Improving referral of patients with back pain to rheumatologists could accelerate the diagnosis of axial spondyloarthritis. The RADAR study compared two strategies in the referral of patients with chronic back pain (>3 months) with an onset before the age of 45 years from primary care centers to rheumatology departments, in relation to the diagnosis of axial spondyloarthritis.
Patients and methodsEach primary care center was assigned a referral strategy for its patients: (a) strategy 1, patients who had one of the 3 following criteria: inflammatory back pain, HLA-B27 positivity or sacroiliitis in imaging; or (b) strategy 2, patients who had 2 of the following 6: inflammatory back pain, HLA-B27 positivity, sacroiliitis in imaging, family history of axial spondyloarthritis, extra-articular manifestations or good response to nonsteroidal antiinflammatory drugs. The rheumatologist established the final diagnosis.
ResultsEighty-eight Spanish patients (mean age 36.8 years [SD 8.7], 55.7% females and 44.3% males) were referred for evaluation, 60 patients under strategy 1 and 28 under strategy 2. A definitive diagnosis of axial spondyloarthritis was established in 25.4% with strategy 1 and in 28.6% with strategy 2 (P=NS). Inflammatory back pain was the criterion most commonly used for referral, and the agreement rate between the primary care physician and rheumatologist was 75%.
ConclusionsA simple referral strategy based on one of three criteria proved as effective as a strategy based on two of six criteria in diagnosing axial spondyloarthritis. Inflammatory back pain was the criterion most commonly used for patient referral.
Mejorar la derivación de pacientes con dolor lumbar a reumatología podría acelerar el diagnóstico de la espondiloartritis axial. El estudio RADAR comparó 2 estrategias de derivación de pacientes con dolor lumbar crónico (> 3 meses) de inicio antes de los 45 años desde atención primaria a reumatología con respecto al diagnóstico de espondiloartritis axial.
Pacientes y métodosSe asignó una estrategia a cada centro de salud para derivar a sus pacientes: (a) estrategia 1, si cumplían uno de los siguientes 3 criterios: dolor lumbar inflamatorio, HLA-B27 positivo o sacroilitis en prueba de imagen; (b) estrategia 2, si cumplían 2 de 6: dolor lumbar inflamatorio, HLA-B27 positivo, sacroilitis en prueba de imagen, historia familiar de espondiloartritis axial, manifestaciones extraarticulares y buena respuesta a antiinflamatorios no esteroideos. El reumatólogo estableció el diagnóstico final.
ResultadosOchenta y ocho pacientes (edad 36,8 años [DE 8,7]; 55,7% mujeres y 44,3% hombres) en España fueron derivados, 60 usando la estrategia 1 y 28 la estrategia 2. El diagnóstico de espondiloartritis axial definitiva se realizó en el 25,4% de los pacientes en la estrategia 1 y en el 28,6% en la estrategia 2 (p = NS). El dolor lumbar inflamatorio fue el criterio de derivación más utilizado y la concordancia entre médico de atención primaria y reumatólogo fue del 75%.
ConclusionesUna estrategia de derivación sencilla, basada en uno de 3 criterios, fue igual de eficaz que una estrategia basada en 2 de 6 criterios para el diagnóstico de espondiloartritis axial. El dolor lumbar inflamatorio fue el criterio más utilizado para la derivación.
Axial spondylitis is an inflammatory disease that primarily affects the spinal column and has a worldwide prevalence of 0.5%–1% including1,2 earlier stages of disease. The paradigmatic expression of the disease is ankylosing spondylitis (AS). Although in its early stages it may predominantly affect the sacroiliac joints, disease progression produces vertebral involvement at all levels.1,3,4
It is a known fact that axial spondyloarthritis usually starts insidiously at an early age (before 40 years) with chronic back pain and between 7 and 9 years pass before the onset of symptoms establishing a correct etiologic diagnosis.5,6 In our country, the REGISPONSER study showed that the diagnosis of AS was made with an average delay of 8 years from the onset of symptoms.7 This delay in diagnosis also involves a delay in establishing the most appropriate treatment for each patient, and the adverse consequences of untreated disease can decrease the quality of life of patients, causing prolonged work disability and increase the economic burden of the disease.8
The axial spondyloarthritis and AS may be diagnosed using a series of clinical, radiological and laboratory tests accessible to rheumatology clinics1,9 and, therefore, early referral of patients with axial symptoms to rheumatology clinics can reduce the time delay in diagnosis and allow proper treatment of the patient in an early stage.10
The aim of the Recognizing And Diagnosing Ankylosing Spondylitis Reliably (RADAR) study was to determine whether a simple derivation strategy for patients with chronic low back pain to rheumatology clinics was similar to a strict strategy to identify patients with a final diagnosis of axial spondyloarthritis.11 Here we report the results of the sample of patients included in Spain.
MethodsThe RADAR study is a multicenter, multinational study in which young patients with chronic low back pain were randomly distributed to one of two strategies. The primary objective of the study was to compare the two strategies of referral of patients with chronic low back pain from primary care rheumatology clinics regarding the final diagnosis of axial spondyloarthritis.11 Other objectives were to assess the usefulness of each criterion, exploring what referral criteria showed the highest yield for the diagnosis of axial spondyloarthritis, assessed according to what criteria determined whether patients were derived, and the degree of agreement between the primary care physician and the rheumatologist in the presence each criterion.
To do this, centers from 16 countries (8 centers in Spain) with networks that included primary care centers for referral and diagnosis of patients with low back pain potentially affected by axial spondyloarthritis were selected. The centers included patients with the following characteristics: (1) chronic back pain (more than 3 months) of unknown origin, (2) age at onset of pain<45 years, and (3) no previous diagnosis of axial spondyloarthritis or AS.10 Each center was assigned by a randomization ratio 1:1, a strategy for referring these patients to rheumatology clinics so that each health center referred all patients with a single strategy. Centers assigned to referral strategy 1 sent patients if they met one of the following three criteria: inflammatory back pain, HLA-B27 positive or sacroiliitis on imaging test. Centers assigned to referral strategy 2 sent patients if they met two of the following six criteria: inflammatory back pain, HLA-B27, sacroiliitis on imaging test, family history of axial spondyloarthritis, extra-articular manifestations and a good response to NSAIDs.
The rheumatologist established the final diagnosis of the patients referred after conducting additional testing if deemed relevant, and this was the patient's final diagnosis. With the final diagnosis, patients were classified as definite axial spondyloarthritis (radiographic or non radiographic), possible axial spondyloarthritis (suspected cases without definitive diagnosis) or no axial spondyloarthritis.
The study included a total of 1072 patients, 1049 of whom completed the study.11 In Spain we included 88 patients, of whom 87 completed the study and are included in this article.
The primary study analysis compared the proportion of patients with a final diagnosis of definite axial spondyloarthritis taking into account both strategies. For the primary analysis a binomial test was used for the difference in the percentage of patients with a final diagnosis of axial spondyloarthritis. The degree of agreement between the primary care physician and the rheumatologist was based on the presence of each criterion individually assessed by the percentage of patients referred due to a particular positive criterion according to the primary care physician and with whom the rheumatologist agreed positivitively.
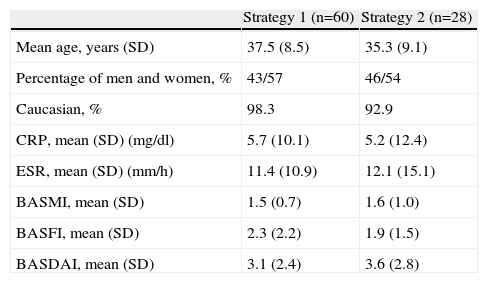
ResultsPatient CharacteristicsIn Spain we included 88 patients (60 patients were referred with strategy 1 and 28 with strategy 2), of which 87 completed the study (one patient of strategy 1 was lost to follow-up). The average age of the patients was 36.8 years (SD 8.7), 55.7% were female and 44.3% male. No demographic differences were observed in patients assigned to any of the 2 strategies (Table 1).
Baseline Characteristics of Patients.
| Strategy 1 (n=60) | Strategy 2 (n=28) | |
| Mean age, years (SD) | 37.5 (8.5) | 35.3 (9.1) |
| Percentage of men and women, % | 43/57 | 46/54 |
| Caucasian, % | 98.3 | 92.9 |
| CRP, mean (SD) (mg/dl) | 5.7 (10.1) | 5.2 (12.4) |
| ESR, mean (SD) (mm/h) | 11.4 (10.9) | 12.1 (15.1) |
| BASMI, mean (SD) | 1.5 (0.7) | 1.6 (1.0) |
| BASFI, mean (SD) | 2.3 (2.2) | 1.9 (1.5) |
| BASDAI, mean (SD) | 3.1 (2.4) | 3.6 (2.8) |
BASDAI, Bath Ankylosing Spondylitis Disease Activity Index; BASFI, Bath Ankylosing Spondylitis Functional Index; BASMI, Bath Ankylosing Spondylitis Metrology Index; SD, standard deviation; CRP C, reactive protein; ESR, erythrocyte sedimentation rate.
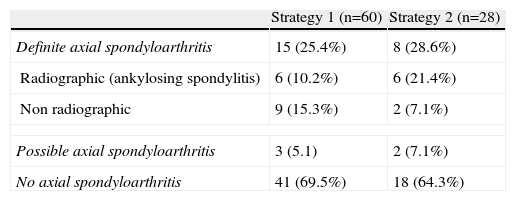
No differences were seen in the final diagnoses issued by rheumatologists between both strategies. The definitive diagnosis of axial spondyloarthritis was performed in 25.4% (n=15) patients of strategy 1 and 28.6% (n=8) of Strategy 2 (P=NS). There were no differences in the percentage of patients in which the axial spondyloarthritis considered as ruled out. The final diagnosis of the patients is shown in Table 2.
Final Diagnosis of Patients in Each Referral Strategy (P=NS for all Comparisons).
| Strategy 1 (n=60) | Strategy 2 (n=28) | |
| Definite axial spondyloarthritis | 15 (25.4%) | 8 (28.6%) |
| Radiographic (ankylosing spondylitis) | 6 (10.2%) | 6 (21.4%) |
| Non radiographic | 9 (15.3%) | 2 (7.1%) |
| Possible axial spondyloarthritis | 3 (5.1) | 2 (7.1%) |
| No axial spondyloarthritis | 41 (69.5%) | 18 (64.3%) |
One patient from strategy 1 was not evaluated.
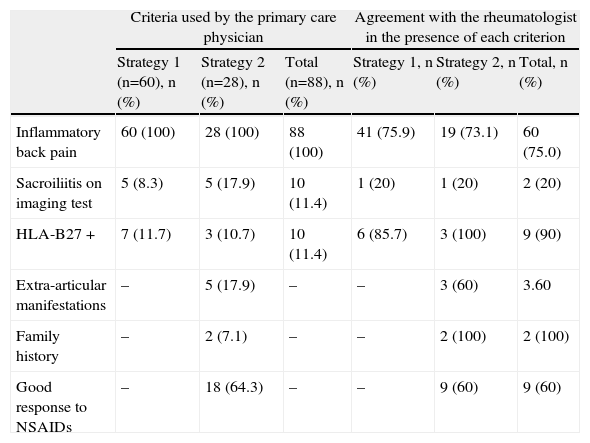
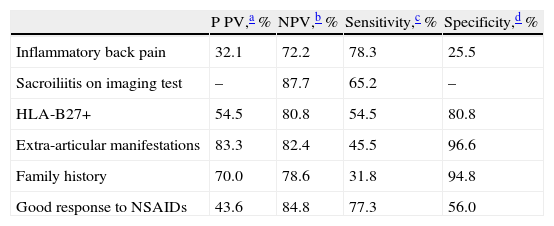
Inflammatory back pain was the criterion most used to refer the patient (100% of patients in both strategies). In strategy 2, the response to NSAIDs was used for 18 patients (64.3%), while the other criteria were seldom used (Table 3). In inflammatory back pain (n=88), the agreement of the rheumatologist in the presence of inflammatory back pain was 75%. The agreement was also high for the presence of HLA-B27 positivity (90%), but was low for the presence of sacroiliitis on imaging techniques (20%) although these criteria were seldomly employed by the primary care physician (Table 3). The most sensitive referral criteria were inflammatory back pain (78.3%) and a good response to NSAIDs (77.3%), while all had a high negative predictive value, especially sacroiliitis and a good response to NSAIDs (Table 4).
Criteria Used by the Primary Care Physician for Referral, and Agreementa With the Rheumatologist in the Presence of Each Criterion.
| Criteria used by the primary care physician | Agreement with the rheumatologist in the presence of each criterion | |||||
| Strategy 1 (n=60), n (%) | Strategy 2 (n=28), n (%) | Total (n=88), n (%) | Strategy 1, n (%) | Strategy 2, n (%) | Total, n (%) | |
| Inflammatory back pain | 60 (100) | 28 (100) | 88 (100) | 41 (75.9) | 19 (73.1) | 60 (75.0) |
| Sacroiliitis on imaging test | 5 (8.3) | 5 (17.9) | 10 (11.4) | 1 (20) | 1 (20) | 2 (20) |
| HLA-B27 + | 7 (11.7) | 3 (10.7) | 10 (11.4) | 6 (85.7) | 3 (100) | 9 (90) |
| Extra-articular manifestations | – | 5 (17.9) | – | – | 3 (60) | 3.60 |
| Family history | – | 2 (7.1) | – | – | 2 (100) | 2 (100) |
| Good response to NSAIDs | – | 18 (64.3) | – | – | 9 (60) | 9 (60) |
NSAID, nonsteroidal anti-inflammatory drugs; HLA, human leukocyte antigen.
Predictive Values, Sensitivity and Specificity of Each Individual Referral Criterion.
| P PV,a % | NPV,b % | Sensitivity,c % | Specificity,d % | |
| Inflammatory back pain | 32.1 | 72.2 | 78.3 | 25.5 |
| Sacroiliitis on imaging test | – | 87.7 | 65.2 | – |
| HLA-B27+ | 54.5 | 80.8 | 54.5 | 80.8 |
| Extra-articular manifestations | 83.3 | 82.4 | 45.5 | 96.6 |
| Family history | 70.0 | 78.6 | 31.8 | 94.8 |
| Good response to NSAIDs | 43.6 | 84.8 | 77.3 | 56.0 |
NSAIDs, non steroidal anti-inflammatory drugs; HLA, human leukocyte antigen; NPV, negative predictive value; PPV, positive predictive value.
Percentage of patients assessed as positive for the criteria that were diagnosed with definite axial spondyloarthritis.
Percentage of patients assessed as negative for the criteria who were not diagnosed with definite axial spondyloarthritis.
The analysis of the patients included in the RADAR study in Spain shows that both referral strategies led to a similar percentage of diagnoses of definite axial spondyloarthritis (25.4% and 28.6% respectively). The simplest referral strategy (one of three criteria) had a similar efficacy as the more complex strategy (two of six criteria) for the diagnosis of this disease.
The sample data included in Spain was consistent with the overall study data, which included 1072 patients, which showed a percent of definitive axial spondyloarthritis diagnosis of 37.8% and 35.6% respectively.11 The percentage of patients diagnosed with definite axial spondyloarthritis in Spain compared to the overall sample was slightly lower. This is due to the inclusion in some of the participating countries of patients with more symptoms and activity (expressed by parameters such as BASDAI, BASFI, BASMI, higher CRP and ESR) in which the percentage with a final diagnosis of definite axial spondyloarthritis was higher. The results are also in line with a recent study carried out in Germany with 2 very similar referral strategies.12
Randomization was performed by study sites (each site referred patients according to one approach) and this is the reason for the difference in sample size of two strategies (60 and 28 patients, respectively), since the centers assigned to strategy 2 recruited fewer patients. In the Spanish sample, inflammatory back pain was used as a criterion for referral for all patients, and the correlation between primary care physicians and rheumatologists was relatively high (75%). This was also the main criterion for referral in the overall sample. In patients in Spain, sacroiliitis and other referral criteria were used rarely. Furthermore, the observed agreement for the diagnosis of sacroiliitis on imaging tests was particularly low in the Spanish sample (20%), with respect to the overall sample (64.2%). This, coupled with the low availability of HLA-B27 in primary care, suggests that LBP of inflammatory characteristics should be the main criterion for referral of early diagnosis cases. The high sensitivity and negative predictive value of inflammatory back pain in the study, important requirements for a test to be useful for screening patients, together with the fact that it is a purely clinical assessment, support its usefulness as a criterion of suspicion and referral.
Today, a patient typically waits between 7 and 9 years from the start of symptoms to having an established diagnosis of AS,5–7 but in the early stages, even without changes on conventional imaging, the disease burden for patient is similar in terms of symptoms and constraints.13 Several studies in Spain have shown that the implementation of protocols for suspected spondyloarthritis improves early diagnosis of this disease.14,15 It is of particular interest to note that in studies in which the disease is actively looked for there is always a significant percentage of patients with low back pain with axial spondyloarthritis who were not previously identified, hence the importance of correct interpretation of lumbar inflammatory pain. In this regard, the Assessment of Spondyloarthritis International Society (ASAS) and the European Study Group for Spondyloarthropathy (ESSG) have issued simple definitions based on inflammatory back pain onset before 40 years (45 in the case of ESSG), improvement with exercise and no improvement with rest, the insidious onset and the presence of pain at night.16,17 In the RADAR study the age of cutoff was before 45 years, which can probably help detect the disease in patients with late onset forms more often.
The main limitation of the study is that, since the analysis was made on a small group of patients (those recruited in Spain), the statistical power is insufficient to draw firm conclusions. For this reason, the data are for descriptive purposes only. The main interest is to show the situation in our country. The fact that of 88 patients included in the study in Spain just over a quarter (23 patients) were diagnosed with definite axial spondyloarthritis by the rheumatologist suggested that there should be more intense training for suspicion of this entity in primary care, and that we should improve the referral of these patients to rheumatology for early diagnosis and treatment.
In summary, the analysis of patients in Spain included in the RADAR study is in line with the results in the overall study population and shows that, in patients with chronic back pain, a simple strategy for referral to rheumatology based primarily on the presence of inflammatory low back pain is as effective as a more conservative approach (two of six criteria) for diagnosing axial spondyloarthritis. Furthermore, the correlation in the diagnosis of inflammatory back pain between primary care physician and rheumatologist was reasonably good. Applying a simple referral protocol, based on the identification of inflammatory back pain may accelerate the diagnosis of these patients and the establishment of appropriate treatment, thereby minimizing the current burden of axial spondyloarthritis currently.
Ethical ResponsibilitiesProtection of people and animalsThe authors state that no experiments were performed on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients and all patients included in the study have received sufficient information and gave their written informed consent to participate in this study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the author of correspondence.
Conflict of InterestsBerta Julia and Luis Cea-Calvo are full-time employees at Merck Sharp & Dohme of Spain. The rest of the authors received financial compensation for participation in the study. Dr. Eduardo Collantes is a member of the Advisory Board of Pfizer, and has received a grant from Merck Sharp & Dohme.
The study Recognizing And Diagnosing Ankylosing Spondylitis Reliably (RADAR) was funded by Schering-Plough (now Merck & Co., Whitehouse Station, New Jersey, USA). The study involved researchers from 16 countries. We thank the coordinators consent to the publication of local data.
Dr. Jose Luis Fernandez-Sueiro died in the period in which this manuscript was in review. We want to recognize his work in this study and manuscript and to show the deepest gratitude for all his teachings.
Please cite this article as: Juanola X, et al. Comparación de 2 estrategias de derivación en el diagnóstico de la espondiloartritis axial en España. Estudio RADAR. Reumatol Clin. 2013;9:348–352.