We present a case of RS3PE syndrome with positive rheumatoid factor (RF) that commenced as positive following the development of a tumour. This normally occurs in these cases years before the appearance of the same.
RS3PE syndrome was described by McCarty in 1985. It occurs predominantly in men over the age of 60 years old (2/3),1 and it has a higher incidence in the white race and rural population.
It may be primary or secondary, associated with infections, systemic diseases, Sjögren's syndrome2 or rheumatoid arthritis (RA).3 It may be associated with digestive neoplasias, with very few described cases of colon adenocarcinoma,4 haematological, gynaecological and nephrological neoplasias,5 or drugs, such as type IDPP-4 antidiabetic drugs.6
It has a rapid onset, almost always in less than one month. It is characterised by symmetrical polyarthritis with synovitis of the extensor and flexor tendons, severe oedema with a depression in the back of the hands and weakness of the pelvic and scapular waists.
The criteria proposed by Olivo et al.7 are used for diagnosis, and in complementary tests RF is usually negative, although in the medical literature a very few cases are described with positive RF,8 as well as with positive anti-CCP.9
Prednisone is used in 95% of cases, of which 74% receive doses of from 15 to 20mg/day during treatment lasting for from 3 to 6 months.10
Our case is that of a 72 year-old man, Caucasian and living in a rural environment. He visited on several occasions due to oedema with a depression on the hands, fundamentally, and to a lesser degree on the ankles; pain and functional weakness in the scapular waist, morning rigidity, symmetrical polyarthritis of the upper limbs and difficulty in flexing-extending both hands. He had no fever, constitutional syndrome or clinical signs of arthritis; no aphtha or uveitis. He underwent treatment with a NSAID and diuretics for this reason, without showing any improvement.
The following aspects of his clinical history stood out: AHT, long-term DM2, dyslipidemia, arrhythmia due to auricular fibrillation, no rheumatological history and total colectomy with ileo-rectal anastomosis due to colon adenocarcinoma. He was in follow-up with no signs of relapse, and habitually took antihypertensive and antihyperlipidemic agents, as well as digoxin and oral antidiabetics (including IDPP-4 for several years).
The analytical findings were: 9.5g/dl haemoglobin, positive RF, 20UI/ml and raised ESR, 49mm/h. ANA, ANCA, anti-CCP, tumour markers, proteinogram and PCR determination showed no pathological results. A colonoscopy was performed which showed anastomosis without alterations, and oral endoscopy was normal. Hand X-rays showed no signs of erosive lesions and abdominal CT showed no signs of relapse or metastasis.
Treatment commenced with calcium, vitamin D and 20mg prednisone per day, giving rise to a notable improvement after a few days. The corticoid dose was reduced in successive check-ups, and the patient currently takes 5mg prednisone per day.
In our case, given the clinical characteristics described as well as the swift response to treatment with prednisone, although it has the peculiarity of positive RF, we are able to state that it is an RS3PE syndrome as it fulfils 6 of the 7 diagnostic criteria proposed by Olivo et al.
As this is a new entity that has hardly been described, with an unknown incidence and diagnostic criteria that are fundamentally clinical, 6 out of 7 of the same, with the exception of the RF determination, which is typically negative, we believe that this fact should strengthen the diagnosis, given that it is included in its definition, so that its positivity should not exclude it or rule it out.
Unlike other authors, who believe RS3PE syndrome to be a benign form of seronegative rheumatoid arthritis in the elderly, we see it initially as a different entity from other rheumatological processes which appears in the elderly in the majority of cases, although it may commence at early ages.2 The chief characteristic, which is present in 100% of cases, is oedema on the back of the hands. It may be associated with other diseases or evolve into a specific rheumatoid condition. Although it normally progresses with negative RF, this may sometimes be positive, as it is in our case. Thus something similar would occur with RA: a positive result of RF would not reveal the diagnosis of the same, given that approximately 20% of the individuals with RA do not have detectable values of RF; moreover, other diseases may arise with a positive RF result, including in individuals, above all the elderly and the healthy, so that it has no clinical repercussion in them (up to 5% of the healthy population).
We also believe that, although at the moment it was diagnosed the syndrome gave rise to no alarming signs and/or symptoms, the existence of a tumour has to be ruled out, and the patient has to be monitored: they may eventually develop a rheumatological disease (more so if at the moment of diagnosis alterations are found in an analytical or radiological test) or a tumour may develop over years, or it may be an essential form of the condition with an excellent prognosis.
More specifically, as our patient had had a tumour (altered immunity status) this may justify alteration in the RF, but nor is it possible to rule out that over time a rheumatic polymialgia or rheumatoid arthritis may develop, although this is rare, or a relapse of the tumour may occur. It is for this reason that we are monitoring the patient.
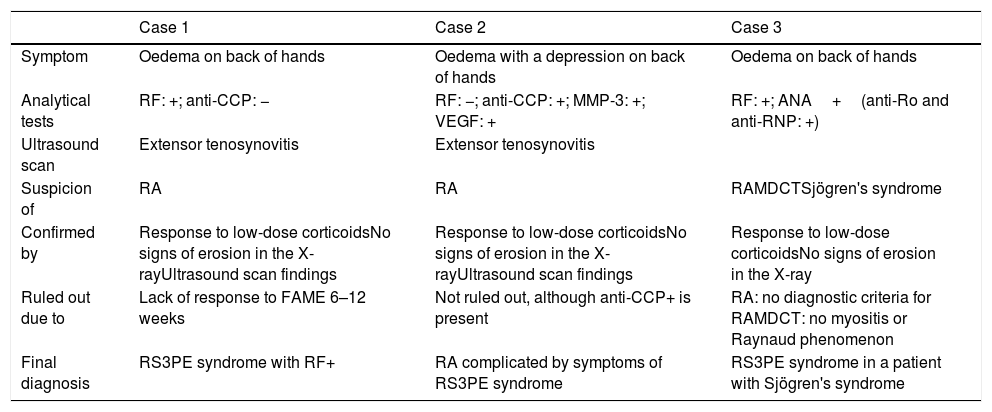
Finally, in those cases which are not seronegative (Table 1) if the suspicion exists that there is another entity, and if this is confirmed by laboratory tests or clinically then it should be treated and the response should be monitored. In those cases where this question is not fully clear low-dose corticoid treatment should be commenced, and if the response is favourable after a few days then the case consists of an RS3PE syndrome. Another option that would guide diagnosis would be IL-6 determination; nevertheless, to differentiate RA from the RS3PE syndrome it would be more useful to determine VEGF and MMP-3, as if they are raised this would favour the later diagnosis.
Coincidences of RS3PE Cases That Are not Seronegative.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Symptom | Oedema on back of hands | Oedema with a depression on back of hands | Oedema on back of hands |
| Analytical tests | RF: +; anti-CCP: − | RF: −; anti-CCP: +; MMP-3: +; VEGF: + | RF: +; ANA+(anti-Ro and anti-RNP: +) |
| Ultrasound scan | Extensor tenosynovitis | Extensor tenosynovitis | |
| Suspicion of | RA | RA | RAMDCTSjögren's syndrome |
| Confirmed by | Response to low-dose corticoidsNo signs of erosion in the X-rayUltrasound scan findings | Response to low-dose corticoidsNo signs of erosion in the X-rayUltrasound scan findings | Response to low-dose corticoidsNo signs of erosion in the X-ray |
| Ruled out due to | Lack of response to FAME 6–12 weeks | Not ruled out, although anti-CCP+ is present | RA: no diagnostic criteria for RAMDCT: no myositis or Raynaud phenomenon |
| Final diagnosis | RS3PE syndrome with RF+ | RA complicated by symptoms of RS3PE syndrome | RS3PE syndrome in a patient with Sjögren's syndrome |
RA: rheumatoid arthritis; MDCT: mixed disease of the connective tissue; RF: rheumatoid factor; MMP-3: metalloproteinases; VEGF: vascular endothelial growth factor.
Please cite this article as: Moreno Obregón F, del Castillo Madrigal M, Díaz Narváez F, Pérez Delgado FJ. Síndrome RS3PE con factor reumatoide positivo. Reumatol Clin. 2019;15:e168–e169.