The chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) and autoimmune/inflammatory syndrome induced by adjuvants (ASIA) were described a decade ago. There are a limited number of reports and these diseases are still underdiagnosed.
We presented a 35 years-old patient with clinical manifestations of cerebellum affection and enhancement in the MRI, with the influenza vaccine as the only triggering factor.
Infectious diseases, malignancy, and additional systemic involvement were ruled out; therefore, on suspicion of CLIPPERS syndrome, the patient received corticosteroid therapy with an adequate response.
The knowledge of CLIPPERS syndrome as an unusual ASIA presentation and high response to the corticosteroids may lead to a timely diagnosis, appropriate treatment, and follow up with better outcomes for patients.
La inflamación linfocítica crónica con realce perivascular pontino que responde a los esteroides (CLIPPERS) y el síndrome autoinmune/inflamatorio inducido por adyuvantes (ASIA) se describieron hace una década. Hay un número limitado de reportes y estas enfermedades aún están infra diagnosticadas.
Presentamos un paciente de 35 años con cuadro clínico de afectación del cerebelo y realce en la RM, con la vacuna anti-influenza como único factor desencadenante.
Se descartaron enfermedades infecciosas, malignidad y afectación sistémica, por lo tanto, ante sospecha de síndrome de CLIPPERS, recibió tratamiento con corticoesteroides con una respuesta adecuada.
El conocimiento del síndrome de CLIPPERS como una presentación inusual de ASIA y su alta respuesta a los corticosteroides puede conducir a un diagnóstico oportuno, un tratamiento adecuado y un seguimiento con mejores resultados para los pacientes.
The chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) and autoimmune/inflammatory syndrome induced by adjuvants (ASIA) were first described a decade ago1,2; until date, there are a limited number of reports and these diseases are underdiagnosed.
Clippers is characterized by the perivascular infiltration of T-cell lymphocytes in the pontine centric area and the pons but can involve other brain parts.3 The pathogenesis is still poorly understood; however, it has been described after a potential immune triggering event.4 Being neurological manifestations part of the spectrum of ASIA highlights the importance of knowing this disease. We described a CLIPPERS Syndrome after the influenza vaccination.
Clinical observationA 35-year-old previously healthy man started with ataxia in gait six days following influenza vaccination, with increased symptomatology and binocular diplopia in the next five weeks.
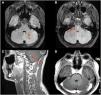
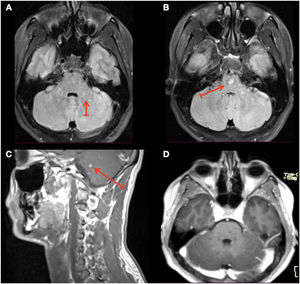
The neurological examination revealed the following remarkable findings: cranial nerves with slight limitation in the abduction of the left eye, with multidirectional nystagmus, motor system, with normal force, hyperreflexia of the four extremities, cerebellum with severe dysmetria in the four extremities, he presented broad-based gait and postural instability. A magnetic resonance imaging (MRI) was performed, which showed hyperintense lesions in the pontine region cerebellar peduncles and cerebellum (Fig. 1A, B), with “peppering” enhancement after contrast administration (Fig. 1C).
(A, B) MRI of the brain T2 Flair at presentation with hyperintense lesions (arrows). (C) MRI of the brain T1 post-gadolinium at presentation, showing foci of pontine “peppering” enhancement lesion highly suggestive of a perivascular distribution. (D) MRI of the brain T1 post-gadolinium at one-month follow-up showing full recovery after corticosteroids treatment.
Biochemical data: ANAs, anti-DNA, rheumatoid factor, HIV, VDRL, oligoclonal bands and AQP4 were negative. The CSF study showed no alterations; cultures and PCR for tuberculosis were negative. Infectious diseases, malignancy and additional systemic involvement, were ruled out; therefore, on suspicion of CLIPPERS syndrome, the patient received methylprednisolone 5g (1g daily) with total clinical improvement. He was discharged with azathioprine 2.5mg/kg/day and prednisone 1.0mg/kg/day with a tapering strategy, decreasing dose of 10mg every two weeks, until 30mg, and then 5mg every two weeks until discontinued. At 1-month follow-up, the MRI lesions showed total resolution (Fig. 1D).
DiscussionWe presented a patient with clinical manifestations of cerebellum affection and enhancement in the MRI, with the influenza vaccine as the only triggering factor.
CLIPPERS syndrome may be underdiagnosed due to the lack of knowledge of the disease. The manifestations of the reported cases are heterogeneous, but in general, the typical presentation is the brainstem and cerebellum subacute symptoms.1,3,4
The CLIPPERS syndrome has been characterized by hallmark lesions in MRI, punctate and curvilinear “peppering” lesions. Although this imaging pattern is very suggestive of this syndrome, it is mandatory to rule out differential diseases, such as infectious, malignancies or rheumatology conditions, since these can mimic the lesions.4 Remarkably, several reports mention CLIPPERS as a pre-lymphoma state or as an initial manifestation of a systemic disease; besides the need for research in that field, follow-up of these patients would lead to a prompt diagnosis and timely interventions.5
There are several reports of neurological affection after influenza vaccination with a time range of 2–60 days, which have been reported as an ASIA. Since the Influenza vaccine has several adjuvants, this may trigger an immune reaction in some predisposed subjects.6,7
This situation draws attention in the COVID-19 vaccination era, where there are reports of ASIA and immune-mediated diseases after different COVID-19 vaccines, highlighting neurological disorders.7,8
The patient met two ASIA diagnostic major criteria2; he was previously healthy, was exposed to an adjuvant and developed manifestations of neurology disease, besides that the perivascular inflammatory cell infiltrates and response to corticosteroids strongly suggest autoimmune disease.1,6,9
Of interest, Tobin et al.10 reviewed the characteristics of 35 patients in Mayo Clinic with suspected CLIPPERS, of the 22/23 confirmed patients presented a complete response to corticosteroid treatment, and at follow-up, most of them continued on immunomodulatory therapy, of note, our patient, has continued with azathioprine, maintenance dose 1.5mg/kg/day for 18 months without relapses. The treatment time is still unclear, but reviews show a trend of maintaining immunomodulatory therapy for at least 12 months.3
ConclusionsThese days, where there is a COVID-19 vaccination program worldwide, and autoimmune reactions have been reported with different vaccines,7,8 the knowledge of CLIPPERS syndrome as an unusual ASIA presentation and high response to the corticosteroids may lead to a timely diagnosis, appropriate treatment, and follow up with better outcomes for patients.
Informed consentInformed consent was obtained from the patient.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone reported.
We thank the patient for granting permission to publish this information.
All authors contributed equally and met the ICMJE authorship criteria.