To develop recommendations for the management of methotrexate (MTX) in psoriatic arthritis (PsA), based on best evidence and experience.
MethodsA group of 12 experts on MTX use was selected. The coordinators formulated 14 questions about the use of MTX in PsA patients (indications, efficacy, safety and cost-effectiveness). A systematic review was conducted to answer the questions. Using this information, inclusion and exclusion criteria were established, as were the search strategies (Medline, EMBASE and the Cochrane Library were searched). Two different reviewers selected the articles. Evidence tables were created. At the same time, European League Against Rheumatism and American College of Rheumatology abstracts were evaluated. Based on this evidence, the coordinators proposed 12 preliminary recommendations that the experts discussed and voted on in a nominal group meeting. The level of evidence and grade of recommendation were established using the Oxford Center for Evidence Based Medicine and the level of agreement with the Delphi technique (two rounds). Agreement was established if at least 80% of the experts voted yes (yes/no).
ResultsA total of 12 preliminary recommendations on the use of MTX were proposed, 9 of which were accepted. One was included in a different recommendation and other two were not voted on and were thereafter clarified in the main text.
ConclusionsThese recommendations aim to answer frequent questions and help in decision making strategies when treating PsA patients with MTX.
Desarrollar recomendaciones sobre el uso de metotrexato (MTX) en pacientes con artritis psoriásica (APs) basadas en la mejor evidencia y experiencia.
MétodosSe seleccionó un grupo de 12 expertos reumatólogos en el manejo de MTX. Los coordinadores generaron 14 preguntas sobre el uso de MTX en pacientes con APs (perfiles de indicación, eficacia y seguridad) para ser contestadas mediante una revisión sistemática de la literatura. En función de las preguntas se definieron los criterios de inclusión y exclusión y las estrategias de búsqueda (para interrogar Medline, Embase y la Cochrane Library). Dos revisores seleccionaron los artículos resultantes de la búsqueda. Se generaron tablas de evidencia. Paralelamente se evaluaron abstracts de congresos de EULAR y ACR. Con toda esta evidencia los coordinadores generaron 12 recomendaciones preliminares que se evaluaron, discutieron y votaron en una reunión de grupo nominal con el resto de expertos. Para cada recomendación se estableció el nivel de evidencia, grado de recomendación, y grado de acuerdo mediante un Delphi. Se definió acuerdo si al menos el 80% de los participantes contestan sí a la recomendación (sí o no).
ResultadosDe las 12 recomendaciones preliminares se aceptaron 9 recomendaciones sobre el uso de MTX en la APs. Una se englobó en otra y otras 2 no se llegaron a votar porque se decidió no incluirlas, pero se comentan en el texto final.
ConclusionesEstas recomendaciones pretenden resolver algunos interrogantes clínicos habituales y facilitar la toma de decisiones con el uso de MTX en la APs.
Psoriatic arthritis (PsA) is a chronic inflammatory disease that commonly affects patients with psoriasis. The prevalence of psoriasis is around 2%–3% of the general population,1 and 20%–30% of those patients will develop PsA.2 Musculoskeletal involvement in PsA can be highly varied, including the axial skeleton, peripheral joints, enthesitis and dactylitis.3 The course of this disease is also variable, there being very aggressive forms, with considerable joint damage and disability.2,4
Concerning treatment, there are now a number of drugs, both for the skin manifestations and the musculoskeletal involvement, that pursue the complete control of the inflammation and an improvement in the quality of life of the patients.5,6
Despite the broad consensus on the efficacy of methotrexate (MTX) in PsA in clinical practice, its inclusion as the preferred disease-modifying antirheumatic drug (DMARD) in the recommendations of the European League Against Rheumatism (EULAR)7 and the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA),8 and its widespread use among rheumatologists, the scientific evidence is limited in certain aspects. Moreover, in the setting of spondyloarthritides (including PsA), in Spain, we have observed a great variability in the use of DMARDs, including MTX.9
Taking into account the above uncertainties, the objective of the present report is to draw up recommendations, based on the best possible evidence and experience, concerning the use of MTX in PsA patients.
MethodsFor building consensus, we followed the nominal group and Delphi method. The preparation of the document involved the distribution of tasks and comments to the participants, with the aid of a systematic literature review (SLR) and of a methodologist.
First, we established a group of 12 experts, representing all of the geographic areas of Spain. They had demonstrated experience in the management of patients with PsA and in the use of MTX. For their selection, we performed a search in MEDLINE that identified Spanish rheumatologists with publications on the subject of the present document, as well as related works submitted to the meeting of the Spanish Society of Rheumatology (SER).
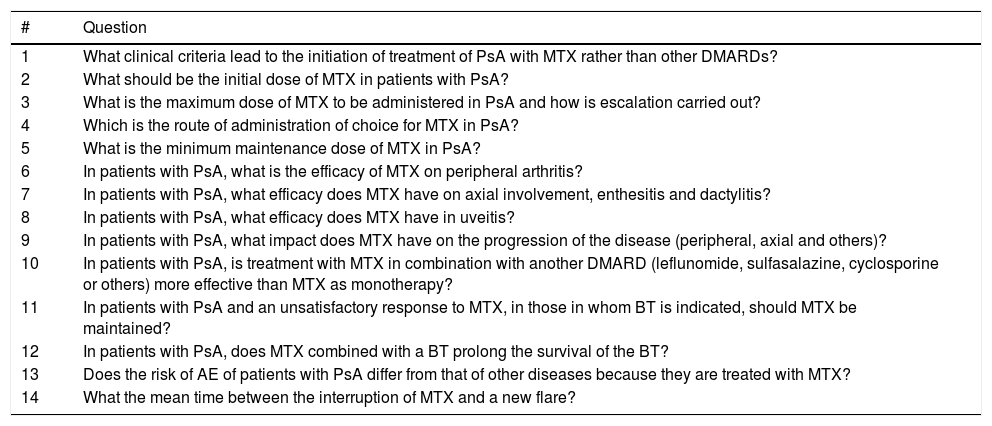
Systematic Literature ReviewThe 2 coordinators of the project provided 14 questions. Given their characteristics, it was seen that they could be responded to with a single SLR (Table 1). With these questions, we defined the criteria for inclusion and exclusion. We searched for articles that involved PsA patients being treated with MTX, regardless of the dose and route of administration. These studies should analyze distinct aspects of the efficacy and safety of the drug treatment. Finally, we included only studies with the following designs: meta-analyses, systematic reviews, randomized controlled trials (RCTs), nonrandomized studies with a valid comparator group and observational studies (prospective, retrospective and cross-sectional). We searched the following bibliographic databases: MEDLINE (from inception to July 2016), EMBASE (from inception to July 2016) and Cochrane Library (from inception to July 2016). We used MeSH terms and free text, and the search was performed with the help of an expert informationist. For each review, two reviewers (EL and TO) independently analyzed the articles returned in the search of the different bibliographic databases, and prepared a detailed analysis of the included articles. In the case of discrepancy, the difference was resolved by a third person (LC). We reviewed the gray literature from the EULAR and American College of Rheumatology meetings of the preceding 2 years, as well as documentation provided by the coordinator (articles and abstracts from congresses and other forums of interest).
Questions Formulated by the Coordinators.
| # | Question |
|---|---|
| 1 | What clinical criteria lead to the initiation of treatment of PsA with MTX rather than other DMARDs? |
| 2 | What should be the initial dose of MTX in patients with PsA? |
| 3 | What is the maximum dose of MTX to be administered in PsA and how is escalation carried out? |
| 4 | Which is the route of administration of choice for MTX in PsA? |
| 5 | What is the minimum maintenance dose of MTX in PsA? |
| 6 | In patients with PsA, what is the efficacy of MTX on peripheral arthritis? |
| 7 | In patients with PsA, what efficacy does MTX have on axial involvement, enthesitis and dactylitis? |
| 8 | In patients with PsA, what efficacy does MTX have in uveitis? |
| 9 | In patients with PsA, what impact does MTX have on the progression of the disease (peripheral, axial and others)? |
| 10 | In patients with PsA, is treatment with MTX in combination with another DMARD (leflunomide, sulfasalazine, cyclosporine or others) more effective than MTX as monotherapy? |
| 11 | In patients with PsA and an unsatisfactory response to MTX, in those in whom BT is indicated, should MTX be maintained? |
| 12 | In patients with PsA, does MTX combined with a BT prolong the survival of the BT? |
| 13 | Does the risk of AE of patients with PsA differ from that of other diseases because they are treated with MTX? |
| 14 | What the mean time between the interruption of MTX and a new flare? |
AE, adverse event; BT, biological therapy; DMARDs, disease-modifying antirheumatic drugs; MTX, methotrexate; PsA, psoriatic arthritis.
Subsequently, we performed a secondary hand-search of the reference lists of the articles that were ultimately included. To evaluate the methodological quality of the included reports, we utilized the Jadad scale for clinical trials and that of the Oxford Center for Evidence-Based Medicine for the remaining designs. We created evidence tables and tables showing the results that describe the main characteristics and findings of the included studies.
Nominal Group Meeting and DelphiThe group of experts held a nominal group meeting, once they were provided with the results of the SLR, together with the major conclusions concerning each question on the basis of the evidence encountered. During the meeting, the recommendations and the evidence were presented and discussed.
After that, the definitive recommendations were formulated and were subjected to Delphi voting, utilizing a system of electronic voting. Agreement was considered to be reached if at least 80% of the participants responded “yes” to the recommendation. The recommendations with a level of agreement (LOA) of less than 80% were reevaluated and, if necessary, were rewritten and voted in a second round.
Final Consensus DocumentThe final document was based on the literature review and the decisions of the nominal group. Each recommendations, with the aid of the methodologist, was assigned a level of evidence (LOE) and a grade of recommendation (GOR), in accordance with the recommendations for evidence-based medicine of the Center for Evidence-Based Medicine in Oxford, United Kingdom. The assignment of the LOA was carried out as was reported above. The document was circulated among the experts for their final evaluation and concluding comments.
Throughout the document, we speak of MTX in generic terms, that is, including the oral, subcutaneous and intramuscular routes. Generally, this term is applied to the oral route, which is that most widely utilized in clinical practice.
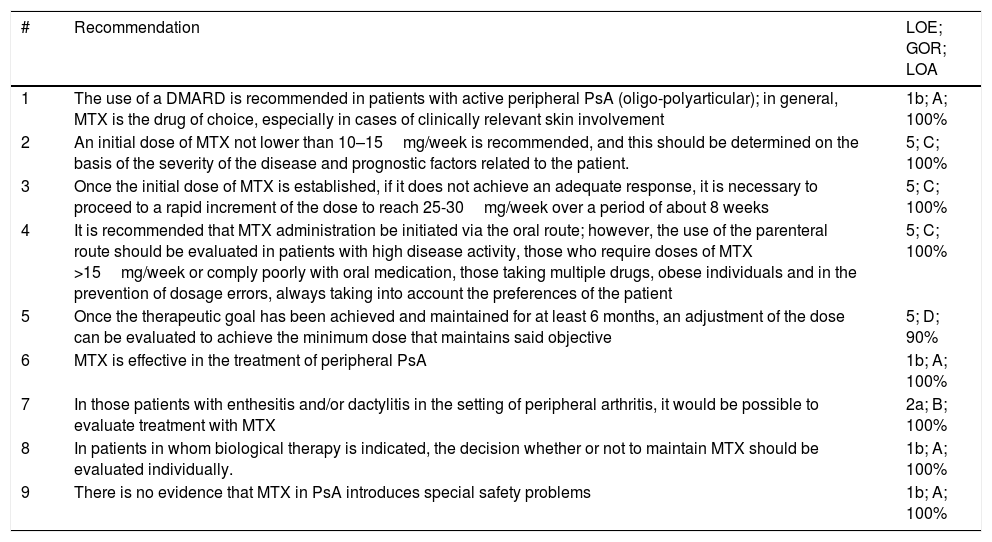
ResultsThe search identified a total of 1124 articles, 297 of which were duplicates. In all, 827 references were evaluated by title and abstract, and 111 remained to be read in detail, while the hand search added another 16 articles. After the detailed reading, 72 reports were eliminated, most of them due to their design or because they did not provide specific data on MTX. The SLR ultimately included 52 articles. Of the 12 preliminary recommendations, 9 were accepted and underwent the voting (see Table 2 for the detailed results of the Delphi round). One preliminary recommendation was included in another, and another 2 were not voted on as it was decided not to include them, but they are commented on the text. The questions, recommendations and available evidence regarding each question are described below.
Definitive Recommendations With Their Level of Evidence (LOE), Grade of Recommendation (GOR) and Level of Agreement (LOA).
| # | Recommendation | LOE; GOR; LOA |
|---|---|---|
| 1 | The use of a DMARD is recommended in patients with active peripheral PsA (oligo-polyarticular); in general, MTX is the drug of choice, especially in cases of clinically relevant skin involvement | 1b; A; 100% |
| 2 | An initial dose of MTX not lower than 10–15mg/week is recommended, and this should be determined on the basis of the severity of the disease and prognostic factors related to the patient. | 5; C; 100% |
| 3 | Once the initial dose of MTX is established, if it does not achieve an adequate response, it is necessary to proceed to a rapid increment of the dose to reach 25-30mg/week over a period of about 8 weeks | 5; C; 100% |
| 4 | It is recommended that MTX administration be initiated via the oral route; however, the use of the parenteral route should be evaluated in patients with high disease activity, those who require doses of MTX >15mg/week or comply poorly with oral medication, those taking multiple drugs, obese individuals and in the prevention of dosage errors, always taking into account the preferences of the patient | 5; C; 100% |
| 5 | Once the therapeutic goal has been achieved and maintained for at least 6 months, an adjustment of the dose can be evaluated to achieve the minimum dose that maintains said objective | 5; D; 90% |
| 6 | MTX is effective in the treatment of peripheral PsA | 1b; A; 100% |
| 7 | In those patients with enthesitis and/or dactylitis in the setting of peripheral arthritis, it would be possible to evaluate treatment with MTX | 2a; B; 100% |
| 8 | In patients in whom biological therapy is indicated, the decision whether or not to maintain MTX should be evaluated individually. | 1b; A; 100% |
| 9 | There is no evidence that MTX in PsA introduces special safety problems | 1b; A; 100% |
DMARD, disease-modifying antirheumatic drug; mg, milligram; MTX, methotrexate; PsA, psoriatic arthritis.
Recommendation 1. The use of a DMARD is recommended in patients with active peripheral PsA (oligo-polyarticular) (LOE 1b; GOR A; LOA 100%); in general, MTX is the drug of choice, especially in cases of clinically relevant skin involvement.
We found no articles defining the clinical criteria that lead to the use of MTX, rather than another DMARD. On the other hand, there is very extensive experience with MTX in rheumatology in distinct chronic diseases, and it is the drug of choice in many of them.10,11 Moreover, MTX is effective in cutaneous psoriasis.12
Regarding the evidence on the efficacy of MTX in PsA, the RCT that we analyzed are highly heterogeneous and have variable quality. They include various profiles of PsA patients (MTX-naïve or whose disease was refractory to DMARDs), and employ different doses of MTX (from 10 to 25mg/week). In general, the RCT found MTX to be effective in peripheral arthritis in PsA over the short (4 months) and the medium term (12 months).13–18
On the other hand, with respect to the observational studies, as occurs with the RCT, there is a wide heterogeneity in the patient profile and in the variables analyzed. They also observed that MTX can be effective in peripheral involvement,19–28 over the short and the long term (2–5 years).29–31
What Should Be the Initial Dose of Methotrexate in Patients With Psoriatic Arthritis?Recommendation 2. An initial dose of MTX not lower than 10–15mg/week is recommended, and this should be determined on the basis of the severity of the disease and prognostic factors related to the patient (LOE, 5; GOR, C; LOA, 100%).
We found no articles that specifically compare initial doses. Generally, in the studies retrieved, treatment begins with low doses that are increased by 2.5mg/week, depending on the clinical response. There are minimum initial doses starting at 5mg/week17,32 to up to 15mg/week.15,22 Other studies manage MTX according to routine clinical practice without really specifying what the dose is and the exact criterion on the basis of which it is modified. Some articles indicate that the authors follow the same guidelines as in rheumatoid arthritis (RA).21,33,34
On the other hand, the panel considers that a number of factors must be taken into account when selecting the initial dose of MTX, such as disease activity and severity (of any of its manifestations). Expert rheumatologists who signed the EULAR consensus document considered, on the basis of the evidence and their experience, that the following are factors of a poor prognosis in PsA: elevated number of active joints (≥5 tender and/or swollen joints); radiographic damage (joint destruction), especially if there is also inflammation; elevated acute-phase reactants and the presence of extra-articular manifestations, especially dactylitis.7 However, it is necessary to take into account patient age, renal function and the possible comorbidities that can accompany the patient with PsA, such as metabolic syndrome or fatty liver.35
Thus, on the basis of these factors, the recommendation leaves a margin for the initial dose of between 10 and 15mg/week.
What Is the Maximum Dose of Methotrexate to Be Administered in Psoriatic Arthritis and How Is Escalation Carried out?Recommendation 3. Once the initial dose of MTX is established, if it does not achieve an adequate response, it is necessary to proceed to a rapid increment of the dose to reach 25–30mg/week over a period of about 8 weeks (LOE, 5; GOR, C; LOA, 100%).
We found no articles that specifically compare maximum doses, with maximum doses of up to 35mg/week reported in the literature reviewed.36 The majority of the studies (RCT and observational studies) have a maximum (per protocol) of 25mg/week.22,37–39 With respect to escalation, it is usually done in intervals of 2.5mg/week, depending on the clinical response.18,36 There are descriptions of other possibilities like incrementing the dose in intervals of 10mg/week.17
It is important to remember that, in the technical specification of MTX in the indication for RA, up to 30mg/week is permitted. On the other hand, if the initial dose does not achieve the adequate response, the panel recommends a rapid escalation over a period of time of approximately 8 weeks. This should be taken as a reference, since the escalation must be adjusted to the characteristics of the patient.
We now have access to documents and treatment strategies like the treat-to-target (T2T) approach and Tight Control of Psoriatic Arthritis (TICOPA), which assist us when it comes to establishing the therapeutic objectives and evaluation of PsA patients.7,40
Again, we must keep in mind the possible comorbidities or patient factors that can affect the escalation and maximum dose, like renal function and patient age. We must also remember that, during dose escalation, systematic evaluations should be carried out to monitor the patient.
Which Is the Route of Administration of Choice for Methotrexate in Psoriatic Arthritis?Recommendation 4. It is recommended that MTX administration be initiated via the oral route; however, the use of the parenteral route should be evaluated in patients with high disease activity, those who require doses of MTX >15mg/week or comply poorly with oral medication, those taking multiple drugs, obese individuals and in the prevention of dosage errors, always taking into account the preferences of the patient (LOE, 5; GOR, C; LOA, 100%).
The majority of the studies included do not specify the route of administration of MTX, although it can be assumed that in most of the patients the oral route was employed. Some of them use the parenteral route,19 but none of them compare the two administration routes. With these limitations, in terms of efficacy and safety, it is not possible to determine whether either of the routes is better than the other in PsA patients.
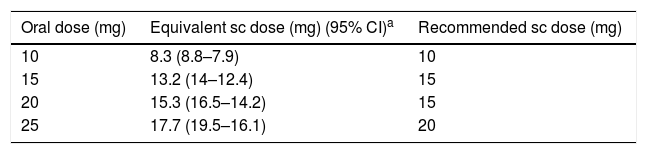
Recently, on the basis of a study on bioavailability (pharmacokinetics),41 a table for dose conversion has been proposed (Table 3), and is the one recommended by the panel.
Bioequivalence of Methotrexate.
| Oral dose (mg) | Equivalent sc dose (mg) (95% CI)a | Recommended sc dose (mg) |
|---|---|---|
| 10 | 8.3 (8.8–7.9) | 10 |
| 15 | 13.2 (14–12.4) | 15 |
| 20 | 15.3 (16.5–14.2) | 15 |
| 25 | 17.7 (19.5–16.1) | 20 |
CI, confidence interval; mg, milligram; sc, subcutaneous.
Recommendation 5. Once the therapeutic goal has been achieved and maintained for at least 6 months, an adjustment of the dose can be evaluated to achieve the minimum dose that maintains said objective (LOE, 5; GOR, D; LOA, 90%).
Different mean maintenance doses have been reported that suggest that these doses achieve the therapeutic objective with no relevant adverse events. In the articles included in this SLR, the mean doses employed varied between 10 and 20mg/week,20,31,33,38,39,42 regardless of whether MTX was utilized as monotherapy or associated, for example, with an anti-tumor necrosis factor-α (TNF-α) agent.
We should remember that changes in the MTX dose must be closely monitored.
In Patients With Psoriatic Arthritis, What Is the Efficacy of Methotrexate on Peripheral Psoriatic Arthritis?Recommendation 6. Methotrexate is effective in the treatment of peripheral psoriatic arthritis (LOE, 1b; GOR, A; LOA, 100%).
In general, RCT (of variable quality) have demonstrated that MTX is effective in peripheral arthritis in PsA patients both over the short term (4 months) and the medium term (12 months), utilizing individual measures and composite indices as efficacy variables.13–18 Although many of these studies are correctly designed, some have certain limitations such as small sample sizes, baseline differences in the characteristics of the patients in the distinct treatment arms or missing data.15,40 In the observational studies, as in RCT, MTX can be effective in peripheral involvement,19–28 both over the short term and the long term (2–5 years).29–31 The experts who signed the EULAR consensus on PsA also took into account the limitations of the literature, but, likewise, evaluated the prolonged survival of MTX in many cohorts, as well as the percentage of patients who achieve minimum activity with MTX as monotherapy. With all this, it is considered the treatment of choice for the management of peripheral arthritis in PsA patients.7
In Patients With Psoriatic Arthritis, What Efficacy Does Methotrexate Have on Axial Involvement, Enthesitis and Dactylitis?Recommendation 7. In those patients with enthesitis and/or dactylitis in the setting of peripheral arthritis it would be possible to evaluate treatment with MTX (LOE, 2a; GOR, B; LOA, 100%).
We have good quality evidence from 3 RCT. In the first,15 the authors evaluated the use of MTX as monotherapy vs the combination of infliximab and MTX. In the two groups, both dactylitis and enthesitis had a statistically significant improvement with respect to their baseline state. In another open-label RCT, at 12 weeks, 25.7% of the patients taking MTX achieved complete remission of enthesitis and 63% of dactylitis. We included a RCT with a duration of 54 weeks,43 in which it was observed that the efficacy of golimumab (GLM) was somewhat superior if it was associated with MTX with regard to dactylitis and enthesitis, although the measures employed were not specified.
The observational studies produced similar outcomes. In a cohort study with a 6-month duration, the authors found that the percentage of patients with dactylitis and enthesitis declined with the use of MTX.26
In terms of axial involvement, there is very little evidence. An observational study44 compared adalimumab (ADA) and the combination of ADA and MTX. The patients were classified on the basis of whether or not they had axial PsA. The addition of MTX did not improve the outcome of the group receiving ADA as monotherapy, regardless of whether or not they had axial involvement. On the other hand, evidence concerning ankylosing spondylitis shows that MTX is not really effective in axial involvement.45
The EULAR consensus on PsA recommends the use of biological therapies in patients with axial involvement that is refractory to nonsteroidal anti-inflammatory drugs (NSAIDs).7
Finally, in this respect, it should be remembered that MTX does not rule out local corticosteroid injection, for example, in those patients with enthesitis or dactylitis who require it.
In patients with psoriatic arthritis, what efficacy does methotrexate have in uveitis?
We found no articles on the systematic review of the use of MTX in uveitis. Therefore, the panel of experts did not issue any recommendation. Reports have been published involving small series of cases.46
In patients with psoriatic arthritis, what impact does methotrexate have on the progression of the disease (peripheral, axial and others)?
In view of the experience of the expert panel, and taking into account the data (at times, contradictory) obtained in the systematic review, it was decided not to issue any recommendation concerning this question. The EULAR consensus on PsA also calls attention to the lack of clear evidence on the efficacy of MTX on radiographic progression.7
At least 7 studies, both RCT and their extensions and observational studies (of up to 5 years of duration), evaluated radiographic progression in PsA patients. They analyzed it basically on the peripheral level.
An open-label RCT47 found that the association of MTX and ADA at week 48 did not add to efficacy in terms of radiographic progression; although the combination appeared to be more effective than ADA as monotherapy, this difference was not statistically significant. In another RCT,43 the changes between the baseline visit and week 24 demonstrated progression with MTX (mean dose of 15mg/week), but not with the combination of GLM at 50mg/week+MTX or with GLM at 100mg/week+MTX. The results in week 52 and during the extension phase (5years),48 were similar. On the other hand, a good-quality RCT49 showed that MTX (up to 25mg/week) associated with infliximab made a positive contribution in that it inhibited radiographic progression in week 54.
In relation to observational studies, one conducted in 201342 demonstrated that, after a year of treatment with MTX, the formation of syndesmophytes had not been inhibited. In another retrospective observational study,20 which included PsA patients taking MTX (mean dose 16.2mg/week) for up to 2 years, it was not possible to arrest radiographic progression (in this report, up to 30% of the patients were receiving another DMARD).
In Patients With Psoriatic Arthritis, Is Treatment With Methotrexate in Combination With Another Disease-modifying Antirheumatic Drug (Leflunomide, Sulfasalazine, Cyclosporine or Others) More Effective Than Methotrexate as Monotherapy?Taking into account expert opinion and the data obtained from the systematic review, it was decided not to issue any recommendation concerning this question.
In a RCT50 involving patients with an incomplete response to MTX, the authors compared its combination with cyclosporine A (CsA) with MTX monotherapy. The CsA+MTX group obtained better results than MTX monotherapy in the swollen joint count and in ultrasound detection of synovitis, but there were no differences in pain or in quality of life; however, there was an increase in the number of adverse events. In a small observational study of PsA patients who had active disease, despite treatment with MTX, leflunomide was added. This achieved a significant improvement in swollen and tender joint counts, Disease Activity Score in 28 joints, acute-phase reactants and in the status of the patients.51
Although an explicit recommendation has not been issued, the panel considers that the clinician should evaluate each patient individually in those situations in which it is appropriate, carry out a risk/benefit evaluation and, on these bases, decide whether or not it is advisable to administer MTX in combination with other DMARDs.
In Patients With Psoriatic Arthritis and an Unsatisfactory Response to Methotrexate, in Those in Whom Biological Therapy Is Indicated, Should Methotrexate Be Maintained? Moreover, in Patients With Psoriatic Arthritis, does Methotrexate Combined With a Biological Therapy Prolong the Survival of the Biological Therapy?Recommendation 8. In patients in whom biological therapy is indicated, the decision whether or not to maintain MTX should be evaluated individually. (LOE 1b; GOR A; LOA 100%).
In the RCT analyzed (over the short and medium term), it seems that the concomitant use of MTX would assure greater efficacy in absolute numbers, but without reaching statistical significance; in other reports, greater efficacy was not observed.2,13,14,37,38,47,52,53
Of the observational studies, only one44 found that the association of MTX would contribute to achieving a significant improvement in joint symptoms and in the Target Lesion Score at 24 months. The remaining studies observed no differences between biological therapy as monotherapy or associated with MTX.30,48,54
On the other hand, we have access to the survival of biological agents associated with MTX. The majority were reported in observational studies, like postmarketing registries of biological drugs. In an analysis of the DANBIO registry,55 the use of MTX was associated with a longer survival of the biological therapy and, in another analysis34 of the DANBIO and ICEBIO registries, the results were similar.
Another observational study56 on the survival of anti-TNFα at 1 year, found that the use of concomitant MTX significantly improved the survival rates of the drug. Again, another report54 observed an association between the concomitant use of MTX and a lower number of dropouts, especially due to a reduction in adverse events.
The panel took very much into account these data on survival of biological therapies (mainly of the monoclonal antibodies, especially chimeric antibodies) on issuing the recommendation.
Does the risk of adverse events of patients with psoriatic arthritis differ from that of other diseases because they are treated with methotrexate?Recommendation 9. There is no evidence that MTX in PsA introduces special safety problems (LOE, 1b; GOR, A; LOA, 100%).
Safety with the use of MTX has been evaluated in different patient profiles (MTX-naïve, those whose disease is refractory to DMARDs, etc.), with distinct MTX doses and criteria, as well as in short-term and long-term studies. The majority of the information came from observational studies.
In RCT,40 the adverse events observed were the same as those reported in other diseases, like RA. Even in the case of association with anti-TNFα, no clear increase in these events has been found,37 but there was a decrease in anti-drug antibodies.38,48
A cross-sectional study33 employed the Methotrexate Intolerance Severity Score to measure toxicity and observed that MTX especially provokes gastrointestinal intolerance. Another observational study21 found that 55.5% of the patients taking MTX developed some type of toxicity, and that 36.7% discontinued the treatment. In a retrospective study57 that examined liver biopsy specimens from PsA patients taking MTX, there was no relationship between the aspartate transaminase levels, the weekly MTX dose, the cumulative dose of the drug and pathological findings. In relation to biological therapies, in one study,54 the authors observed that the incidence of adverse events (approximately 5%–6% per year), was similar in the group of patients treated with anti-TNFα, whether or not it was associated with MTX,
Again, we wish to stress that we have access to documents that indicate how to prevent and monitor the safety of patients being treater with DMARDs, both synthetic and biological.
What the Mean Time Between the Interruption of Methotrexate and a New Flare?Based on their experience and on the lack of evidence in the systematic review, the panel of experts decided not to issue any recommendation.
In an observational study performed in 2000,58 after 4 to 6 months of treatment with MTX (at a dose of 15–20mg/week), the attempt was made to replace MTX with a NSAID or corticosteroids. The symptoms could be controlled in only 35% of the patients and, over the long term, the majority of the patients again required MTX.
DiscussionIn the present report, we offer a series of recommendations on the use of MTX in PsA patients, based on the best available evidence. For this purpose, we followed the nominal group and Delphi method, which are widely utilized in documents of this type.7,10,11 We selected a group of prestigious Spanish experts, who had the support of a systematic review and the help of an expert methodologist.
Methotrexate is a standard drug in the treatment of many rheumatic diseases, with RA as the paradigmatic disease in relation to its use. In fact, it is in regard to this disease where the main body of the evidence is encountered.10,11
On the other hand, PsA is a highly complex disease and there is less available evidence on the use of MTX as compared to RA. However, there are certain aspects that appear to be widely accepted in the management of these patients. Once the diagnosis is established, the indication of MTX as the first-line treatment (patients whose disease is refractory to NSAIDs and corticosteroids or those who directly have factors associated with a poor prognosis) is clearly defined, as EULAR properly recommends.7 Moreover, it is especially suitable for patients with skin involvement.
Although the indication of MTX appears to be clear, there is still a wide variability in clinical practice in Spain with respect to the initial dose, the criteria for the escalation of that dose and the choice of the administration route in PsA patients.9 Thus, we carried out a comprehensive SLR, that was taken very much into account on formulating the recommendations issued in the present document.
Although the search strategy and review of the gray literature were extensive, the major limitation of the recommendations is the difficulty in establishing robust or highly specific recommendations, given that there is a great variability in the profiles of patients included in the studies, as well as the type of outcome variables analyzed. However, MTX is a drug that has been utilized for several decades in rheumatology, meaning that there is a great deal of clinical experience with its use. Moreover, in the present document, the experts agreed thoroughly with the formulation of the recommendations. Another important limitation is that there are very few high-quality RCT.
On the other hand, there are still questions to be resolved in the use of MTX in PsA. One of the most important is the dosage (initial, maximum and escalation of the dose and its optimization). Currently, we follow the recommendations established for RA. We also need studies that evaluate the efficacy of MTX in certain extra-articular manifestations like uveitis, its real effect on radiographic progression and its possible role in relation to the immunogenicity generated with drugs like the anti-TNFα agents.
In short, with the objective of improving clinical practice, it is essential to have access to explicit recommendations that encompass aspects like dosage and the safety of MTX in PsA. Although the evidence is still limited in many areas, this document presents a series of recommendations that we trust will be relevant and helpful to clinicians. Moreover, we refer to routine aspects related to its use, which means that the recommendations can be implemented in daily practice without difficulties. The panel is convinced that applying them will improve the management of the patients and, thus, their prognosis.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThe project was financed by Gebro Pharma, which did not intervene in the design of the project or in drafting the recommendations.
Conflict of InterestThe authors received economic compensation from Gebro Pharma for the services they provided in the development of the project.
Please cite this article as: Cañete JD, Ariza-Ariza R, Bustabad S, Delgado C, Fernández-Carballido C, García Llorente JF, et al. Recomendaciones sobre el uso de metotrexato en pacientes con artritis psoriásica. Reumatología Clínica. 2018;14:183–190.