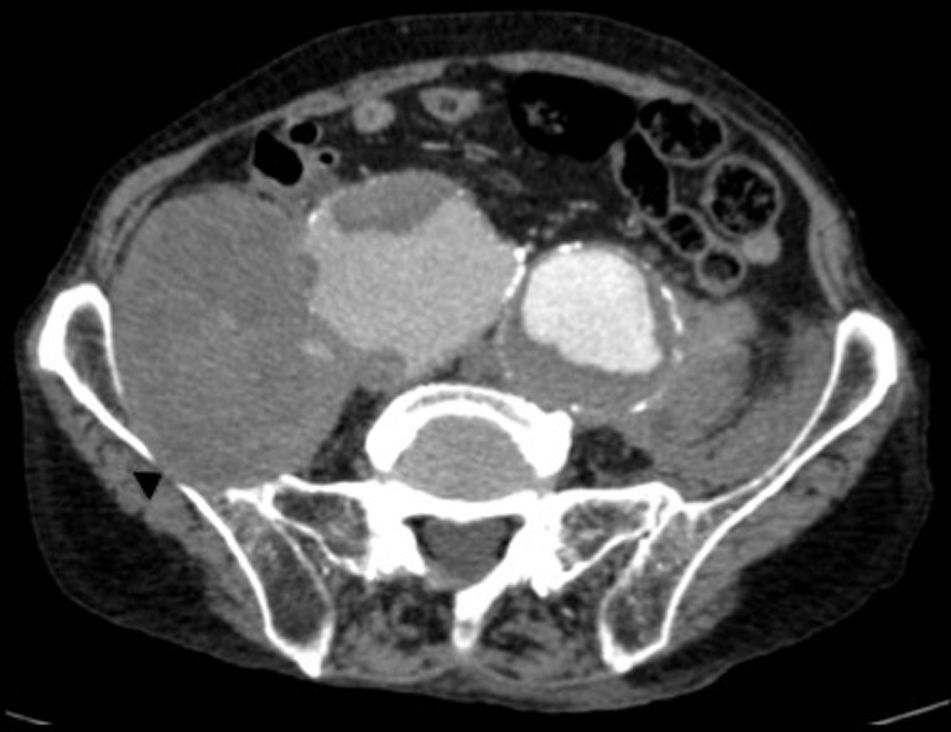
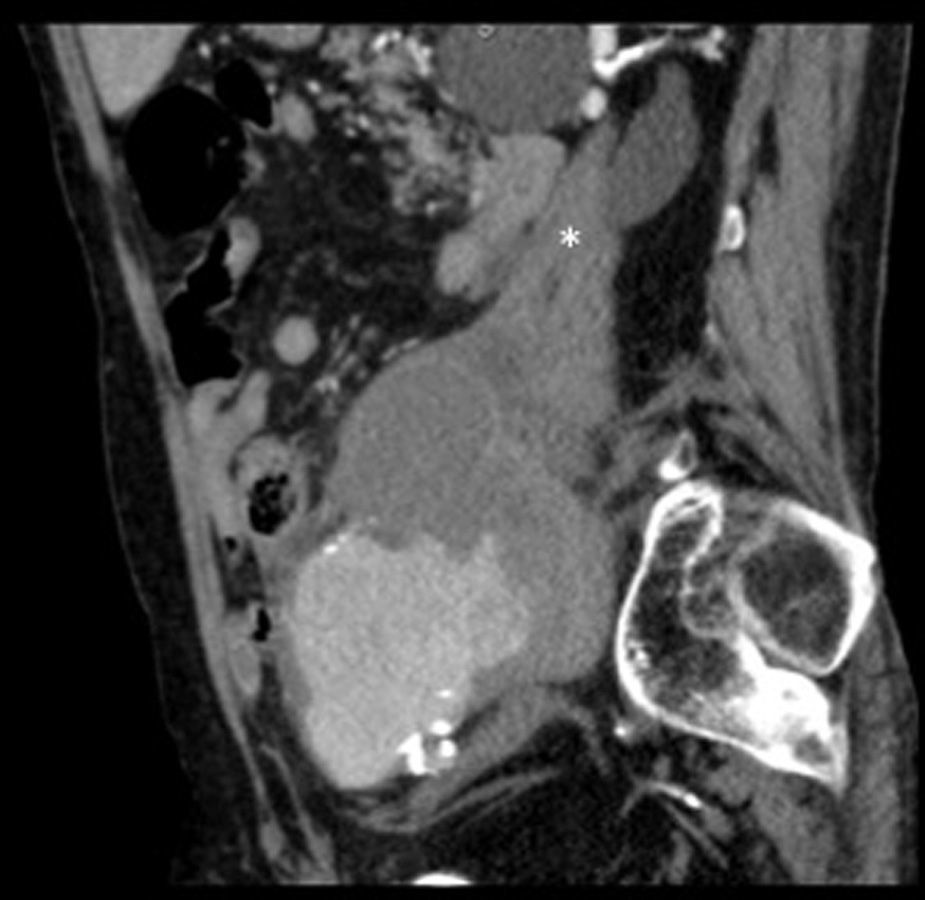
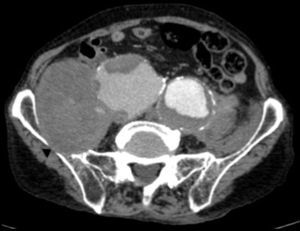
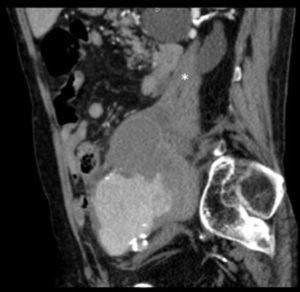
The patient was an 86-year-old man who was taking 2 medications for hypertension. He had a history of several months of low back pain that radiated to right thigh, for which symptomatic treatment provided partial relief. His rheumatologist had ordered thoracolumbar magnetic resonance imaging (MRI), but it was not performed because, prior to the scheduled date, the patient went to the emergency department with an increase in the intensity of the pain. Laboratory analyses showed a hemoglobin level of 8.4g/dL, lactate dehydrogenase of 318U/L, creatinine of 1.29mg/dL, C-reactive protein of 6.16mg/dL, erythrocyte sediment rate of 24mm/h and mild hypoproteinemia. There was no evidence of hemodynamic instability. He underwent abdominopelvic computed tomography (CT) with intravenous contrast, which revealed isolated bilateral iliac aneurysms>6cm (Fig. 1) with contained rupture of the aneurysm on the right (Fig. 2), which displaced the psoas muscle (Fig. 3) and perforated the ipsilateral iliac bone (Fig. 4). The patient underwent aortobifemoral bypass but, unfortunately, he died during the postoperative period.
Isolated iliac aneurysms, without an associated aortic aneurysm, are rare.1 They are relatively difficult to identify, as up to 40% of them may present with rupture.2 The incidence rate of extraspinal causes of sciatica is low.3 Likewise, chronic rupture of an aneurysm constitutes a peculiar entity. All these circumstances coming together result, in most cases, in an erroneous or late diagnosis.4 It is usually a dorsolateral rupture toward the anterior insertions of the psoas muscle, which contains the hematoma, avoiding massive extravasation, but not the infiltration of the roots of the lumbosacral plexus. This produces chronic low back pain that radiates to the lower limb,5 this being the most common presentation.6 The diagnosis can be based on abdominal CT,7 and lumbar MRI (parasagittal slices).7,8 The aneurysm may undergo secondary acute rupture at any time.4 This case serves to remind us, in our routine practice, that an aneurysm may be involved in the symptoms of sciatica.9
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Alonso-Gómez N, González-Gutiérrez A, Molina López-Nava P, Sáinz-González F. Rotura crónica contenida de aneurisma ilíaco simulando ciática. Reumatol Clin. 2016;12:294–295.