Cogen syndrome (CS) is a systemic inflammatory disease the standard characteristics of which are interstitial keratitis and audiovestibular symptoms similar to those of Ménière's syndrome, with an interval between both manifestations of under 2 years.1 However, atypical forms of the disease exist where ocular or audiovestibular symptoms are different, or the interval between the two is longer than 2 years.2 Its aetiology is unknown, but it has been suggested that there are mechanisms of autoimmunity in the inner ear.3 Apart from steroids, there is no standard treatment alternative for patients with poor response. Cochlear implant offer the opportunity to restore hearing function and communication.4 Association with spondyloarthritis uncommon and we therefore considered it interesting to present this case where satisfactory posterior evolution to the use of steroids, infliximab took place and a cochlear implant was used.
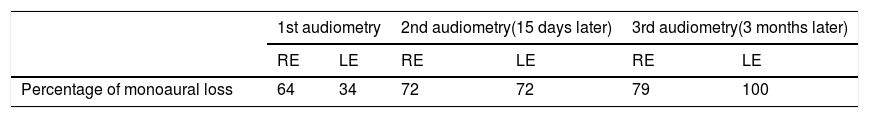
We present the case of a 58-year old man, a cardiologist, with a background of high blood pressure, a tobacco habit and palmoplantar keratoderma since adolescence. He stated he had had inflammatory lumbago and cervical pains since 49 years of age, associated with nonspecific urethritis with no recurring events. At 55 years of age he presented with left keratouveitis. There was evidence of scar-pitting, dactylitis, limitation in flexing hips and a normal breadth of axial movements. Bilateral grade 2 Sacroileitis. Magnetic resonance of the sacroiliac joints: right fatty infiltrate and active left erosion. ESR and RCP rates normal. RA-test and HLA-B27 negative. Anti-HSP-70 positive. Four months after the keratouveitis his hearing was reduced. Audiometry reported moderate hearing loss and bilateral neurosensorial hearing loss. He received 16mg/iv/12h dexametasone for 3 days with improvement. Two weeks later, progressively exacerbated onset of tinnitus. He received treatment with 1g/iv/3 dose of methylprednisolone and later 25mg prednisone daily, 20mg/oral/week methotrexate and 80mg subcut STAT adalimumab and later 40mg/subcut/15 days. He was referred to a hearing clinic but the second audiometric test reported severe bilateral neurosensorial hearing loss, and the third one (3 months later) reported severe right and profound left hearing loss (Table 1) and as a result the adalimumab was withdrawn. He began treatment with IV cyclophosphamide and took 6 fortnightly doses (4 of 500mg and 2 of 750mg) with no improvement. The patient abandoned treatment due to major depression which was resolved satisfactorily with pharmacological treatment. He was given a cochlear implant a year after the onset of clinical symptoms and this has functioned up until now. Two months later, he started treatment with infliximab (5mg/kg)+20mg/week methotrexate and up to 5mg daily of prednisone was also prescribed. He received treatment with infliximab for 2 years, which was suspended due to the lack of availability of the same, but the patient remained stable and went back to work.
Cogen syndrome is of low prevalence and is rarely associated with spondyloartritis. Its evolution is generally torpid up to profound hearing loss and there is little response to immunosuppressant treatment. This patient had spondyloartritis with cutaneous involvement (but did not meet with the CASPAR criteria for psoriatic arthritis),5 and presented with a normal range of axial movements due to the hyperelasticity traits. During the course of the disease he quickly and progressively developed neurosensorial hearing loss which responded to steroid treatment, was associated with anti-HSP70 antibodies and was therefore associated with inner ear autoimmune disease.6 This, together with the keratouveitis, resulted in diagnosis of atypical Cogen syndrome. Few cases regarding this association have been described worldwide and they coincide in the irregular response to immunosuppressant treatment. Post cochlear implant evolution was satisfactory, and has been maintained up until the present day (45 months after its implantation), despite not continuing with the infliximab treatment at present. In this patient, the association between the medical and surgical treatment allowed for the restoration of hearing and the clinical remission of spondyloarthritis, reflecting the importance of multidisciplinary management in complex cases.
Please cite this article as: Guasamucaro-Castillo MG, Bonito-Torrealba FA, Maldonado T, Posadas-Escudero A. Síndrome de Cogan y espondiloartritis. Reporte de caso. Reumatol Clin. 2019;15:e170–e171.