The patient was a 68-year-old man with a personal history of Forestier-Rotés Querol disease, hypertension, type II diabetes mellitus, hepatic steatosis and Haglund's disease in right foot. He reported a worsening of the clinical signs and symptoms in cervical spine over the preceding year, with continuous pain and progressive limitation for movements from side to side, and no evidence of radiculopathy or myelopathy. He also complained of dysphagia with solid food and, to a lesser extent, with liquids, and had lost 15kg over the preceding year.
The involvement of cervical spine in this disease and the development of dysphagia has been documented previously. However, the purpose of presenting this case report is to show the radiological progression over a 5-year period in the same patient and its clinical impact.
The radiographic changes in Forestier-Rotés Querol disease were described by Resnick in 1975.1 These criteria include the ossification of the anterior longitudinal ligament along the anterolateral surface of at least 4 contiguous vertebral bodies, the preservation of disc height, the absence of the vacuum phenomenon or marginal sclerosis in the vertebral bodies and the absence of ankylosis of the facet joints or changes in the sacroiliac joints.1
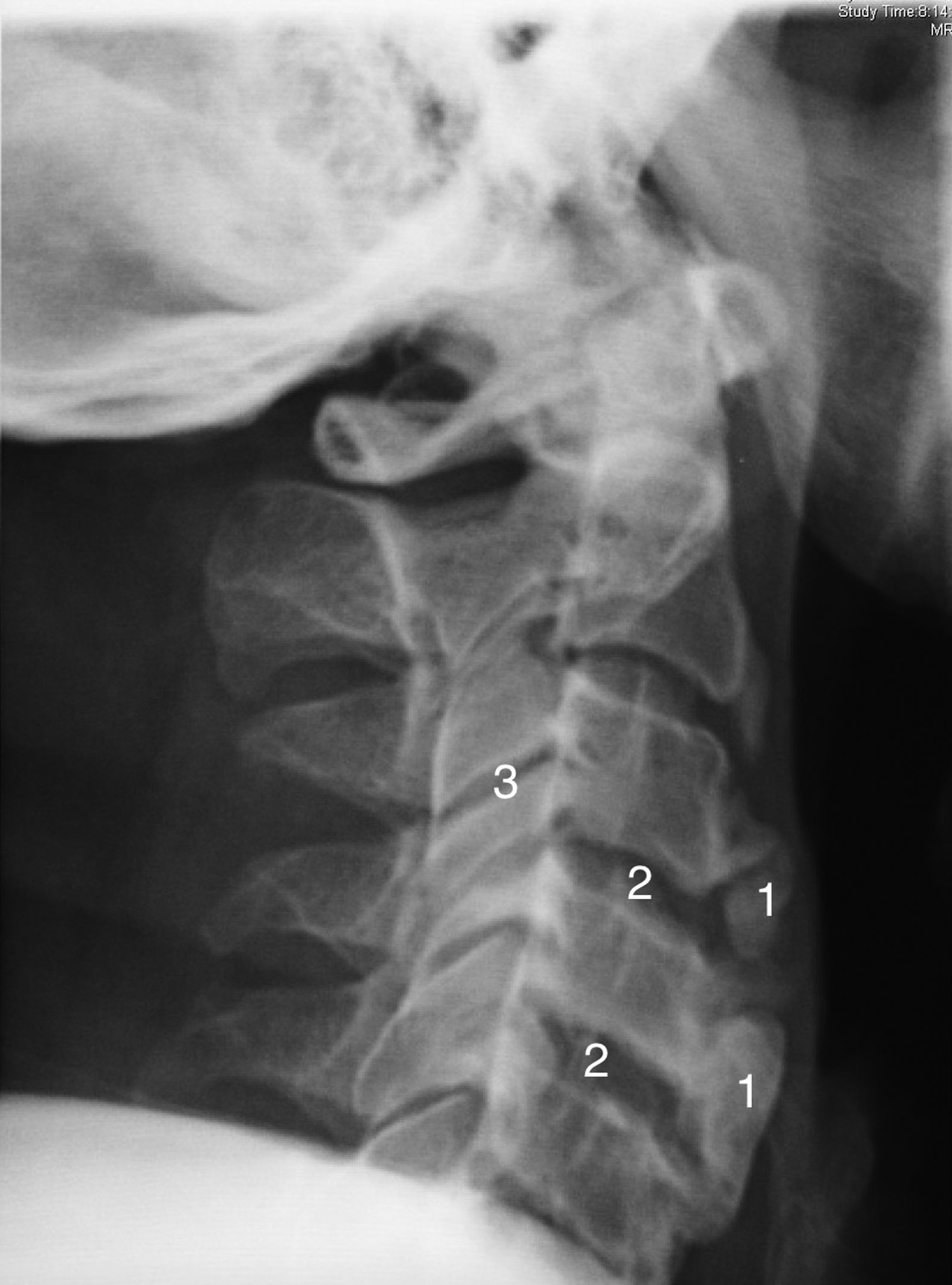
The assessment of the radiological changes in the cervical spine of this patient over a 5-year period revealed an increase in osteophyte size and in the ossification of anterior cervical ligament, which affected several contiguous vertebrae (Figs. 1 and 2). This could explain an extrinsic cause of the dysphagia. There are other radiological features of interest, such as the relative preservation of the intervertebral disc space and the absence of involvement of the facet joints.
Radiography of lateral cervical spine (2014) showing an increase in the extent of ossification of anterior cervical ligament with overall involvement of the cervical spine (1), and a protuberance (*) toward the aerodigestive tract. A relative conservation of the height of the intervertebral disc space is also observed (2).
Given the systemic signs, the patient underwent gastroscopy and upper gastrointestinal series, the results of which were normal.
Computed tomography of the cervical spine revealed ossification of anterior longitudinal ligament and anterior osteophytes, with involvement basically in the upper cervical spine (C2–C4), which made forward motion of the aerodigestive tract more difficult. There was no evidence of involvement of the facet joints.
In conclusion, dysphagia is a relatively common manifestation when the cervical anterior longitudinal ligament is affected.2,3 In the differential diagnosis, it is necessary to rule out both an intrinsic and an extrinsic component, since the most frequent causes of dysphagia continue to be tumors.2 For treatment, a conservative approach should be adopted (analgesia, rehabilitation, suitable nutritional intake and monitoring for metabolic syndrome, which is closely related to Forestier disease)4–7 and, in more serious cases, the compression produced by the osteophytes may require surgical intervention.3,4 However, there is a high percentage of recurrences following surgery.8
Ethical DisclosuresProtection of human and animal subjectsThe author declares that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe author declares that she has followed the protocols of her work center on the publication of patient data and that all the patients included in the study have been properly informed and have given their written consent to participate in said study.
Right to privacy and informed consentThe author has obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe author declares that she has no conflicts of interest.
Please cite this article as: García García M. Enfermedad de Forestier-Rotés Querol: progresión radiológica cervical y aparición de disfagia. Reumatol Clin. 2016;12:292–293.