To determine the comorbidities associated with disability in patients with OA in Mexico (2013–2015).
Material and methodsA cross-sectional, retrospective and multicentre IMPACTAR study (n=7703) in Mexican patients (2013–2015). Comorbidities associated with disability were identified in 4971 patients diagnosed with OA from the IMPACTAR registry (n=7073). An adjusted logistic regression analysis was carried out by demographic, economic, clinical and medical variables.
ResultsMean age was 63 years; and 75% of the patients were women. Subjects with OA and presence of comorbidities are 42% more likely to develop disabilities than patients without associated comorbidity, considering age, sex, family income, OA diagnosis duration, and education level. The highest rate of people with disability (28.9%) was concentrated in Region 7, which corresponds to Mexico City. There are also significant differences between median family incomes, when the income of persons with disability is under $13 000 (IQR: 9000–16 000) Mexican pesos, compared to patients without disability. Almost half of the subjects (49.6%) reported having at least one comorbidity. Arterial hypertension was the risk factor with a statistically significant difference (32.8%) among those with disability (34.7%).
ConclusionsPrograms and interventions for OA patients should take into consideration comorbidity factors, being female, family income, and the region of residence as variables that may increase the possibility of developing an OA-associated disability.
Determinar las comorbilidades asociadas a la incapacidad en pacientes con osteoartritis (OA) en México (2013-2015).
Material y métodosEstudio IMPACTAR transversal, retrospectivo y multicéntrico (n=7.703) en pacientes mejicanos (2013-2015). Se identificaron las comorbilidades asociadas a la incapacidad en 4.971 pacientes diagnosticados de OA en el registro IMPACTAR (n=7.073). Se realizó un análisis de regresión logística ajustada por variables demográfica, económica, clínica y médica.
ResultadosLa edad media fue de 63 años, y el 75% de los pacientes eran mujeres. Los sujetos con OA y la presencia de comorbilidades tienen un 42% mayor de probabilidad de desarrollar incapacidades que los pacientes sin comorbilidad asociada, considerando la edad, el sexo familia, los ingresos, la duración del diagnóstico de OA y el nivel educativo. La tasa poblacional con mayor tasa de incapacidad (28,9%) se concentró en la Región 7, que corresponde a Ciudad de México. También existieron diferencias significativas entre los ingresos familiares medios, cuando la renta de las personas con incapacidad se sitúa por debajo de los 13.000$ (RIC: 9.000-16.000) pesos mejicanos, en comparación con los pacientes sin incapacidad. Casi la mitad de los sujetos (49,6%) reportaron tener al menos una comorbilidad. La hipertensión arterial fue el factor de riesgo con diferencia estadísticamente significativa (32,8%) entre aquellas personas con incapacidad (34,7%).
ConclusionesLos programas e intervenciones para pacientes con OA deberían considerar los factores de comorbilidad tales como sexo femenino, ingresos familiares y región de residencia como variables que podrían incrementar la posibilidad de desarrollar una incapacidad asociada a OA.
Rheumatic and musculoskeletal diseases are among the most common non-transmittable chronic diseases.1 Among these, Osteoarthritis (OA) is the most frequent in young adults and older individuals and is associated with short and long-term disability.2,3 OA is characterized by joint pain, stiffness, inflammation, and weakness, which lead to physical disability.4
In Latin America, by using the COPCORD methodology, OA prevalence varies between 2.3% up to 20.4%; primary or idiopathic OA represents 88.2% of cases,5 with the knee being the most affected (51.1%) and associated with a Health Assessment Questionnaire (HAQ)>0.375 (OR 1.9, 95% CI 1.5–2.4); in addition, the inability to kneel is a predictor for patients seeking healthcare visits.6
Worldwide, OA is the fourth most frequent cause of years lived with disability (YLDs),7 whereas in Mexico it ranks 8th among women an 13th in men.8 Some studies report that up to 50% of patients with symptomatic OA suffer from some degree of disability.9 According to the World Health Organization (WHO), “disability” is a general term covering impairments, activity limitations, and participation restrictions. An impairment is a problem in body function or structure; an activity limitation is a difficulty encountered by an individual in executing a task or action; while participation restriction is a problem experienced by an individual I involvement in life situations.10
Disability increases with age and disease duration, with pain being one of the most important causes of disability in patients with OA9,11–13. It has been reported that OA occurs in at least 10% of adults 60 years and older, it can damage any joint, with knee and hip the most affected.14
According to several studies, the main co -morbidities that influence OA are: obesity, diabetes mellitus, hypertension, dyslipidemia, metabolic syndrome, gout, and pulmonary diseases,5,14–18 with obesity and diabetes being the most associated with OA and the presence of disability.16–19
In Mexico, patient care with rheumatic and musculoskeletal diseases can vary widely since there a very peculiar health care system, and healthcare coverage is based on patient emplo yment and economic income.20
The aim of this study is to determine the association of co -morbidities and their impact on disability, since it represents the most important outcome at the public health level.
Materials and methodsTransverse, analytic and multicenter study of the “Iniciativa Mexicana de pacientes con Osteoartritis y Artritis Reumatoide” (IMPACTAR), in a nationwide sample involving 55 centers in 20 states in Mexico.
This study included 4971 consecutive patients 18 years and older with the diagnosis of OA according to American College of Rheumatology (ACR) classification criteria that received ambulatory care in public, private or social security institutions across Mexico during 2013–2015.
Patients belonged to different federative entities or states from the whole country, in order to classify their origin, we used the socio-economic region classification from the “Instituto Nacional de Estadística y Geografía” (INEGI), an autonomous agency of the Mexican Government to coordinate the National System of Statistical and Geographical Information.21
Prior informed consent, each subject completed a questionnaire regarding socioeconomic, clinical, healthcare, and physical disability aspects.
Disability was evaluated using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), which was designed to measure functional capacity in patients with OA and contains 24 items grouped in 3 different domains: pain (0–20), stiffness (0–8) and functional limitation (0–68); each item having 5 levels which are codified from 0 to 4 (none, mild, moderate, severe, and extreme).22,23 These domains result in an index score ranging from 0 to 12, and from these, two categories were created: absence of disability (<3) and presence of disability (> or =3).24
Statistical analysisA bi-varied analysis was performed to describe the main characteristics of the study population by using disability as a dependent variable. For categorical variables, frequencies and percentages were reported; the Pearson chi squared test was applied to determine statistically significant (P<.05) between both groups, and for continuous variables, the median and interquartile range, the Wilcoxon sum of range s was employed to compare medians (P<.05). The independent variables considered were: sociodemographics, economics, geographic, comorbidities and some health care related characteristics. Federation entities (states) from which patients were recruited were classified according to the INEGI socio-economic regions, where wellbeing related information is summarized in such aspects as education, employment, occupation, housing and health (7 is de most favorable stratum, and 1 the least favorable).21 To evaluate the association between co -morbidity and disability, we performed a logistic regression analysis adjusted for biologic co-variables like age, gender, time from diagnosis (three categories: <5 years, 5–10 years and >10 years from the diagnosis of OA up to the year of the IMPACTAR interview), family income (five categories in Mexican pesos: below 2598; between 2598 and 5196; between 5196 and 10,392; between 10,392 and 18,186; and above 18,186), and school grade. Once the statistical model was defined, diagnosis was performed by using a goodness of fit, specificity, and multicollinearity tests. The main predictor of disability variables was the presence of co-morbidity, which was defined as any morbidity in addition to OA in the study patients. Statistical analysis was performed with STATA software version 14.0.
Ethical considerationsThis study was approved by the Ethics committee of the University Hospital “Dr. José Eleuterio González” of the Universidad Autónoma de Nuevo León. Registry No. RE14-004 and by the Instituto Mexicano del Seguro Social (IMSS) F-CNIC-2015-113.
Data confidentiality: The authors declare that they have followed the established protocols in their respective institutions in regards to patient data confidentiality, and that they have followed ethical guidelines or rules to publish with patient informed consent, and that all patients included in this study were provided with sufficient information about this study and gave their informed consent to participate.
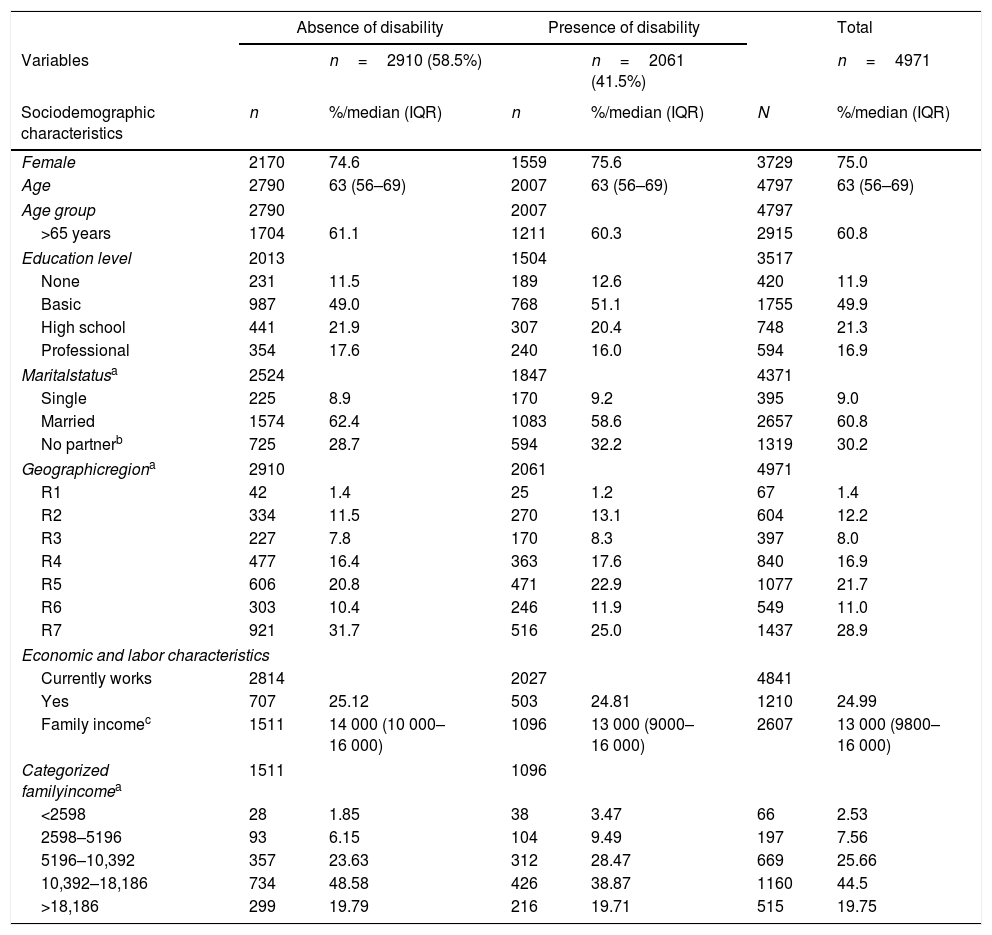
ResultsThe IMPACTAR registry accrued a total of 7073 patients; of these 4971 were selected by having a diagnosis of OA and a complete functional evaluation (WOMAC). Mean age was 63 years, 75% were female, with most having a basic education level (49.9%). Two groups were created: One with presence of disability (41.5%) and the other without (58.5%). (Table 1)
Sociodemographic, economic and geographic characteristics associated with disability in patients with OA in Mexico 2013–2015.
| Absence of disability | Presence of disability | Total | ||||
|---|---|---|---|---|---|---|
| Variables | n=2910 (58.5%) | n=2061 (41.5%) | n=4971 | |||
| Sociodemographic characteristics | n | %/median (IQR) | n | %/median (IQR) | N | %/median (IQR) |
| Female | 2170 | 74.6 | 1559 | 75.6 | 3729 | 75.0 |
| Age | 2790 | 63 (56–69) | 2007 | 63 (56–69) | 4797 | 63 (56–69) |
| Age group | 2790 | 2007 | 4797 | |||
| >65 years | 1704 | 61.1 | 1211 | 60.3 | 2915 | 60.8 |
| Education level | 2013 | 1504 | 3517 | |||
| None | 231 | 11.5 | 189 | 12.6 | 420 | 11.9 |
| Basic | 987 | 49.0 | 768 | 51.1 | 1755 | 49.9 |
| High school | 441 | 21.9 | 307 | 20.4 | 748 | 21.3 |
| Professional | 354 | 17.6 | 240 | 16.0 | 594 | 16.9 |
| Maritalstatusa | 2524 | 1847 | 4371 | |||
| Single | 225 | 8.9 | 170 | 9.2 | 395 | 9.0 |
| Married | 1574 | 62.4 | 1083 | 58.6 | 2657 | 60.8 |
| No partnerb | 725 | 28.7 | 594 | 32.2 | 1319 | 30.2 |
| Geographicregiona | 2910 | 2061 | 4971 | |||
| R1 | 42 | 1.4 | 25 | 1.2 | 67 | 1.4 |
| R2 | 334 | 11.5 | 270 | 13.1 | 604 | 12.2 |
| R3 | 227 | 7.8 | 170 | 8.3 | 397 | 8.0 |
| R4 | 477 | 16.4 | 363 | 17.6 | 840 | 16.9 |
| R5 | 606 | 20.8 | 471 | 22.9 | 1077 | 21.7 |
| R6 | 303 | 10.4 | 246 | 11.9 | 549 | 11.0 |
| R7 | 921 | 31.7 | 516 | 25.0 | 1437 | 28.9 |
| Economic and labor characteristics | ||||||
| Currently works | 2814 | 2027 | 4841 | |||
| Yes | 707 | 25.12 | 503 | 24.81 | 1210 | 24.99 |
| Family incomec | 1511 | 14 000 (10 000–16 000) | 1096 | 13 000 (9000–16 000) | 2607 | 13 000 (9800–16 000) |
| Categorized familyincomea | 1511 | 1096 | ||||
| <2598 | 28 | 1.85 | 38 | 3.47 | 66 | 2.53 |
| 2598–5196 | 93 | 6.15 | 104 | 9.49 | 197 | 7.56 |
| 5196–10,392 | 357 | 23.63 | 312 | 28.47 | 669 | 25.66 |
| 10,392–18,186 | 734 | 48.58 | 426 | 38.87 | 1160 | 44.5 |
| >18,186 | 299 | 19.79 | 216 | 19.71 | 515 | 19.75 |
IQR=interquantile.
In this study most subjects belonged to region 7 which corresponds to Mexico City, the states of Nuevo León, Coahuila and Jalisco with 28.9% followed by region 5 comprising the states of Baja California Norte, Baja California, Sonora, Chihuahua and Tamaulipas with 21.7%, whereas the least represented region was region 1 which corresponds to the states of Guerrero, Oaxaca, and Chiapas with 1.4%.
The median family income in our cohort was $13 000 MXP (IQR: 9800–16 000) (Table 1).
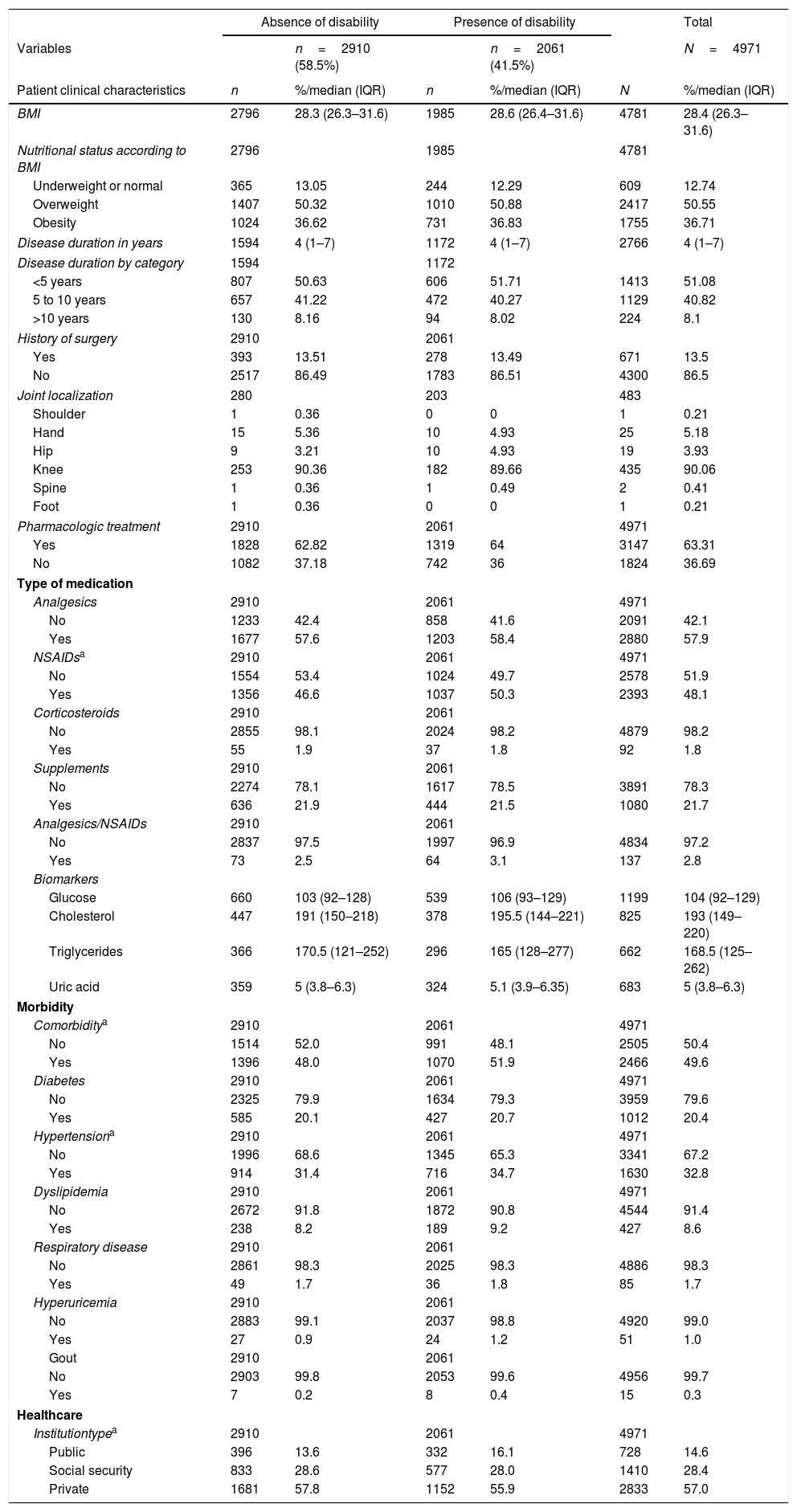
The median Body Mass Index (BMI) was 28.4 (26.31.6) kg/m2, and according to the WHO classification, 86.7% of patients were obese or overweight.
The general median to the time of OA diagnosis was 4 years (IQR 1–7 years), and 51.2% of patients had less than 5 years since diagnosis. The most affected joint in OA patients was the knee (88.8%), and up to 13.5% of patients reported history of joint surgery.
When we investigated the different types of medications taken by patients at the time of the interview, we found that 48.1% took non-steroidal anti-inflammatory drugs (NSAIDs).
More than 49% of subjects had at least one co-morbidity, with hypertension being the most prevalent in 32.8% (Table 2)
Clinical characteristics, pharmacologic treatment, and healthcare institution associated with disability in patients with OA in Mexico 2013–2015.
| Absence of disability | Presence of disability | Total | ||||
|---|---|---|---|---|---|---|
| Variables | n=2910 (58.5%) | n=2061 (41.5%) | N=4971 | |||
| Patient clinical characteristics | n | %/median (IQR) | n | %/median (IQR) | N | %/median (IQR) |
| BMI | 2796 | 28.3 (26.3–31.6) | 1985 | 28.6 (26.4–31.6) | 4781 | 28.4 (26.3–31.6) |
| Nutritional status according to BMI | 2796 | 1985 | 4781 | |||
| Underweight or normal | 365 | 13.05 | 244 | 12.29 | 609 | 12.74 |
| Overweight | 1407 | 50.32 | 1010 | 50.88 | 2417 | 50.55 |
| Obesity | 1024 | 36.62 | 731 | 36.83 | 1755 | 36.71 |
| Disease duration in years | 1594 | 4 (1–7) | 1172 | 4 (1–7) | 2766 | 4 (1–7) |
| Disease duration by category | 1594 | 1172 | ||||
| <5 years | 807 | 50.63 | 606 | 51.71 | 1413 | 51.08 |
| 5 to 10 years | 657 | 41.22 | 472 | 40.27 | 1129 | 40.82 |
| >10 years | 130 | 8.16 | 94 | 8.02 | 224 | 8.1 |
| History of surgery | 2910 | 2061 | ||||
| Yes | 393 | 13.51 | 278 | 13.49 | 671 | 13.5 |
| No | 2517 | 86.49 | 1783 | 86.51 | 4300 | 86.5 |
| Joint localization | 280 | 203 | 483 | |||
| Shoulder | 1 | 0.36 | 0 | 0 | 1 | 0.21 |
| Hand | 15 | 5.36 | 10 | 4.93 | 25 | 5.18 |
| Hip | 9 | 3.21 | 10 | 4.93 | 19 | 3.93 |
| Knee | 253 | 90.36 | 182 | 89.66 | 435 | 90.06 |
| Spine | 1 | 0.36 | 1 | 0.49 | 2 | 0.41 |
| Foot | 1 | 0.36 | 0 | 0 | 1 | 0.21 |
| Pharmacologic treatment | 2910 | 2061 | 4971 | |||
| Yes | 1828 | 62.82 | 1319 | 64 | 3147 | 63.31 |
| No | 1082 | 37.18 | 742 | 36 | 1824 | 36.69 |
| Type of medication | ||||||
| Analgesics | 2910 | 2061 | 4971 | |||
| No | 1233 | 42.4 | 858 | 41.6 | 2091 | 42.1 |
| Yes | 1677 | 57.6 | 1203 | 58.4 | 2880 | 57.9 |
| NSAIDsa | 2910 | 2061 | 4971 | |||
| No | 1554 | 53.4 | 1024 | 49.7 | 2578 | 51.9 |
| Yes | 1356 | 46.6 | 1037 | 50.3 | 2393 | 48.1 |
| Corticosteroids | 2910 | 2061 | ||||
| No | 2855 | 98.1 | 2024 | 98.2 | 4879 | 98.2 |
| Yes | 55 | 1.9 | 37 | 1.8 | 92 | 1.8 |
| Supplements | 2910 | 2061 | ||||
| No | 2274 | 78.1 | 1617 | 78.5 | 3891 | 78.3 |
| Yes | 636 | 21.9 | 444 | 21.5 | 1080 | 21.7 |
| Analgesics/NSAIDs | 2910 | 2061 | ||||
| No | 2837 | 97.5 | 1997 | 96.9 | 4834 | 97.2 |
| Yes | 73 | 2.5 | 64 | 3.1 | 137 | 2.8 |
| Biomarkers | ||||||
| Glucose | 660 | 103 (92–128) | 539 | 106 (93–129) | 1199 | 104 (92–129) |
| Cholesterol | 447 | 191 (150–218) | 378 | 195.5 (144–221) | 825 | 193 (149–220) |
| Triglycerides | 366 | 170.5 (121–252) | 296 | 165 (128–277) | 662 | 168.5 (125–262) |
| Uric acid | 359 | 5 (3.8–6.3) | 324 | 5.1 (3.9–6.35) | 683 | 5 (3.8–6.3) |
| Morbidity | ||||||
| Comorbiditya | 2910 | 2061 | 4971 | |||
| No | 1514 | 52.0 | 991 | 48.1 | 2505 | 50.4 |
| Yes | 1396 | 48.0 | 1070 | 51.9 | 2466 | 49.6 |
| Diabetes | 2910 | 2061 | 4971 | |||
| No | 2325 | 79.9 | 1634 | 79.3 | 3959 | 79.6 |
| Yes | 585 | 20.1 | 427 | 20.7 | 1012 | 20.4 |
| Hypertensiona | 2910 | 2061 | 4971 | |||
| No | 1996 | 68.6 | 1345 | 65.3 | 3341 | 67.2 |
| Yes | 914 | 31.4 | 716 | 34.7 | 1630 | 32.8 |
| Dyslipidemia | 2910 | 2061 | 4971 | |||
| No | 2672 | 91.8 | 1872 | 90.8 | 4544 | 91.4 |
| Yes | 238 | 8.2 | 189 | 9.2 | 427 | 8.6 |
| Respiratory disease | 2910 | 2061 | ||||
| No | 2861 | 98.3 | 2025 | 98.3 | 4886 | 98.3 |
| Yes | 49 | 1.7 | 36 | 1.8 | 85 | 1.7 |
| Hyperuricemia | 2910 | 2061 | ||||
| No | 2883 | 99.1 | 2037 | 98.8 | 4920 | 99.0 |
| Yes | 27 | 0.9 | 24 | 1.2 | 51 | 1.0 |
| Gout | 2910 | 2061 | ||||
| No | 2903 | 99.8 | 2053 | 99.6 | 4956 | 99.7 |
| Yes | 7 | 0.2 | 8 | 0.4 | 15 | 0.3 |
| Healthcare | ||||||
| Institutiontypea | 2910 | 2061 | 4971 | |||
| Public | 396 | 13.6 | 332 | 16.1 | 728 | 14.6 |
| Social security | 833 | 28.6 | 577 | 28.0 | 1410 | 28.4 |
| Private | 1681 | 57.8 | 1152 | 55.9 | 2833 | 57.0 |
BMI=body mass index; IQR=interquantile range; NSAIDs=non-steroidal anti-inflammatory drugs.
Wilcoxon signed-rank test<0.001.
Regarding the type of health care, the patients belonged to, 14.6% belonged to public institutions, 28.4% to social security and the rest to private medical practice.
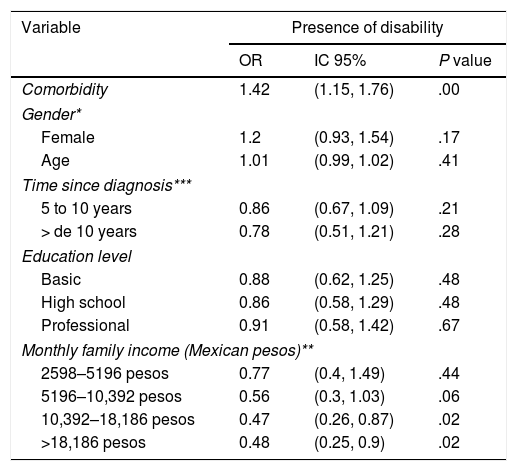
ModelFrom an adjusted model, we found that patients with OA with the presence of co-morbidity had a 42% higher probability of having disability (OR 1.42 [CI 95% (1.15–1.76) P=.001], adjusted for age, gender, economic income, time to diagnosis and education level (Table 3).
Factors associated with the presence of disability in patients with OA in Mexico, 2013–2015.
| Variable | Presence of disability | ||
|---|---|---|---|
| OR | IC 95% | P value | |
| Comorbidity | 1.42 | (1.15, 1.76) | .00 |
| Gender* | |||
| Female | 1.2 | (0.93, 1.54) | .17 |
| Age | 1.01 | (0.99, 1.02) | .41 |
| Time since diagnosis*** | |||
| 5 to 10 years | 0.86 | (0.67, 1.09) | .21 |
| > de 10 years | 0.78 | (0.51, 1.21) | .28 |
| Education level | |||
| Basic | 0.88 | (0.62, 1.25) | .48 |
| High school | 0.86 | (0.58, 1.29) | .48 |
| Professional | 0.91 | (0.58, 1.42) | .67 |
| Monthly family income (Mexican pesos)** | |||
| 2598–5196 pesos | 0.77 | (0.4, 1.49) | .44 |
| 5196–10,392 pesos | 0.56 | (0.3, 1.03) | .06 |
| 10,392–18,186 pesos | 0.47 | (0.26, 0.87) | .02 |
| >18,186 pesos | 0.48 | (0.25, 0.9) | .02 |
OR, Odds ratio adjusted for co variables: gender, age, education level (years), income, and time from diagnosis.
Reference category, male.
Reference category, less than 5 years since diagnosis*** Reference category, no formal education level **Reference category, income<2598 pesos.
Source: IMPACTAR database.
Additionally, patients with OA whose monthly family income was above $10,392 MXP, had 53% (OR 0.47 (CI 95% (0.26–0.87) P=.02) less probability of presenting disability when compared with patients with income below $2598 MXP, adjusted for gender, age, time from diagnosis, co-morbidity and education level (Table 3).
When analyzing WOMAC against the presence or absence of any co-morbidity, the median in the pain domain was 5.2 when a co-morbidity was present and 4.7 versus none (P=.001); for the morning stiffness dominion, the medians were 18 vs 1.7 respectively (P=.02); and for the function dominion medians were 27.9 vs 16.55 respectively (P=.001).
To evaluate the effect of having 2 or more comorbidities vs none or just 1, the medians for the WOMAC pain dominion were 5.3 vs 4.8 respectively (P=.001), for function 18.3 vs 16.3 respectively (P=.001) and for stiffness 1.8 vs 1.76 (P=.07). When analyzing the presence of 3 or more co-morbidities vs 0 to 2 of them, medians for pain were 5.5 vs 4.9 (P=.001), function 18.8 vs 17 (P=.001) and stiffness 1.8 vs 1.7 (P=.12). We found a nonparametric correlation (Rho Spearman) between the pain and the function WOMAC dominions in our patients (r=0.82).
DiscussionThe strength of this study is that it offers a global view of the current situation regarding OA patients when being attended by internal medicine, rheumatologists, and orthopedics specialists, whereas other studies exclude these patients or include only those being taken care of by primary care physicians. Furthermore, this analysis comes from a national registry of almost 5000 OA patients, the largest published so far. Our study reflects the characteristics of 4971 OA patients cataloged by 7 socioeconomic regions and different healthcare types and assesses the impact of co-morbidities toward disability through the WOMAC questionnaire. Regarding patient age and gender, our cohort showed similar results to other previously published studies.
Regarding the healthcare professionals that participated in the IMPACTAR study, we presented significant differences with studies previously done in Mexico,6,12 while Burgos et al. and the PANLAR study reported patients evaluated only by rheumatologists, the IMPACTAR initiative included patients evaluated by physicians from all medical specialties and subspecialties related to the management and treatment of OA which allows for a wider healthcare perspective.12
In our transversal study, 75% of our sample was comprised by women,25 which is in accordance with other studies of knee OA. It is also in accordance with community -based reports using the COPCORD methodology where the mean OA prevalence in Mexico is 10.5%, although some northern regions like Nuevo León reported 17.3% with also, female predominance. These results coincide with those found by Burgos et al., and others.5,12,26
Regarding the most affected anatomical site in different cohorts, in the IMPACTAR registry, 88% was the knee, a similar proportion reported by Burgos et al.,12 whereas in the PANLAR study the knee represented only 31%. These differences may be explained by the wider population diversity in the PANLAR study. Furthermore, there may be selection, diagnosis and referral bias, since due to its clinical characteristics, knee OA is easier to diagnose, and frequently requires orthopedic and rehabilitation evaluations and less care by rheumatologists, especially if it has already caused disability.
Another contrasting finding was disease latency; Burgos et al.12 reported a mean duration of 69 months, while in patients in the IMPACTAR registry was 48 months; this may be due to the heterogeneity of medical specialists that took care of patients in our cohort.
It is also worth noting that in the study by Burgos et al.,12 one quarter of patients had a low WOMAC score and minimal physical limitations despite the diagnosis. In our study, we observed that a larger number of patients (41.5%) from different regions had disability as measured by a WOMAC above or equal to 3, which reflects the type of population that is seen by medical specialists.
Previous OA cohorts in Mexico had not considered adjusting variables like socioeconomic income, education level, socioeconomic region or biochemical profile.6 We registered these variables and they were evaluated in the statistical model.
Some authors have found an association with two co -morbidities in patients with knee OA.25 In our study, 49.6% of patients had at least one comorbidity. We report a high prevalence of hypertension (HTN) (32.8%) in our population. Barquera et al.,27 in the 2006 national health survey, found an HTN prevalence of 31.5% (CI 95% 29.8–33.1) which coincides with our results.
A study done in Cuba by Friol GJ et al., found that half of patients referred co-morbidities associated with OA, with diabetes mellitus and obesity being the most frequent, either alone or combined; obesity was present in 13.5% of subjects and diabetes mellitus in 9%, even though almost 75% were above 60 years old.9
It is expected that when Body Mass Index (BMI) increases, the number of co-morbidities increases and physical activity decreases.28 In our study, average BMI was 28.3 (26.3–31.6) in patients with OA without disability and there was no significant difference to those who had disability.
The presence of disability was defined as a WOMAC function score ≥3 and was analyzed in a dichotomous manner. It is possible that the cutoff point does not discriminate adequately patients with different types of co-morbidities due to the low quantity of subjects with one severe disability for this cutoff point in the WOMAC scale. Nonetheless, the definition of disability was mostly designed toward detecting patients without disability.
The economic income in patients with disability was lower ($13 000 MXP) (IQR: 9000–16 000) adjusted to relevant co-variables like gender, age, time from diagnosis, co-morbidity and education level. This agrees with previously published data in other studies of musculoskeletal pain where socioeconomic privation has been described as a risk factor for pain in general as well as chronic pain.26,29,30 Also, the WOMAC pain dominion has been associated with poverty level. Data indicate that disability leads to poverty and poverty is associated with greater disability.29 We observed a statistically significant difference between patients with or without disability according to the type of institution they received care from, where the group with disability who were taken care for in public hospitals (16.1%) was higher in comparison to those without disability (13.6%), and this may be bound to the former.
We found that 48.1% of patients took NSAIDs, which is very similar to that observed in community-based studies where NSAIDs are the most frequently used medications (up to 60%).5,26 Moreover, we observed that patients who reported NSAID intake were more likely to be disabled (50.3%) which would reflect in a higher NSAID associated co-morbidity; however, we were unable to establish this association in this study.
Age, education level and time from OA diagnosis were not significantly associated with the presence of disability under an adjusted model, and this may be due to a large proportion of patients having a low education level. In Mexico, we still have low education levels, and in this study, we observed that half of OA patients had only basic schooling level (49.9%). Cleveland et al, found that the WOMAC functional domain and total scores were associated with schooling level, where OA patients with low education levels had more pain and worse function.
We report a significant nonparametric correlation (Rho=0.82) between the WOMAC pain and function dominions.
It is important to understand the disability process and characterize the changes that occur during its development and establish when it is reaching a critical point in order to incorporate preventive strategies; ideally, this would be during preclinical asymptomatic stages or early asymptomatic radiographic stages.
There are weaknesses in our study. One was that we did not evaluate the radiographic OA stage with disability nor the presence of comorbidities. Also, we only included patients that attend to hospitals or medical specialists and thus, it will not reflect the state of disability or presence of co -morbidities in the open population. We could not evaluate nor compare in our study if patients with OA and disability had more hospital admissions, out of pocket expenses, or if comorbidity decompensation resulted in more hospitalizations or physician office visits per year. We were unable to determine if the increased use of these medical services is due specifically to OA or other potential confounding factors.
ConclusionPatients with OA and presence of co-morbidity have almost a 50% more chance of having disability than those without co-morbidities. Regions in Mexico show different proportions of patients with disability, and a higher economic income was associated with a decreased risk of having disability. There is a need for programs and interventions to decrease disability in OA patients while taking in consideration co-morbidities, female gender, family economic income and geographic region origin as variables that are associated to disability in OA.
Funding informationColegio Mexicano de Ortopedia y Traumatología, through an unrestricted educational grant from the pharmacological company SANOFI. SANOFI did not participate in the elaboration of this manuscript or in data analysis presented.
Data confidentiality: The authors declare that they have followed the established protocols in their respective institutions in regards to patient data confidentiality, and that they have followed ethical guidelines or rules to publish with patient informed consent, and that all patients included in this study were provided with sufficient information about this study and gave their informed consent to participate.
Conflict of interestAll authors declare to have no conflicts of interest.
- •
Thanks to Collaborators and Co-investigators of the IMPACTAR Study Group (They are included in Annex 1).
- •
Thanks to Edgar Leonel Gonzalez Gonzalez PhD, Researcher at Mexico's National Institute of Public Health, and to Diana Molina Velez, M.Sc., and also to Concepción Garcia, Master in Public Health from the National Institute of Public Health for their help in the statistical analysis of the Database of the IMPACTAR initiative.