To describe (structure, processes) of the multidisciplinary care models in psoriatic arthritis (PsA) in Spain, as well as barriers and facilitators of their implementation.
MethodsA qualitative study was performed following structured interviews with 24 professionals (12 rheumatologists, 12 dermatologists who provide multidisciplinary care for patients with PsA). We collected data related to the hospital, department, population and multidisciplinary care model (type, physical and human resources, professional requirements, objectives, referral criteria, agendas, protocols, responsibilities, decision-making, research and education, clinical sessions, development and planning of the model, advantages and disadvantages of the model, barriers and facilitators in the implementation of the model). The models characteristics are described.
ResultsWe analyzed 12 multidisciplinary care models in PsA, with at least 1–2 years of experience, and 3 subtypes of models, face-to-face, parallel, and preferential circuit. All are adapted to the hospital and professionals characteristics. A proper implementation planning is essential. The involvement and empathy between professionals and an access and well-defined referral criteria are important facilitators in the implementation of a model. The management of agendas and data collection to measure the multidisciplinary care models health outcomes are the main barriers.
ConclusionsThere are different multidisciplinary care models in PsA that can improve patient outcomes, system efficiency and collaboration between specialists.
Describir la estructura y procesos de distintos modelos de atención multidisciplinar de pacientes con artritis psoriásica (APs) en España, así como las barreras y facilitadores en su implantación.
MétodosSe realizó un estudio cualitativo mediante entrevistas estructuradas a 24 profesionales (12 reumatólogos y 12 dermatólogos que realizan atención multidisciplinar en pacientes con APs). Se recogieron datos relacionados con el centro, servicio, población atendida y sobre el modelo de atención multidisciplinar (tipo, recursos materiales y humanos, requerimientos de los profesionales, objetivos, criterios de entrada y salida, agendas, protocolos de actuación, responsabilidades, toma de decisiones, actividad investigadora y docente, sesiones clínicas conjuntas, creación/inicio, planificación, ventajas/desventajas del modelo y barreras/facilitadores en la implantación del modelo. Se describen sus características.
ResultadosAnalizamos 12 modelos de atención multidisciplinar en APs, implantados desde hace al menos 1-2años, que globalmente pueden resumirse en 3 subtipos diferentes: presencial conjunto, presencial paralelo y circuito preferencial. La implantación de uno u otro modelo es consecuencia de la adaptación a las circunstancias del centro y profesionales. Una correcta planificación de la implantación es fundamental. La implicación y buena sintonía entre profesionales así como un acceso y criterios de derivación bien definidos son facilitadores muy importantes en la implantación de un modelo. La gestión de las agendas y la recogida de datos para medir resultados de salud de estos modelos son las principales barreras.
ConclusionesExisten distintos modelos de atención multidisciplinar implantados que tienen como objetivo intentar mejorar la atención del paciente con APs, la eficiencia del sistema y la colaboración entre especialistas.
Psoriatic arthritis (PsA) is a potentially severe, chronic, progressive, multiorgan disease. Patients should be properly and indefinitely evaluated from the first visit.1–4 Many of them are studied by dermatologists and rheumatologists separately, meaning that the care process may not be optimal from a clinical perspective, and is not ideal for the patient, or even for the system.5–7
On the other hand, the 2012 recommendations of the European League Against Rheumatism (EULAR) propose a multidisciplinary approach in PsA,8 as do expert groups and patients.9 Thus, in recent years, dermatologists and rheumatologists have teamed together to introduce multidisciplinary units to treat PsA patients.10,11 Now that they have been established, it is essential that their activity be evaluated to demonstrate their efficacy and pinpoint areas for improvement. Moreover, their experience can serve other professionals interested in introducing a multidisciplinary strategy in their management of these patients.
One of these units, in which both a rheumatologist and a dermatologist see patients jointly and in collaboration, recently reported their 4-year experience.10 During this period, they received a total of 259 visits (71% first appointments). Joint visits resulted in a change in diagnosis in 1 third of the patients, and a therapeutic change in nearly half of those cases. Aside from the aforementioned impact on care, the introduction of this multidisciplinary model in patients with PsA led to an increase in the collaboration between the 2 specialties, and has been exported to other Spanish hospitals.
Taking the above into account, the objective of the NEXUS project, which includes the work described in that first report, was to promote and standardize multidisciplinary care in PsA patients being provided in Spain. The work presented here constitutes the first objective of the NEXUS project and consists in depicting the different features of the multidisciplinary care model in this country, as well as the barriers and facilitators involved in introducing it. This could serve as a guideline for those professionals who would like to undertake multidisciplinary care in patients with PsA, and for the subsequent development of quality standards and indicators.
Material and MethodsStudy DesignThe study was designed to characterize the different multidisciplinary care units currently functioning in Spain, including the barriers and facilitators associated with their introduction. This work is part of the NEXUS project, an undertaking with the participation of the Spondyloarthropathy Study Group of the Spanish Society of Rheumatology (GRESSER), the Spanish Group on Psoriatic Arthritis (GEAPSO) and the Spanish Academy of Dermatology and Venereology (AEDV). Their main objective is to produce quality standards and indicators for multidisciplinary care of the PsA patient. This project was developed in different phases that included a meeting of a nominal group of experts, a systematic literature review and, ultimately, structured telephone interviews.
Nominal Group Meeting and Literature ReviewIn a nominal group meeting, with a total of 24 professionals (12 rheumatologists and 12 dermatologists who were involved in multidisciplinary care of PsA patients), the subject was the different models, and the variables that should be brought together to describe these models. The participants were selected on the basis of their experience and interest in the topic being studied (this included a Medline search to locate professionals with publications in this area, who were asked about other professionals who might participate in the project). In the selection, the geographic representativeness was taken into account, and the professionals had to come from both large hospitals and from smaller centers, as well. A literature search on models of multidisciplinary care in PsA was conducted.
Structured Telephone Interviews and Variables GatheredUsing the information obtained in the literature review and in the nominal group meeting, a specific outline was designed to collect data on the different models of multidisciplinary care provided in Spain. Teleconferences enabled us to contact members of the multidisciplinary units and interview them (jointly when possible). We had sent a summary of the outline so that the interviewee could prepare the necessary data and responses. The following variables were collected: (a) related to the workplace, including hospital level, city, reference population, distribution of the population attended to (% urban, % rural) and computer literacy; (b) regarding the department, such as the organizational structure (unit, service, section), PsA patient care (hospital or ambulatory, or both), and the number of physicians on the staff; (c) related to multidisciplinary care and the model employed, including material resources (office, equipment, etc.), human resources (specialists, nursing, etc.), qualifications of the professionals (training, interest in those affected, etc.), definition of objectives, criteria for access and discharge (document authorizing referral from or to another department, a form on paper, etc.), development of the agenda, activity protocol (diagnosis, follow-up, treatment), the evaluation of the outcome (recording clinical data, administrative tasks, costs, of the unit itself, etc.), defining responsibilities, decision making, research or teaching, joint clinical meetings, creation/initiation (evaluation of needs of the center/health area and resources, contacts among specialties, hospital management, information, distribution to the different departments, specific training), strategies for introducing an innovative measure, leadership, planning, service portfolio, incentives, diffusion beyond the rheumatology and dermatology setting, advantages/disadvantages of the models, and barriers to/facilitators of the introduction of models.
Statistical AnalysisWe present a description of the different models of multidisciplinary care of PsA patients. Given the nature of the study, there was no comparative statistical analysis.
ResultsWe analyzed a total of 12 models of multidisciplinary care. Jointly, they can be classified as 3 different subtypes: face-to-face (n=9), parallel (n=1) and preferential circuit (n=2). Most had been functioning for 1–2years and the main objective of all of them was to improve the health care received by their patients. More specifically, the objectives were to achieve an early diagnosis of PsA, the detection and management of complications of the disease, as well as counseling in terms of treatment (in patients with psoriasis as well as PsA). They were always evaluated from a multidisciplinary approach and were studied in these units during the time considered necessary by those responsible for referring them. Once the reason for their visit had been attended to, they usually returned to their attending physician. We wish to indicate that active and systematic data collection was carried out only to enable their correct utilization.
With regard to hospitals, these models are applied to level 3 or 4 centers, with reference populations that ranged from nearly 150,000 to almost 500,000 inhabitants, mostly corresponding to an urban population, with a very high level of computer literacy. The organizational and structural characteristics of the rheumatology and dermatology departments vary widely.
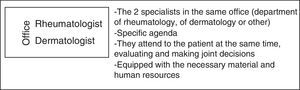
Multidisciplinary Care Models in Patients With Psoriatic ArthritisFace-to-face ApproachIn the model involving the face-to-face method (Fig. 1), the 2 specialists are physically in the same office and attend to the patient during the same appointment. The offices are in the department of rheumatology or in that of dermatology. They all have the necessary equipment, with the exception of an ultrasound scanner (depending on the center).
All of the offices have at least 1 permanent dermatologist and a permanent rheumatologist. Some offices have more than 1 specialist, and they take turns. Each has a colleague to substitute for the permanent physician if the latter is going to miss a patient's appointment.
There is no specific nurse assigned to the unit, but access to members of the nursing staff is ensured.
Most have no explicit written objectives (in the form of an agreement, for example), but they coincide in that the main aim is to improve the care provided to PsA patients, in the attempt to make the health care system more efficient and enhance the relationship among specialists. These units are mainly characterized as “one-stop”. However, the users include a growing number of complex patients who require a larger number of follow-up visits, and some end up transferred to these offices.
Regarding the norms for the admission and discharge of patients, they are controlled by the departments of rheumatology and dermatology, who follow transfer criteria that are generally well-defined. In most of the patients, there are uncertainties concerning the diagnosis and/or the therapeutic approach (including safety). In the majority of cases, the transfer has involved the usual form (on paper), but not always. The reason for seeing the patient may appear in the electronic medical record.
The patients return to their attending physicians once the motive has been attended to. Depending on the patient and/or center, the patient may be referred with treatment recommendations and, in other cases, with the prescription of a new treatment, for which the patient is being controlled.
Except in a few circumstances, most of these units have had, and continue to have, problems with their agendas. The admissions department does not allow the generation of a single agenda in which the activity simultaneously processes 2 different specialties. Thus, some centers have found diverse strategies to handle the situation. Some have 2 agendas with different names (1 for each specialty, with different patients). The patients from the other agenda are later included in the first (as emergencies, unforeseen, etc.). Therefore, all the patients attended to are processed as though they had been seen by both specialties. The patients are scheduled for successive appointments (first, one from one agenda and, a little later, another patient from the other agenda). In another center, on an unspecified agenda of this activity in a department, all of the patients will be scheduled in multidisciplinary visits. This means that this has to be reviewed systematically to ensure that only those of the multidisciplinary unit are recorded. Later, the other specialist processes them in his or her department as emergencies, unforeseen, etc. In another, each year, the activity is processed for 1 of the 2 departments. Finally, in 1 center, the activity is processed as being from only 1 department.
The frequency of these visits is variable, 1 or 2 appointment each month; normally, 1 each month. The number of patients seen, like the time devoted to each, is variable, from 20 to 40min per patient.
On the other hand, all of the professionals follow the consensus and guideline recommendations, both Spanish and international, in addition to their acquired personal experience. This is all adapted to the features of the health center or area. Specific protocols for these units have not been designed.
In most cases, a specific report is given to the patient.
Data collection is electronic in all the centers that provide joint multidisciplinary care. There is wide variability in the data gathered and where—in the record—they are stored. There are centers in which each department has a copy of the same record and/or process, and others in which they are filed among the documents corresponding to the department from which each patient is referred, and still others in which another process is created for the other department. On the other hand, there are units that have a specific database apart from the medical report in which they store data (mostly retrospective) to evaluate the health outcomes of the measures taken.
Patients are seen by both specialists at each visit. Depending on the reason for the appointment, one specialist may have to attend to some other activity. Both are responsible for attending to the patient, including decision making. There is no need to wait for a patient to visit to discuss any occurrence by phone, e-mail, etc.
With the development of these joint multidisciplinary care units, many professionals have decided to participate in research projects and hope to get involved in more (if they can). Moreover, their knowledge and skills in the management of PsA have increased considerably.
In addition, dermatology, rheumatology and/or family residents are rotating in many of these units. In some, there are even students. However, they do not usually hold joint clinical meetings.
In contrast to traditional care, patients see 2 specialists on the same day, which means it can be timesaving. Moreover, joint care can avoid the duplication of ancillary tests and prevent diagnostic or therapeutic delays. These face-to-face encounters may be the model of choice (if they can be adjusted to the characteristics and needs of the center and/or those of the professionals).
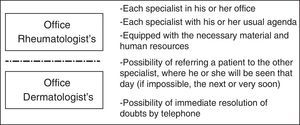
Parallel ApproachIn these models (Fig. 2), the dermatological and rheumatology visits are separate, but physically are close together and the patients are attended to at the same time. Patients go to one office and then to the other. The specialists discuss the patients or can even see them jointly, but only in cases in which a specialist considers it necessary. Doubts are often resolved by phone. The patients go to one appointment, where they are seen by the specialist and the process is recorded, and then they go to the other, where the specialist can see what his or her companion has written. With this exception, everything described above for the face-to-face multidisciplinary model can be applied here. The remainder of the characteristics are similar to the face-to-face approach.
Although there is less time spent together, to see how each professional works as occurs in the face-to-face appointments, those taking part in these visits also comment that they learn a great deal about the other specialty.
Preferential CircuitsIn this model (Fig. 3), each specialist continues in his or her usual office in the corresponding department, with their customary agendas. In visits of this type, there is no interval or specific time allotted. It is very much like the habitual clinical appointment and, although it seems to be very different from the other 2 models, many of the aspects commented above also apply here.
The major difference with regard to usual clinical practice is that the 2 specialists are qualified, trained in PsA, with their referral criteria, and can schedule a rapid multidisciplinary appointment or other undertaking, at any time, or whenever necessary and effective. Each specialist remains in his or her usual office, but will be able to find time if the other specialist, when it arises, studies a patient who could be amenable and decides to arrange for his or her referral. These patients should be seen that same day or in a maximum of 48h. There are certain patients, very complex patients, for example, that can be seen jointly. Although this occurs, it is an exception. This functions, as we say, in a more independent way.
As in the parallel visits, the telephone also helps to resolve doubts that arise or to discuss patients, always following pre-established criteria. As in the other approaches, the participants in these models make it clear that each has learned a lot from the other.
Experience in Introducing Models of Multidisciplinary CareThere is certain variability in the training requirements when establishing multidisciplinary models. In some centers the interest and experience in treating PsA patients was sufficient. In others, it was necessary to set up some type of previous training, including a rotation in the other department in the multidisciplinary care project. All of those interviewed coincided in that it is essential that those participating get along well, as is the need to measure these models for multidisciplinary care in terms of health (not of activity). This is one of the present challenges to these models; that the data that has to be systematically gathered to evaluate the outcomes of these approaches, must be expressed in terms of health.
When it comes time to introducing a multidisciplinary care model, those interviewed refer to the good planning of the entire process and recommended following a series of steps (Table 1). One of the major barriers mentioned with regard to establishing these units is the organization of the agenda/s, which should be decided before beginning. In principal, the model should be evaluated every 3–6 months and the necessary adjustments should be made over time (Table 2), this during approximately the first 2 years. From the start, and especially after that period, it is important to have a strategic plan that must be evaluated, as well as others that must be undertaken when the first are accomplished, and there has to be a plan for improving the model on the basis of errors, events, etc.
General Steps to Follow in the Introduction of a Multidisciplinary Care Model for Patients With Psoriatic Arthritis (PsA).
| Preintroduction steps |
|---|
| 1. Look for 2 involved specialists, with experience and interest, and who get along well |
| 2. Communication between directors or others responsible for the department to get their approval |
| 3. If necessary, present the proposal to the management and/or medical direction |
| 4. Define collectively: |
| • Type of model that best fits the circumstances of the center/professionals |
| • Criteria for patient access and discharge |
| • Intervals between visits and no. patients/visit (joint models) |
| • How and which days to communicate by phone, e-mail, in person, etc. |
| • Location for multidisciplinary visits (joint models) |
| • Necessary materials (computer, chairs, etc.) |
| • If necessary: protocols, guidelines |
| • Level of responsibility/implication in patient follow-up and treatment: |
| - Decide whether to recommend or to directly change therapy |
| - Should biologic therapy be indicated, establish a criteria as to who has to calculate the prescription |
| • Planned objectives |
| • Recording and evaluation of the activity (what, who, when, etc.) |
| • Measures (activity of the visit, activity and damage due to PsA, quality of life. etc.) |
| 5. Prepare the logistics of the agenda |
| • Attempt to prepare a single agenda with the activities of both departments |
| 6. Present the project to the 2 departments |
General Steps to Follow During Establishment (First 2 Years) and After That Period, From a Multidisciplinary Care Model.
| Steps during establishment (first 2 years) |
|---|
| 1. Look for efficient formulas to expedite the visits |
| 2. One report to the patient and another to the attending physician (can be different) |
| 3. Evaluate the multidisciplinary visit and make adjustments: |
| • Once started, evaluate every 3–6 months, making necessary adjustments: |
| - On the agenda, changes in intervals and/or no. of patients per visit |
| - Remind departments of the service and the referral criteria |
| - Implicate, train nursing staff/nursing assistant |
| - Define more specifically the attitude to adopt with certain types of patients |
| - Need of adjustments in the electronic medical record |
| - In the case of data collection, determine if it takes too much time, if it is feasible, if variables have to be modified, reduce the number to be collected, etc. |
| • At the end of one year, evaluation of the specific objectives proposed |
| Postestablishment steps (after the first 2 years) |
|---|
| 1. Evaluation of the unit and its objectives |
| • Should be performed every 1 or 2 years |
| - Analysis of anything that is not going well, events, etc. |
| - If some objective has not been accomplished, examine why |
| - This will help to design an improvement plan |
| 2. Together with the improvement plan, new objectives can be proposed. In addition to the clinical objectives, others related to the investigation and/or teaching can be assessed |
| 3. Once consolidated, it can be seen whether the unit meets the quality standards put forward in NEXUS |
| 4. Likewise, the introduction of the quality indicators also generated in NEXUS can be considered |
In this article, we have described 3 different types of multidisciplinary care for PsA patients, as well as the experience of introducing them. Although they may differ in structure and organization, they are all focused on providing better care to those patients, as well as to improve the efficiency of the health care system. Moreover, they have promoted collaboration between specialties. At the present time, they are recommended for the care of patients with PsA.8,9
There are previous experiences reported on multidisciplinary care in PsA. One involves the a model of face-to-face multidisciplinary care in the United States.12,13 After 6 years it was established that, in this modality—and in comparison with the previous traditional system (in which each specialist attends to a patient independently), more diagnoses were reviewed, facilitating the detection and confirmation of arthritis. Likewise, more systemic treatments were prescribed, including biologic therapies. On the other hand, a report presented at a meeting shows that a face-to-face multidisciplinary unit in the United Kingdom achieved high levels of satisfaction on the part of patients.14 However, more data are necessary to determine whether these multidisciplinary units, in comparison with the usual clinical approach, improve the course and outcome of these patients.
In Spain, data have also been published on a unit that follows a similar model of care, although it is functioning with existing resources.10 In this clinic, there was an improvement in patient management of those who had problems involving the diagnosis or disease control. There has also been an increase in the early diagnosis of arthritis, which has made it possible to initiate early treatment. Moreover, since the unit was introduced, collaboration between the specialties of rheumatology and dermatology has increased and the model has also been exported to other hospitals. This is one of the models analyzed and described in the present article.
This face-to-face multidisciplinary model has been found to be ideal on the part of professionals. It offers the possibility of standardizing the patient visit, gathering and analyzing its activity and, using a very special approach, reinforce the collaboration between the 2 specialties with the creation of referral criteria and protocols for patient management accorded by consensus.
There is also a work published in an international congress that refers to the 2-year experience in a parallel approach in Spain.15 In this model (included in this study), each patient is seen first by 1 specialist and, subsequently, by the other. After 3 years of follow-up, among other things, it has been found that the treatment has been modified in more than half of the patients.
A possible advantage to the parallel model over the face-to-face model is that not all of the patients require that the 2 specialists see them in depth. A patient expresses his or her doubts on arrival, and the necessary decisions are then considered. The other specialist can then pose any questions very rapidly. This can save time, would enable a larger number of patients to be seen.
Finally, we have found a third type of multidisciplinary care, which is the preferential circuit. This model is more similar to usual clinical care, although, it must be remembered that there is a very close collaboration among specialists and the possibility that the patient be evaluated by the 2 specialists the same day, in accordance with the protocols and arrangements in this respect. This model could be proposed in smaller centers, with fewer resources, or as a form of multidisciplinary care prior to the establishment of 1 of the models described above. In principal, this approach would be easier to introduce.
Regardless of what has been portrayed here, there is no doubt that the election of one model or another will depend on the needs of the center/health area, of the departments and professionals, as well as the available resources. As we mentioned earlier, this can start with a strategy that is easier to establish, like the preferential circuit, and another may be adopted later on.
On the other hand, regarding its introduction, good planning of the process can help enormously in the success of the undertaking. In this respect, it is essential that the participants in the multidisciplinary clinics be interested in the subject and that they get along well. Moreover, it is necessary that questions concerning agendas be accorded prior to beginning to introduce any of these models.
Finally, although at the present time, we need more data on the efficacy of these multidisciplinary care models. It seems clear that we can improve the management of patients with psoriasis or PsA, despite diagnostic uncertainties or questions on the treatment, as well as the results of the health care system. All this can be done, as we also promote collaboration among different medical specialties.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis project was funded by the Spanish Rheumatology Foundation.
Conflicts of InterestJosé Carlos Ruiz Carrascosa has received fees for conferences and for trials promoted by Abbvie, Pfizer, Novartis, MSD and Janssen. Conrad Pujol has received grants and fees related to research, as a consultant, and for training in the following companies: Abbvie, Janssen, LEO, MSD, Novartis and Pfizer. Raquel Rivera has participated in clinical trials, and worked as a consultant and a speaker for Abbvie, Celgene, Janssen, Leo-Pharma, Lilly, MSD, Novartis, Pfizer and Novartis. The remaining participants declare they have no conflicts of interest.
Please cite this article as: Queiro R, Coto P, Rodríguez J, Notario J, Navío Marco T, de la Cueva P, et al. Modelos de atención multidisciplinar en pacientes con artritis psoriásica en España. Reumatol Clin. 2017;13:85–90.