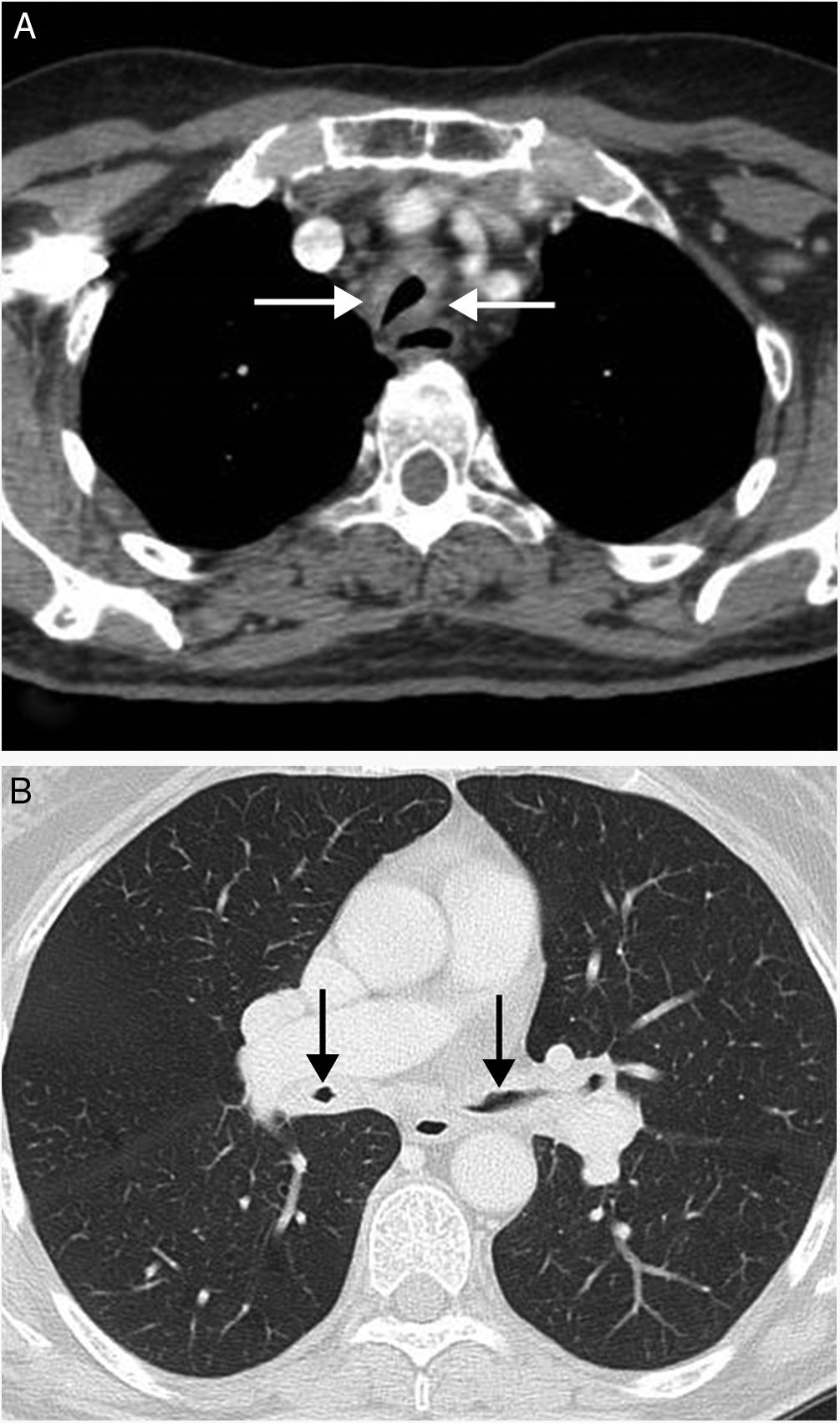
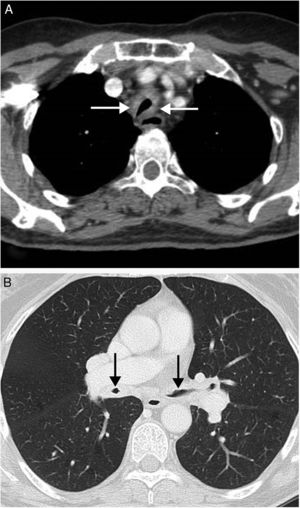
We present the case of a 68-year-old patient, a non smoker, who sought medical attention due to a dry cough of several months onset. During the previous few weeks the patient had presented with intermittent, low-grade fever in the evenings. The patient's medical background only highlighted several episodes of anterior uveitis which responded to topical treatment with glucocorticoids. A chest X-ray did not show any radiologic changes, but computerised tomography (CT) of the chest revealed a noticeable circumferential thickening of the walls of the trachea (respecting the posterior tracheal wall) and the main bronchi which had led to a major reduction in their lumens (Fig. 1). Subsequent to these findings, a diagnosis of relapsing polychondritis (RP) was made, which was confirmed with transbronchial biopsy performed by fibrobronscopy. The latter revealed inflammatory changes to the pericartilaginous structures, thus meeting the Damiani and Levine criteria for the diagnosis of RP.1 Respiratory function tests only showed a slight airflow obstruction. Other rheumatic, endocrine and haematological diseases which may be associated with RP in up to 33% of cases, were ruled out. The patient responded favourably to treatment with glucocorticoids and azathioprine.
(A) CT axial view where a noticeable thickening of the tracheal walls (arrows) may be observed, together with highly significant reduction in their lumens. (B) CT axial view (lung imaging window) where major circumferential thickening of the walls of both main bronchi may also be observed, together with serious reduction in their lumen quality (arrows).
RP is a rare multisystemic disease characterised by recurrent and progressive episodes of inflammation and the destruction of cartilaginous tissue affecting, among other organs, the outer ear, nose and airways. For most patients with RP initial clinical symptoms are usually nasal and/auricular chondritis. Both ocular involvement (in the form of uveitis, scleritis or keratitis) and the involvement of tracheobronchial cartilage are highly uncommon forms of RP presentation, and they remind us that initial atypical manifestations of this disease exist and require differential diagnosis to apparently banal symptoms.2–5
Ethical liabilitiesProtection of people and animalsThe authors declare that for this research no experimentation has been carried out on human beings or animals.
Data confidentialityThe authors declare that they have adhered to the protocol of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Gorospe Sarasúa L, Barrios-Barreto D, Said-Criado I, de la Puente-Bujidos C. Diagnóstico de policondritis recidivante en una paciente con tos crónica y sin condritis nasal ni auricular. Reumatol Clin. 2019;15:e51–e52.