SAPHO syndrome was proposed in the late 80s in order to group different osteoarticular manifestations with specific radiological findings such as the hyperostosis of the front part of the chest wall. Prevalence, etiology and pathogenesis of the disease are unknown, while diagnosis is made both clinically and by the specific gammagraphic image of “bull horn” in the sternoclavicular joint.
The following case of a 64-year-old woman diagnosed with infiltrating ductal carcinoma of the right breast pT1N0 Mx is reported. When studying the extent of the disease, a gammagraphic image of diffuse blast injury in the sterna manubrium was evidenced, which allowed the suspicion of Paget's disease or metastatic injury. Study was completed with a chest CT in which manubrium sclerosis was evidenced, suggesting metástasis.
Results of the studies pointed out SAPHO syndrome as the most likely diagnostic option. The low tumor stage of the patient prompted the idea of possible alternative diagnoses. A deeper knowledge of this clinical condition may be crucial to avoid mistakes when classifying a subject in more advanced tumor stages, and consequently, to prevent the use of more aggressive chemotherapy and radiotherapy treatments.
El síndrome de SAPHO fue propuesto a finales de los años 80 para agrupar diversas manifestaciones osteoarticulares con hallazgos radiológicos propios como la hiperostosis de la pared anterior del tórax. La prevalencia, la causa y la patogénesis de la enfermedad son desconocidas. El diagnóstico se realiza tanto por la clínica como por la imagen específica gammagráfica de «asta de toro» en la articulación esternoclavicular.
Se presenta el caso de una mujer de 64 años diagnosticada de carcinoma ductal infiltrante de mama derecha pT1N0 Mx. En el estudio de extensión de la enfermedad se evidenció imagen gammagráfica de lesión blástica, difusa, en manubrio esternal, sospechosa de enfermedad de Paget o lesión metastásica. Se completó el estudio con TC torácica en la que se evidenció esclerosis del manubrio esternal, sugerente de metástasis.
Por el resultado de los estudios se pensó en el síndrome de SAPHO como opción diagnóstica más probable. El bajo estadio tumoral de la paciente hizo pensar en posibles alternativas diagnósticas. Conocer esta entidad clínica puede evitar errores a la hora de clasificar en estadios tumorales más avanzados a un sujeto y, por tanto, evitar tratamientos quimioterápicos y radioterápico más agresivos.
SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis and osteitis)1 was proposed toward the end of the 1980s by Chamot et al.2 to group a number of osteoarticular manifestations with common radiological features, like hyperostosis of anterior chest wall. These signs are often, although not necessarily, associated with dermatological conditions such as acne conglobata, palmoplantar pustulosis and/or psoriasis. The presence of the bone lesions may be unrelated to the development of the skin lesions. The cause of SAPHO syndrome is unknown, although different theories propose the presence of a certain genetic predisposition, infectious causes and the association of immune disorders.3 The prevalence is unknown, although some authors report that it is 1 per 10,000 population in Caucasians and lower in Asian populations.4 The diagnosis is based mainly on the clinical signs, indicated by the presence of at least one of the inclusion criteria and none of the exclusion criteria, as described by Benhamou et al.5 The study includes ancillary diagnostic tests such as the specific bone scintigraphic image6 of the “bull's head” sign in the sternoclavicular joint. The laboratory findings are also nonspecific, with the exception of an increase in acute-phase reactants.7 The disease prognosis is usually benign, although, in certain cases, the pain produced by joint inflammation can be quite severe.8 The treatment of this condition includes nonsteroidal anti-inflammatory drugs, intravenous bisphosphonates or biological therapies.3 The response to a treatment is assessed in terms of pain relief, according to the visual analog scale, or using imaging techniques like bone scintigraphy (BS), computed tomography (CT) or positron emission tomography with CT (PET-CT).9,10
Case ReportWe present the case of a 64-year-old woman who was diagnosed with stage T1cN0 Mx invasive ductal carcinoma of right breast. After undergoing segmental mastectomy of right breast and selective biopsy of the sentinel lymph node, she was referred to our department by the Breast Disease Committee to receive adjuvant radiation therapy. The patient had a history of hypertension, dyslipidemia and intermittent low back pain, that she had had since her youth and associated with her job as a salesclerk. She had had no previous visits to any specialist and did not require medication on a regular basis.
In the physical examination, there was no evidence of infection or inflammation of the mastectomy scar. However, the third proximal to the clavicle was enlarged and the patient perceived mild selective pain on palpation of the sternoclavicular joint. On examination of the abdomen, no masses or enlargement of organs was detected. The patient reported that she had never had clinical signs of skin conditions (palmoplantar pustulosis or acne).
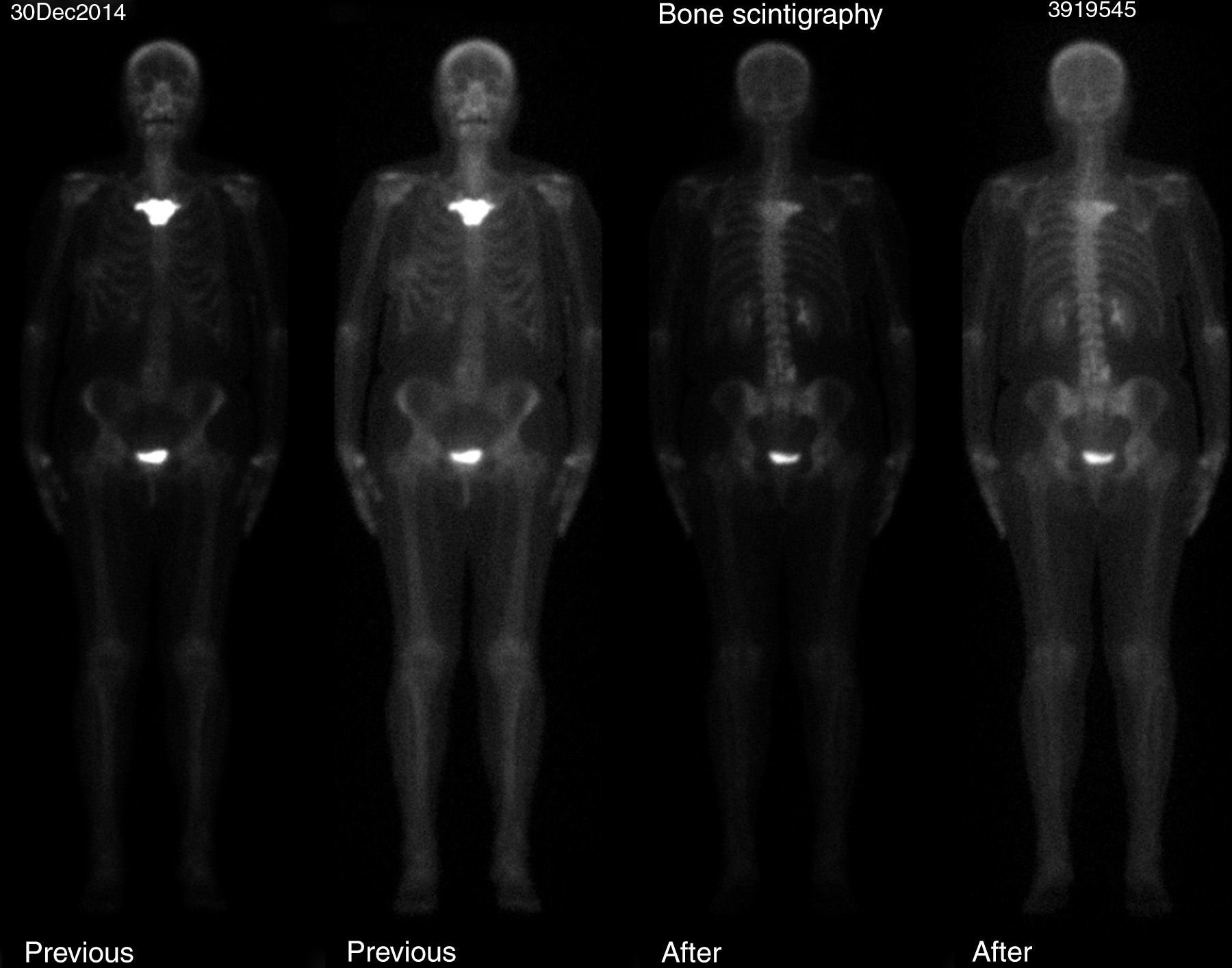
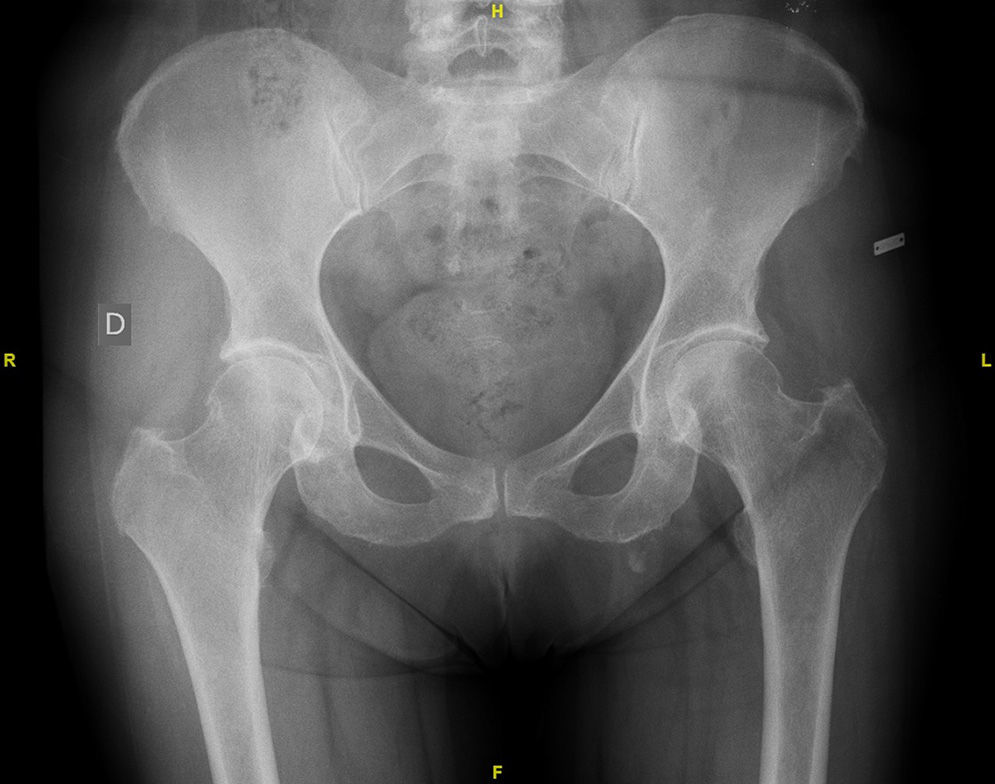
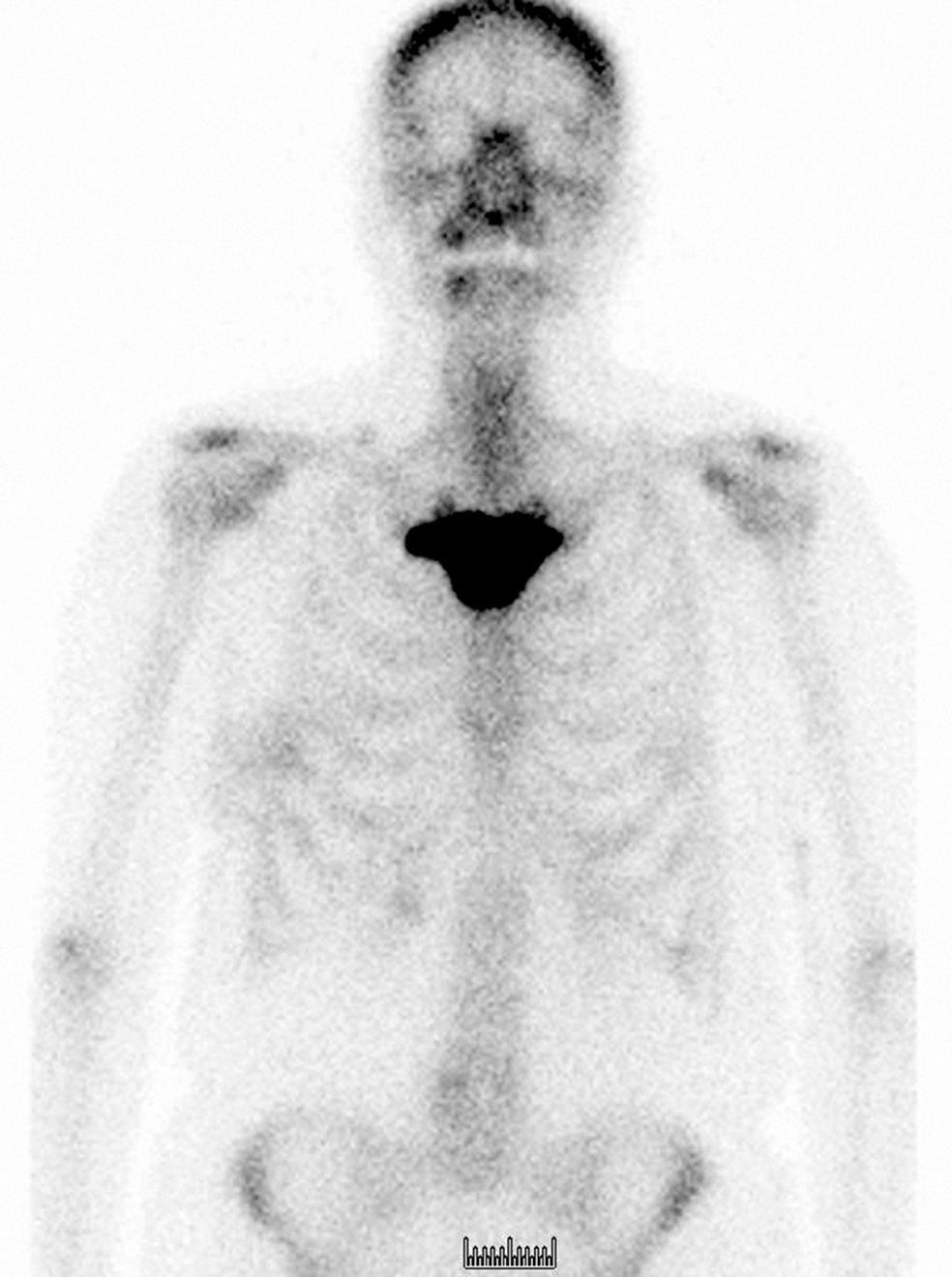
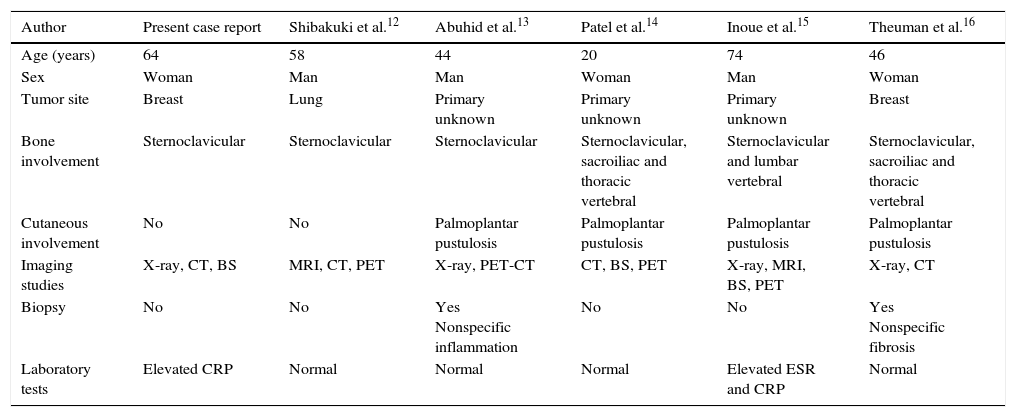
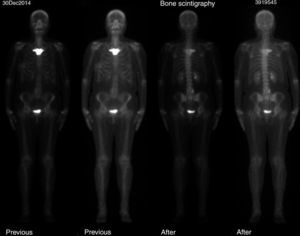
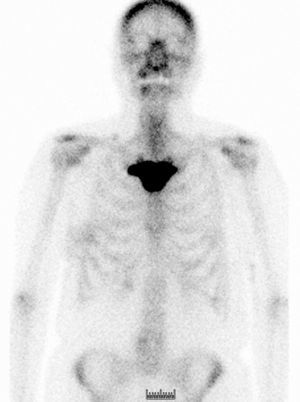
The study of the extension of the disease included BS, which revealed the presence of a diffuse blastic lesion in the sternal manubrium, suggestive of Paget's disease or a metastatic lesion (Fig. 1). The study was completed with radiographs of chest, lumbosacral spine and pelvis (Figs. 2 and 3), in which the only finding was increased density in L4-L5 facet joints. Chest CT, recommended by the professionals in nuclear medicine, revealed sclerosis in the sternal manubrium, suggestive of metastasis (Fig. 4).
Laboratory findings included normal values for alkaline phosphatase (95IU/L), calcium (9.57mg/dL), lactate dehydrogenase (161IU/L) and erythrocyte sedimentation rate (6mm). Only a slight increase in C-reactive protein (0.60mg/dL) was observed. A test for HLA-B27 was not requested because of the negative results in the laboratory tests and the limited relationship to SAPHO syndrome reported in some case series.9
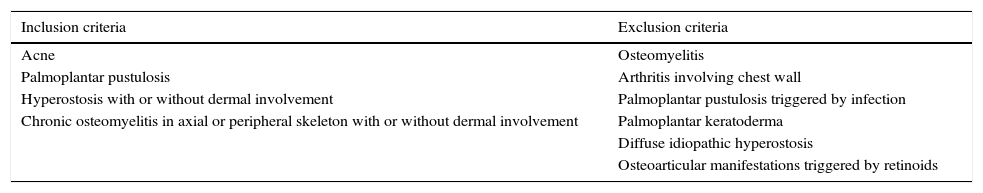
Given the difficulty of the case, a clinical discussion session was held, with the participation of the departments of radiation oncology, rheumatology, radiodiagnostics and nuclear medicine, to review the findings. The outcome was a definitive diagnosis of SAPHO syndrome, as the patient met one of the inclusion criteria described by Benhamou et al.,5 hyperostosis of anterior chest wall, with or without dermal involvement, and none of the exclusion criteria (Table 1). A biopsy of the lesion was ruled out at that time, pending the radiographic evolution. The decision was made to perform BS and osteoarticular CT11 6 months later, at which time, no noteworthy changes were observed, and a biopsy of the affected area was definitively ruled out, as the images showed no signs of aggressive disease. During treatment, the patient required no analgesic medication of any type. We excluded the affected area from the field of treatment to avoid provoking modifications secondary to the radiotherapy that could lead to confusion when assessing the changes in the lesion. After 18 months of follow-up, the complete response of the tumor persists and the patient is disease-free.
Inclusion and Exclusion Criteria in SAPHO Syndrome.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Acne | Osteomyelitis |
| Palmoplantar pustulosis | Arthritis involving chest wall |
| Hyperostosis with or without dermal involvement | Palmoplantar pustulosis triggered by infection |
| Chronic osteomyelitis in axial or peripheral skeleton with or without dermal involvement | Palmoplantar keratoderma |
| Diffuse idiopathic hyperostosis | |
| Osteoarticular manifestations triggered by retinoids |
Source: modification of Benhamou et al.5
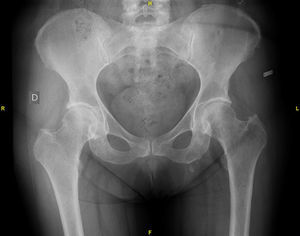
SAPHO syndrome is a rare clinical condition of benign nature that usually presents in young individuals, a circumstance that makes it difficult to detect complications in the patients with this disease. The problem arises when it is diagnosed in a cancer patient, as none of the imaging techniques help to definitively rule out metastasis.11 In the literature (Table 2),12–16 there are few cases in which SAPHO syndrome was diagnosed on the basis of an image suspected of depicting a metastasis that, after further study, was found to show no evidence of aggressive disease. Of these cases, only one was identified as breast cancer; in addition to the sternoclavicular involvement, there were dermatological signs that could have pointed to the diagnosis. In none of these cases was the biopsy of the region being studied (sternal manubrium) of any help in reaching the definitive diagnosis.
Review of Case Reports With a Diagnosis of SAPHO Syndrome Based on Images Suggestive of Metastasis.
| Author | Present case report | Shibakuki et al.12 | Abuhid et al.13 | Patel et al.14 | Inoue et al.15 | Theuman et al.16 |
|---|---|---|---|---|---|---|
| Age (years) | 64 | 58 | 44 | 20 | 74 | 46 |
| Sex | Woman | Man | Man | Woman | Man | Woman |
| Tumor site | Breast | Lung | Primary unknown | Primary unknown | Primary unknown | Breast |
| Bone involvement | Sternoclavicular | Sternoclavicular | Sternoclavicular | Sternoclavicular, sacroiliac and thoracic vertebral | Sternoclavicular and lumbar vertebral | Sternoclavicular, sacroiliac and thoracic vertebral |
| Cutaneous involvement | No | No | Palmoplantar pustulosis | Palmoplantar pustulosis | Palmoplantar pustulosis | Palmoplantar pustulosis |
| Imaging studies | X-ray, CT, BS | MRI, CT, PET | X-ray, PET-CT | CT, BS, PET | X-ray, MRI, BS, PET | X-ray, CT |
| Biopsy | No | No | Yes Nonspecific inflammation | No | No | Yes Nonspecific fibrosis |
| Laboratory tests | Elevated CRP | Normal | Normal | Normal | Elevated ESR and CRP | Normal |
BS, bone scan; CRP, C-reactive protein; CT, computed tomography; ESR, erythrocyte sedimentation rate; MRI, magnetic resonance imaging; PET, positron emission tomography; SAPHO, synovitis, acne, pustulosis, hyperostosis and osteitis.
In our patient, the stage of her tumor (IA) and the phenotypic characteristics indicated that the result of the study of its extension, which was interpreted as a possible sternal metastasis of the breast carcinoma, could be questioned. Therefore, we considered possible diagnostic alternatives that could explain these findings. Although SAPHO syndrome is a clinical condition with a low incidence, knowledge of it can avoid a diagnosis of metastasis in patients found to have the characteristic image of the “bull's head” on BS. If this image had been seen in a patient with factors indicative of a poor prognosis, we probably would not have questioned the possibility of a metastatic lesion. As a result, the patient would have undergone chemotherapy (vinorelbine or taxanes) and more aggressive radiotherapy, and would have been exposed to the complications associated with these strategies.
ConclusionsSAPHO syndrome has different clinical manifestations that, together with the osteitis that is characteristic of this entity, can result in different differential diagnoses. Thus, this syndrome should be taken into account in the context of the neoplastic disease, in order to avoid erroneous diagnoses that require aggressive treatments in a disease that usually has a benign course.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Berenguer Francés MÁ, Lafaurie Acevedo A, Tormo Ferrero V, Cardenal Macia R, Andreu Martínez FJ. Síndrome de SAPHO como diagnóstico diferencial de metástasis. Reumatol Clin. 2016;12:288–291.