We present the clinical and ultrasound findings of four patients with moderate synovitis and urticarial skin lesions associated with sports activity in warm environments. We include progress after treatment with hydroxycin. We suggest a causal relationship similar to cholinergic urticaria where the neighbouring synovium responds with effusion that self-limits once the triggering process has been halted.
Presentamos los hallazgos clínicos y ecográficos de 4 pacientes con sinovitis moderada y lesiones cutáneas urticariales asociadas a la actividad deportiva en ambientes cálidos. Incluimos la evolución tras su tratamiento con hidroxicina. Sugerimos una relación causal similar a la urticaria colinérgica en la que la sinovia vecina responde con derrame que autolimita una vez suspendido el proceso desencadenante.
Cholinergic synovitis is a rare dermatological entity, characterised by the appearance of pruriginous weals as a response to local increase in temperature.1 It is not part of physical urticaria in the strict sense since the heat trigger is not necessarily exogenous.2 Recently, over 5 years, we have had the experience of observing and treating 4 cases of local synovitis associated with weals after isolated physical effort at high temperatures.
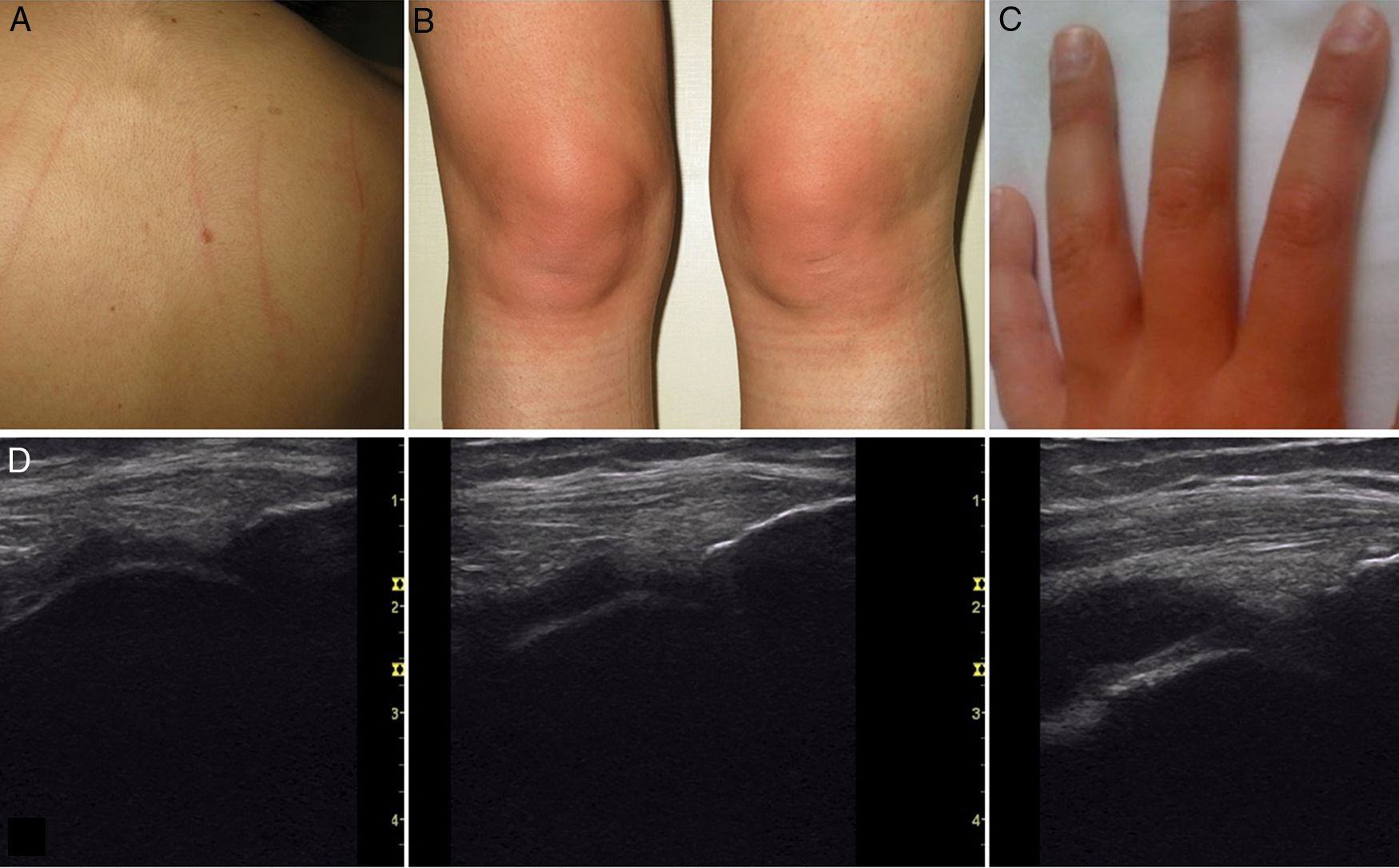
Clinical observationsCase 1A 25-year-old woman, with no history of asthma or known atopia who, during the summer and after physical exercise, presented swelling of both knees associated with erythema on the anterior face and pruritis. Dermographism was found on examination (Fig. 1A and B). Both knees showed synovial effusion with minimal membrane proliferation and absence of power Doppler signal. After 2h the skin lesions disappeared, and 24h later the volume of synovial fluid was physiological. Days after the event, 1mg subcutaneous methacholine was administered, in a concentration 1:100 (methacholine test) that caused the onset of weals. The patient was treated with hydroxycholine 100mg/day during the summer months with full resolution of symptoms.
(A) Dermographism observed in case 1. (B) Appearance of the knees 1h after physical activity in case 1. (C) Appearance of the hands in case 2 after isometric dumbbell exercises. (D) From left to right: basal situation of the pre-patellar recess of the patient of case 3, 1h after exercise and 3h later.
A 28-year-old woman, sedentary and overweight. In the summer after a sports routine with low weight dumbbells, she started to notice functional limitation in her elbows, and swelling in her elbows and metacarpophalangeal joints that became more evident when using elbow pads and gym gloves (Fig. 1C). She had erythema and itching without weals. Ultrasound revealed synovial effusion in the radiohumeral joint and the MCPJ of both hands. The lesions lasted 4–6h and the synovitis disappeared after 12–24h. After the lesions and the functional limitation had disappeared, the methacholine test was positive. Treatment with hydroxycholine 75mg/day was initiated that had to be increased to 200mg/day to achieve complete control of the manifestations. The patient had to start treatment again the following summer.
Case 3A 31-year-old woman with a known history of asthma and cholinergic urticaria from the age of 25, presenting with swelling and onset of weals on the anterior of her knees after physical exercise cycling) most often in the summer months. Moderate parapatellar synovial effusion and mild membranous proliferation without hyperaemia were observed in both knees (Fig. 1D). The skin lesions persisted for 2–8h and the swelling disappeared in the first 24h after discontinuing sport. She had had a positive methacholine test 4 years previously and therefore it was decided not to perform a further provocation test. She responded satisfactorily to hydroxyzine 100mg/day, which she only uses during the summer months.
Case 4A 34-year-old woman. A walking enthusiast, wearing ankle weights. During the summer she had ankle swelling associated with the appearance of pruriginous weals on the back of her foot. Ankle ultrasound showed moderate effusion with no synovial proliferation on the tibioastragaline joints. Neither finding lasted more than 24h after discontinuing sport. The methacholine test was positive, and she was treated with hydroxyzine 100mg/day which almost completely resolved uncovering the ankles while walking.
None of the patients presented significant analytical alterations. In no case were the acute phase reactants altered. All the patients were seronegative for rheumatoid factor and citrulline antipeptide antibodies. Case 3 had ANA (1/160) in a single test and 2 subsequent negative studies. In no case did the symptoms cause absence from work.
DiscussionThe 4 cases meet the ultrasound definition of synovitis without hyperaemia and with a low proliferative component. They have in common the chronological association of repeated local heat in a warm environment. Up to this point, the documented synovitis could be explained as a response to previously reported mechanical synovial stress in healthy subjects.3 However, the persistent relationship with characteristic dermatological manifestations of cholinergic urticaria and the – inconstant – presence of dermographism, suggest that the origin of symptoms was a complex response to both skin and synovial heat. The relatively rapid return to normality of the skin lesions suggests a physiopathological vasomotor mechanism which, in the absence of synovial hyperaemia, would not seem to explain the synovial effusion. On the other hand, the low synovial membrane proliferation suggests that the genesis of the process would be in the skin, and that the effusion would be a synovial reaction by proximity.
There is no physiopathological explanation for cholinergic urticaria, and its association with transient synovitis has not been previously described in the literature. However, methacholine test positivity and favourable synovial response to hydroxyzine, a classical treatment for cholinergic urticaria, establish a physiopathogenic link between the mechanisms that produce skin manifestations and those that cause synovial effusion.
ConclusionThe entity described in these 4 cases, and that we arbitrarily suggest calling self-limiting cholinergic synovitis, can be understood as a synovial response to the same cholinergic stimuli characteristic of urticaria in superficial joint territories or close to the skin and triggered by local heat generation in high temperature environments. However, as in the case of cholinergic urticaria, cholinergic synovitis is an entity that should be the subject of future studies.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Guillén Astete C, Zamorano Serrano M, Luque Alarcón M. Sinovitis colinérgica: descripción de 4 casos. Reumatol Clin. 2021;17:113–115.