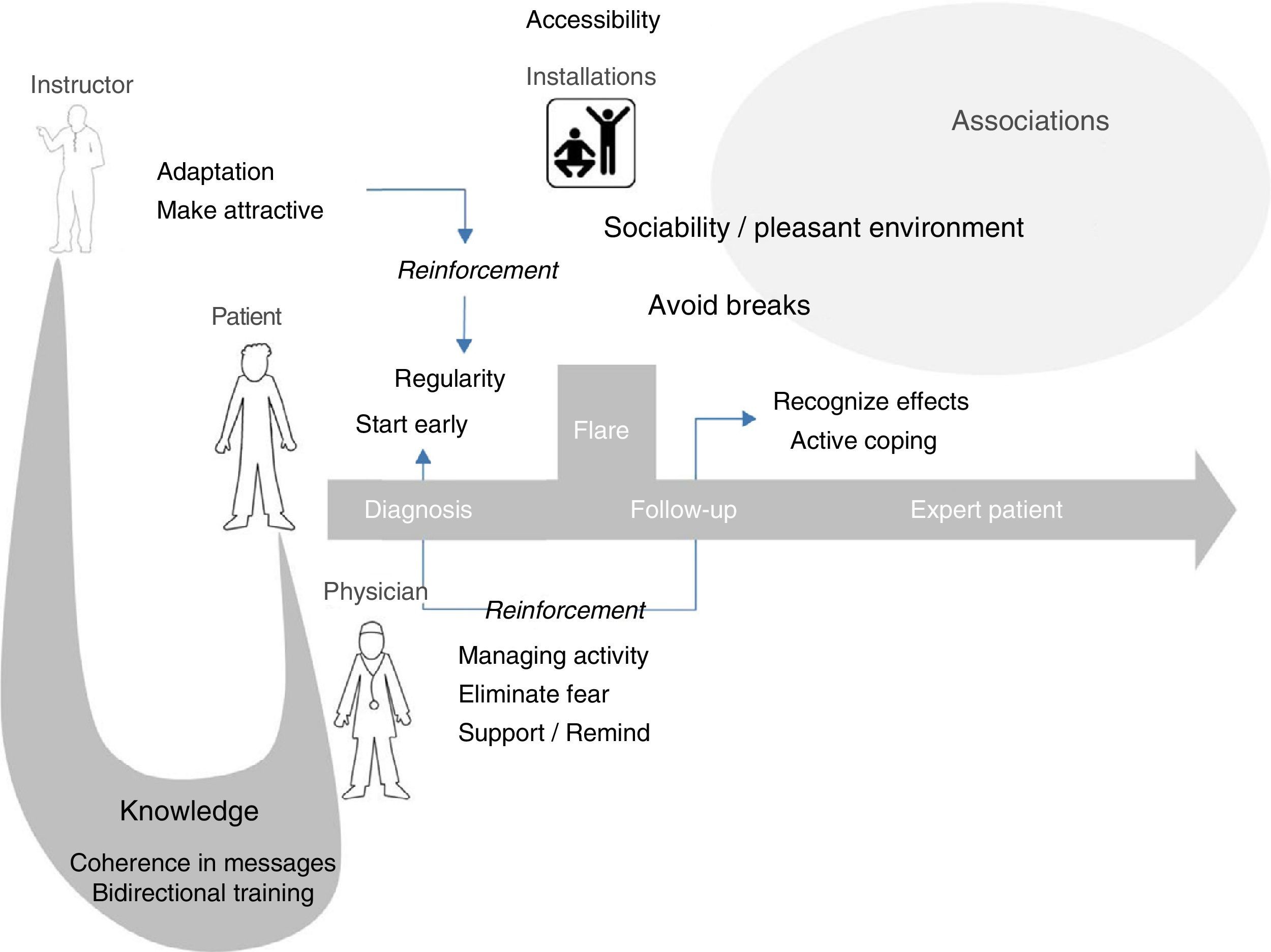
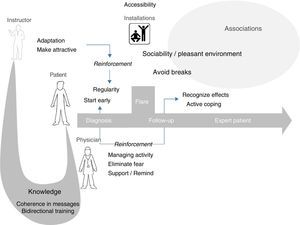
Fig. 1 attempts to summarize the different interrelationships that favored exercise in this model. So this can all begin, the knowledge of exercise specialists should be shared with rheumatologists, who must, in turn, educate patients. This education can be indirect, through other professionals or web pages, but they must at least prescribe that education. Rheumatologists must also reinforce, support and eliminate fears of patients concerning exercise. It is also the role of instructors, or specialists in exercise, to make exercise attractive and adapt it to the situation and physical condition of patients; they must be familiar with the disease diagnosed in the persons who are to receive his or her instruction in physical activity and sports. We have attempted to reflect the role of patient associations supporting access to atmospheres that favor participation.
Hypothetical model of exercise reinforcement in spondyloarthritis. Exercise specialists should share their knowledge on exercise with rheumatologists, who must, in turn, share it with their patients. The role of instructors is to make exercise attractive and adapt it to the physical condition and activity of the patients, information that they should receive from the rheumatologists. The latter should do all they can to manage their patients’ disease and eliminate their fears of exercise, giving them encouragement and reminding them that it is necessary. Patients should begin immediately and make it a habit as soon as possible, with an attitude of active coping. Sports facilities should be accessible and provide atmospheres that favor participation. Patient associations could promote both, and serve as a platform for instructor training.
Patients have access to a wide variety of specialists which, in general, are limited. They are often monitors with a minimum of training, and only in a specific technique, not in its impact, a fact that exercise specialists should be aware of. However, they do not have much information on diseases. We think that the solution proposed by the groups to count on patient associations for the training of monitors, physical therapists or exercise specialists is especially useful.
In general, the utilization of the pros and cons of exercising in our arguments to reinforce patients should improve adherence, on one hand, and health outcomes on the other. Nevertheless, this should be confirmed in an intervention study, not using a qualitative design.
The multidimensional nature of adherence makes it difficult to study. An important element in the decision to exercise is the individual determination and training it involves.18 On occasion, patients request home physiotherapy. At times of increased disease activity, home care has come to be understood as being an element of marginal benefit. It does not achieve the knowledge/training in an independent display of patients in their relationship to physical exercise.19 Thus, we should be capable of transferring to patients the knowledge they need for it to be beneficial, and not doing it in its place.
In short, aside from acknowledging the existence of personal factors that are not easy to modify, in general, patients demand greater knowledge on the part of their physicians, and education on the pros and cons of exercise in the context of their disease, coherence in the messages received and better monitors accompanying them in their coping with the disease and exercise. The associations are a vehicle for a great deal of information, aside from providing companionship and the past experience of others.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe present study was financed by Merck Sharp & Dohme de España.
Conflicts of InterestThe authors declare they have no conflicts of interest concerning the research topic.
The authors wish to sincerely thank the participants in the focus groups, who unselfishly contributed to our knowledge of this singular reality. We also thank the Liga Reumatológica Española (LIRE) for allowing us the use of their installations for the groups and the Coordinadora Española de Asociaciones de Espondiloartritis (CEADE) for recruiting the participants.
Please cite this article as: Curbelo Rodríguez R, Zarco Montejo P, Almodóvar González R, Flórez García M, Carmona Ortells L. Barreras y facilitadores para la práctica del ejercicio físico en pacientes con espondiloartritis: estudio cualitativo de grupos focales (EJES-3D). Reumatol Clin. 2017;13:91–96.