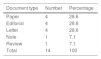
A search in Scopus – the largest database of abstracts and citations in peer reviewed scientific journals in the world – shows that from 1990 to June 2018 the number of papers on the subject of consent for the publication of case reports (CPCR) amounted to 14 documents.1–14 Of this total, only four were peer reviewed papers published in indexed journals, as is shown in Table 1.
Consent documents for publication in published case reports 1990–2018.
| Document type | Number | Percentage |
|---|---|---|
| Paper | 4 | 28.6 |
| Editorial | 4 | 28.6 |
| Letter | 4 | 28.6 |
| Note | 1 | 7.1 |
| Review | 1 | 7.1 |
| Total | 14 | 100 |
Within the sample analysed, such a small number of results clearly shows the relevance of the paper: “The Patient Information Sheet (PIS) and Informed Consent (IC) for case reports and case series: Proposal for a standard model for presentations in congresses and other scientific publications”, published by Juana Cruz del Río, Isabel Sastre Gervás and Susana Romero Yuste, * in this edition of Clinical Rheumatology.
The authors propose a digital format as the bioethical support for: (1) the description of case reports and case series in conferences; (2) publication in journals that lack their own model, and (3) undertaking teaching activities in the health sector. With their proposal the authors seeks to comply with the right to privacy and the protection of patient data used in research in Spain.
This paper is not only relevant, as it is also opportune given that several medical journals have gradually ceased to publish case reports. They state that studies of this type affect levels of impact as they lack quality standards, are quoted very infrequently and fail to comply with the ethical standards governing clinical research. The work presented here aims to correct these deficiencies to a certain degree.
Some challenges for Latin AmericaDuring the second half of the 20th century it became obligatory in several Western countries to revise the ethical aspects of experiments undertaken in human beings.15
Until 1966 medical research was routinely performed without seeking any type of consent from the patients subjected to research.16 As a part of developments in the this field, in 1996 the first paper and guides were published by the International Committee of Medical Journal Editors on CPCR.14
In spite of the progress made since then many challenges remain in this field, particularly in developing countries, where research ethics committees either do not exist or are in a precarious situation.
Given that consent depends on the context, this problem has to weigh sociocultural factors such as the age of participants, their educational level, language differences, coercion and the influence of patriarchal or traditional societies.17
The CPCR developed in Latin American countries also have to take into account the fact that sometimes researchers have to deal with highly vulnerable populations including children, women, the elderly, individuals with mental development disorders,18 illegal immigrants and native populations.
Within all of these contexts, guaranteeing the rights of research subjects who are illiterate, disabled or speakers of native languages, for example, usually requires the additional presence of an independent witness, a tutor or a translator to confirm that consent was given consciously and freely.
All of these considerations have to be taken into account when obtaining a CPCR, with the aim of minimising asymmetries between researchers and research subjects.19
The duty of rheumatologists to protect personal rights and dignityTo summarise: the CPCR, which has the aim of protecting research subjects against possible harm and exploitation during the publication of a study, must be contextualised within the sociocultural reality in each nation, especially when research to be published consists of a case report or case series in rural, marginalised or very poor communities.
In any case it must never be forgotten that in medical research projects undertaken by rheumatologists respect for the privacy, rights and intrinsic dignity of individuals is expressed by components such as the CPCR.
The above considerations mean that constant, respectful and fluid dialogue and communication are necessary between researchers, patients and their associations, regulatory bodies, health institutions and scientific journals. This has to be strengthened by suitable and solid bioethical training in undergraduate and graduate courses.20,21
Conflict of interestsThe authors have no conflict of interests to declare, and they have received no financing.
Please cite this article as: Pineda C, Sandoval H. Consentimiento para publicación de casos clínicos en Reumatología. Reumatol Clin. 2018;14:181–182.